Epileptic spasms (ESs) are a type of epileptic seizure characterized as brief muscle contractions with ictal polyphasic slow waves on an electroencephalogram and a main feature of West syndrome. Resection surgeries, including frontal/posterior disconnections and hemispherotomy, have been established for the treatment of medically intractable ES in patients with unilaterally localized epileptogenic regions. Corpus callosotomy (CC) has been mainly used to treat drop attacks, which are classified as generalized tonic or atonic seizures. However, CC has also been adopted for ES treatment.
1. Introduction
In 1940, van Wagenen and Herren
[1] first introduced the corpus callosotomy (CC) as a surgical treatment option for patients with medically intractable epilepsy and reported the efficacy of preventing the propagation of focal seizures to the contralateral hemisphere. Since then, CC has been applied for the treatment of drop attacks, which were classified into generalized tonic or atonic seizures in the latest classification of seizure types in 2017 by the International League Against Epilepsy (ILAE). However, CC has also been adopted for the treatment of epileptic spasms (ES), as reported by Pinard in 1993
[2], and reports concerning CC for the treatment of patients with ES has increased since 2010
[3][4][5][6][7][8][9][10][11][12][3,4,5,6,7,8,9,10,11,12].
ES are epileptic seizures characterized as brief muscle contractions that typically involve the axial muscles, proximal limb segments, and a main feature of West syndrome
[13]. It has been hypothesized that the epileptogenic cortex triggers the activation of subcortical structures, leading to ES
[14][15][14,15]. Resection surgeries, including cortical resections, frontal/posterior disconnection and subtotal/total hemispherotomy/-rectomy, have been established for the treatment of ES in patients with epileptogenic regions estimated to be located in the unilateral hemisphere
[16][17][18][19][20][16,17,18,19,20]. However, CC has also been a helpful treatment option for patients without apparent lateralized epileptogenic findings on presurgical evaluations.
2. Corpus Callosotomy for Epileptic Spasms
Prior to 2000, there were few reports concerning the use of CC to treat patients with ES
[2][21][22][2,60,61]. Talwar et al. reported three patients aged between 5 and 12 years who had undergone CC surgery, with two of the patients having experienced a marked reduction in ES frequency
[21][60]. In 1999, Pinard et al. reported a case series involving the use of CC to treat patients with ES
[22][61] involving ten patients (age range, 2–9 years) with symptomatic generalized epilepsy presenting with ES, who received one or two stages of total CC. In that case series, CC was found to be insufficiently effective; eight patients developed tonic seizures, with each patient showing asymmetrical spasms and head nodding postoperatively. Between 2000 and 2009, a limited number of studies concerning CC, including some patients with West syndrome, have been reported
[23][24][62,63]; however, its efficacy in treating patients with ES or West syndrome was not elucidated.
Since 2010, the number of studies concerning the use of CC to treat patients with ES has increased. Some studies have not provided particular details concerning the efficacy of CC procedures to treat ES or West syndrome, but have reported whole outcomes including patients with other types of seizures, Lennox-like syndrome, or Lennox-Gastaut syndrome
[25][26][27][28][29][30][64,65,66,67,68,69]. However, in other recent studies, the outcomes of CC to treat ES, which mostly involved patients with West syndrome, have been presented using detailed patient data
[3][4][6][8][9][10][11][31][3,4,6,8,9,10,11,70]. Because of these studies, CC use has been adapted to not only involve treatment for drop attacks (tonic seizures, atonic seizures) and atypical absence and tonic–clonic seizures, but also for patients with ES, and for older patients with Lennox-Gasutaut syndrome and Lennox-like syndrome, as well as infants with West syndrome, regardless of the presence of the sudden falling-down manifestation.
36. Efficacy of Corpus Callosotomy for Epileptic Spasms
3.1. Seizure Outcomes Post-Corpus Callosotomy for Epileptic Spasms
2.1. Seizure Outcomes Post-Corpus Callosotomy for Epileptic Spasms
Although most previous studies regarding the efficacy of CC for drop attacks have not provided data on efficacy, particularly for ES, several studies have described CC outcomes in relation to ES
[3][4][6][8][9][10][11][12][22][31][3,4,6,8,9,10,11,12,61,70] as shown in
Table 1. Seizure-free ratios post-CC ranged from 25% to 79% among the studies. In a relatively large study, Otsuki et al. reported that CC achieved seizure freedom in 7 of 15 patients (54%) with West syndrome and in 7 of 10 (70%) patients with ES
[4]. Baba et al.
[6] reported the efficacy of CC in 56 patients (age range, 5.1–22.6 months old at CC; mean follow-up, 36.6 months) with intractable West syndrome without brain lesions on MRI. Regarding patients with ES, they reported that 43% of these patients who underwent CC achieved seizure freedom, 23% achieved ≥80% seizure reduction, and 13% achieved ≥ 50% seizure reduction at the last follow-up, whereas in patients with tonic seizures, no seizure freedom was observed
[6].
Table 1. Previous studies of corpus callosotomy (CC) for epileptic spasms (ES).
| Authors |
N: CC for ES (Total N of Any Size) |
Age at 1st CC |
Seizure Types (ES and Others) |
MRI Lesion (+/-) |
Procedures of Resection |
| 1 |
Pinard et al. 1999 [23] |
14 (17) |
1.7–14.3 years |
ES only:
36% ES + generalized: 64% |
Unknown |
ACC only: 2 ACC→TCC: 10 PCC→TCC: 2 |
| 2 |
Ono et al. 2011 [3] |
7 (19) |
0.4–3 years |
ES only: 86%
ES + focal + generalized: 14% |
MRI lesion (+): 28%
Bilateral: 28% |
ACC→CR: 14%
ACC→TCC→CR: 14%
TCC→CR: 57% TCC→PQD: 14% |
| 3 |
Otsuki et al. 2016 [4] |
10 (30) |
Unknown |
Unknown |
Unknown |
TCC only: 100% |
| 4 |
Iwasaki et al. 2016 [32] |
8 (26) |
1–14 years |
ES only: 50%
ES + generalized: 50% |
MRI lesion (+): 50%
Unilateral: 13%
Bilateral: 38% |
TCC only: 100% |
| 5 |
Baba et al. 2018 [6] |
56 |
0.4–1.9 years |
ES only: 84%
ES + generalized: 16% |
MRI lesion (+): 0% |
ACC only: 4%
ACC→TCC: 5%
TCC only: 91% |
| 6 |
Baba et al. 2019 [8] |
42 |
0.6–7 years |
ES only: 43%
ES + focal: 7%
ES + generalized: 50% |
MRI lesion (+): 21% |
TCC only: 79%
TCC→AQD/PQD/SHR/HR: 21% |
| 7 |
Okanishi et al. 2019 [9] |
7 |
2.1–21.5 years |
ES only: 29%
ES + focal: 29%
ES + generalized: 43% |
MRI lesion (+): 100% (bilateral tubers only) |
TCC only: 71%
TCC + CR/PQD: 29% |
| 8 |
Kanai et al. 2019 [10]
Oguri et al. 2020 [11]
(Using the same patient data) |
17 |
1.4–19.8 years |
ES only: 18%
ES + others: 82% |
MRI lesion (+): 65% |
ACC only: 18%
TCC only: 82% |
| 9 |
Uda et al. 2021 [12] |
8 (10) |
0.8–9.1 years |
Unknown |
MRI lesion (+): 0% |
TCC only: 63% (5/8)
TCC→AQD/PQD/HR: 37% (3/8) |
| ES outcomes |
Good prognostic factor |
Others |
| 1 |
Seizure free: 79% (after final CC) |
NA |
- |
| 2 |
Seizure free: 71% (TCC + others) |
NA |
This study reported only cases involving additional resection/disconnection. |
| 3 |
Seizure free: 70% |
NA |
Described as part of 67 surgical study cases |
| 4 |
Seizure free: 38% |
MRI lesion (-) |
- |
| 5 |
Seizure free: 43%
> 80% reduction: 23% |
low DQ |
This study included only non-lesional cases |
| 6 |
Seizure free: 26% (after TCC)
Seizure free: 43% (TCC ± others) |
Low gamma power and connectivity (scalp EEG) |
- |
| 7 |
Seizure free: 43% (after TCC)
Seizure free: 71% (TCC ± others) |
NA |
Involved only patients with TSC. One patient achieved seizure freedom after taking everolimus additionally |
| 8 |
Seizure free: 41% |
Symmetrical ictal slow waves (scalp EEG)
Low interhemispheric phase lags (scalp EEG) |
Some epileptic spasms were described as tonic spasms in Kanai et al.’s study [7] |
| 9 |
Seizure free: 25% (after TCC)
Seizure free: 63% (TCC ± others) |
NA |
AQD without CC was selected for two patients based on a presurgical evaluation |
Abbreviations: ACC/PCC/TCC, anterior/posterior/total (complete) CC; AQD/PQD, anterior/posterior quadrant disconnection; CC, corpus callosotomy; CR, cortical resection; ES, epileptic spasms; HR, hemispherotomy/hemispherectomy; MRI, magnetic resonance imaging; NA, not analyzed; DQ, developmental quotient; SHR, subtotal HR; TCC, total corpus callosotomy; TSC, tuberous sclerosis complex.
Large data of long-term outcomes of CC for ES is unavailable. Stigsdotter-Broman reported the data of long-term outcomes of CC for tonic seizures and atonic seizures, and, in this study, the total seizure frequency gradually decreased over 5–10 years of follow-up
[33][72]. The efficacy of CC preventing interhemispheric recruitment of bilateral epileptic activities may contribute to suppression of epileptic aggravation. There also has been no evidence that the CC prevents the evolution from West syndrome to Lennox-Gastaut syndrome. However, the seizure outcome is poor in the patients who have not only spasms but also tonic seizures
[6] and cases that have evolved from West syndrome into Lennox-Gastaut syndrome
[34][73]. CC within the period of ES only or West syndrome might be warranted in the patients with unsuccessful medical treatments.
Occasionally, CC fails to achieve seizure freedom and ES continue from the unilateral hemisphere as an asymmetrical feature. In this situation, additional resection surgeries, such as cortical resection, anterior or posterior disconnection, or total or subtotal hemispherotomy/hemispherectomy are performed after CC. In previous studies, seizure-free ratios, including patients who received CC plus additional resection surgeries, ranged from 43% to 71%
[3][7][8][9][12][3,7,8,9,12]. The duration from CC to additional resection surgeries have become shorter in recent studies (1–6 months)
[9][12][9,12] than previously reported (6–62 months)
[3]. The efficacy of CC usually become apparent soon after the procedure. For the better seizure and cognitive outcomes, the early evaluation might be recommended in residual ES cases after CC.
3.2. Effects on Developments in Patients with Epileptic Spasms
2.2. Effects on Developments in Patients with Epileptic Spasms
Some studies have reported the effects of CC on patient development. In one study concerning the use of CC to treat patients with West syndrome, patients with a successful outcome (≥80% seizure reduction) had better developmental outcomes than those with poorer outcomes (<80% seizure reduction) at one and two years postoperatively
[6]. Honda et al. investigated changes in the development of 106 patients who had undergone CC surgery prior to age 6. Among 89 patients who presented with ES, 44% were reported to have improved developmental quotients one year postoperatively. In data concerning 106 patients, low preoperative developmental quotients and postoperative seizure freedom were found to correlate with developmental improvements due to CC surgery
[27][66].
43. Prognostic Factors for Seizure Outcomes Post-Corpus Callosotomy
In a study of CC non-specific to ES but including other types of drop attacks, total CC (compared with anterior CC)
[35][32], no structural etiology, no background disorders, and patients aged < 6 years
[31][70]) were reported to be favorable prognostic factors. In a study involving patients with West syndrome who presented with ES or tonic seizures, no developmental delay prior to the onset of epilepsy was found to be a favorable prognostic factor
[6].
In terms of ES outcomes, Kanai et al. visually analyzed ictal polyphasic slow waves and reported that the symmetries of negative peaks, amplitudes, and durations were favorable prognostic factors
[10]. Baba et al. analyzed presurgical recorded interictal scalp EEGs and reported that less power and connectivity of high-gamma activities were associated with favorable seizure outcomes post-CC
[8]. Oguri et al. undertook computed frequency analyses of ranged delta to gamma waves during the ictal periods in the same patient group, and reported that fewer phase lags in the delta, theta, and gamma bands predicted favorable seizure outcomes after CC
[11].
54. Surgical Treatment Selection: Resection Surgery or Corpus Callosotomy First?
5.1. Resection Surgeries and Adaptations for Epileptic Spasms
4.1. Resection Surgeries and Adaptations for Epileptic Spasms
Seizure-free ratios have been reported to range from 61% to 83%. These outcome data were relatively favorable compared with studies evaluating the outcomes of CC. However, patient backgrounds differed between those who underwent resection surgery and those who underwent CC.
Resection surgery was initially reported by Horsley in 1886, in which three adult patients with focal onset seizures had localized epileptogenic lesions surgically removed at London’s National Hospital
[36][74]. To be a suitable candidate for resection surgery, patients with focal epilepsy, that is, with semiological, neurophysiological, neuroimaging, and nuclear medicine imaging findings indicating focal or lateralized epileptogenic regions, are required
[37][38][39][40][41][42][25,34,35,75,76,77]. This concept of suitable candidates for resection surgery has also been applied to patients with ES or West syndrome
[16][17][18][19][20][25][43][16,17,18,19,20,64,78]. In previous studies involving resection surgery for patients with ES, most patients had epileptogenic lesions with a positive ratio on MRI ranging from 83% to 100% and comprised 94% of the total patients reported (
Table 2). CC studies with countable data have shown that the ratios of patients with brain lesions ranged from 0% to 65%, comprising 17% of the reported patients (
Table 1). These ratio differences indicate different surgical adaptations for each surgical strategy. Resection surgeries are usually performed in unilateral hemispheres in each patient, and lateralization signs/findings are crucial for adaptation. Lesions observed on MRI that are concordant with seizure laterality, the distribution of discharges on scalp EEG, or abnormal areas on nuclear scanning, are appropriate lesions for resection regions, as are epileptogenic lesions
[37][38][40][41][25,34,75,76]. As a representative study, Erdemir et al. reported 70 patients for whom resection strategies were decided based on lesions observed on MRI without invasive EEG monitoring
[19]. The seizure-free ratio was 60% in their study, which was similar to that in other resection studies using invasive monitoring
[19]. EEG and nuclear medicine imaging are also used to predict outcomes. Concordance between areas with interictal discharges on scalp EEG and MRI lesions or hypometabolism areas on positron emission topography (PET) in presurgical evaluations led to favorable findings in relation to seizure outcomes
[20]. PET has also been reported to help with surgical decision-making and with guiding the placement of subdural electrodes in non-lesional MRI cases
[16]. From these studies, focal or lateralized signs can be considered good indicators of resection surgery for ES, with the consistency of epileptogenic findings among each modality indicating a favorable predictive factor.
Table 2. Previous studies of resection surgery for epileptic spasms.
| Authors |
N |
Age at Surgery |
Seizure Types or Symmetry of ES |
MRI Lesion |
Procedures of Resection |
| 1 |
Chugani et al. 2015 [16] |
65 |
5.1 ± 4.4 years
(0.2–19 years) |
ES only: 23%
ES + focal: 58%
ES + generalized: 11% |
Lesion (+): 92% |
Hemispherectomy: 31%
Subtotal hemispherotomy: 26%
Multilobar: 20%
Lobar ± tuberectomy: 14%
Tuberectomy: 9% |
| 2 |
Barba et al. 2016 [17] |
80 |
5.8 ± 4.0 years |
Symmetric ES: 49%
Asymmetric ES: 24%
Both types: 28% |
Lesion (+): 96% |
Lobectomy: 72.5%
Multilobar/hemispherotomy: 27.5% |
| 3 |
Chipaux et al. 2017 [18] |
59 |
4.6 ± 3.5 years
(0.3–16 years) |
ES only: 15%
ES + others: 85% |
Lesion (+): 96% |
Hemispherotomy: 34%
Lesionectomy: 8%
Lesionectomy + cortical resection *: 46%
Frontal disconnection: 8%
Posterior disconnection: 3%
Endoscopic HH removal: 3% |
| 4 |
Erdemir et al. 2021 [19] |
70 |
1.9 ± 1.6 years |
ES only: 46%
ES + others: 54%
Symmetric: 54%
Asymmetric: 40%
Unknown symmetry: 6% |
Lesion (+): 100%
Bilateral: 24%
Unilateral: 76% |
Hemispherectomy: 44%
Lobectomy/lesionectomy: 33%
Multilobar resection: 23% |
| 5 |
Liu et al. 2021 [20] |
64 |
3.3 ± 2.7 years |
ES only: 64%
ES + others: 36% |
Lesion (+): 83% |
Hemispherotomy/subtotal hemispherotomy: 27%
Multilobar: 11%
Lobar: 34%
Tuberectomy: 23%
Unknown: 3% |
| Outcomes |
Good Prognostic Factor |
Others |
| 1 |
Seizure free: 71% |
Short epilepsy duration
MRI lesion (+) |
22 patients discontinued medication after surgery |
| 2 |
Seizure free: 61% |
Complete resection of SOZ
MRI lesion (+)
Low age at surgery/short epilepsy duration |
ECoG monitoring: 30% |
| 3 |
Seizure free: 75% |
Low age at surgery |
Visible epileptogenic lesions on MRI in most cases. Eight patients were declined surgery following presurgical evaluation because of multiple foci. |
| 4 |
Seizure free: 60%
Improvement: 24% |
Lobar/sublobar epileptogenic lesion |
MRI-oriented surgery
No invasive EEG (ECoG) |
| 5 |
Seizure free: 83% ** |
Concordances:
between MRI and scalp EEG
between PET and scalp EEG
Frequent interictal gamma activities (scalp EEG)
Intraoperative continuous discharges (ECoG) |
ECoG monitoring: 95%
Stereo-EEG: 20% |
Abbreviations: ES, epileptic spasms; HH, hypothalamic hamartoma; SOZ, seizure onset zone; MRI, magnetic resonance imaging; PET, positron emission tomography; ECoG, electrocorticography; EEG, electroencephalogram. * Resection of cortex with seizure onset zone in ECoG array; ** residual aura was accepted.
Functional deficits after the resection of eloquent cortices should be avoided as much as possible in resection surgeries
[37][25]. Although the eloquent cortices include anterior or posterior language areas, visual cortices, and the primary motor area among others, hemiparesis after the resection of primary motor cortex is the critical for the patients with ES, who usually have severe cognitive impairment. The patients presenting with ES often have large epileptogenic zones and require multilobar resection or hemispherotomy/hemispherectomy
[16][17][18][19][20][16,17,18,19,20]. If the patients present early pathologic handedness or hemiparesis, the resection surgery is considered relatively acceptable for the patients. If the epileptogenic zone is spread widely in the unilateral hemisphere, but avoids primary motor cortex on intracranial EEG, subtotal hemispherectomy, which spares the primary sensorimotor cortex, is considered a good procedure for the treatment of ES
[16][44][16,51].
5.2. Characteristics of Patients Who Undergo Corpus Callosotomy
8.2. Characteristics of Patients Who Undergo Corpus Callosotomy
In previous studies regarding CC, patients tended not to have localized or lateralized signs or findings. The largest study concerning CC surgery for patients with ES by Baba et al. included 56 patients without MRI lesions. They reported that 43% of patients were seizure-free and that 23% of patients had a ≥80% seizure reduction postoperatively [6]. CC has also been performed for patients with bilateral diffuse or multiple lesions in patients with polymicrogyria, cortical tubers, or general atrophy on brain MRI [3][7][9][31][3,7,9,70]. Criteria for CC surgery to treat ES have included patients with no lesion or equally bilateral epileptogenic lesions selected for CC surgery. Factors such as presurgical severe developmental delay [6] and symmetrical ictal slow waves [10] on presurgical EEG findings have been associated with favorable CC outcomes. Based on advanced analyses for presurgical EEG, less power and less connectivity of high-gamma activities on presurgical scalp EEG [8] recordings and lower phase lags in ictal slow and gamma waves among bilateral hemispheres [11] have been associated with favorable seizure outcomes.
5.3. Types of Epileptic Spasms in Terms of Cortical Excitations and the Role of Corpus Callosum
8.3. Types of Epileptic Spasms in Terms of Cortical Excitations and the Role of Corpus Callosum
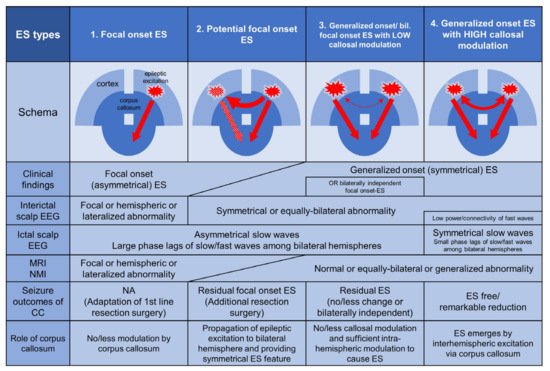
Figure 1 shows four pattern types in relation to cortical excitation and the role of the corpus callosum, and we describe the characteristics of the role of the corpus callosum, clinical features, neuroimaging, EEG, and surgical strategy based on previous knowledge and experience. Focal onset ES (type 1) is caused predominantly by unilateral cortices and tends to show a uniformly lateralized seizure type. These emerge with little or no contribution from the corpus callosum. Unilateral epileptogenic lesions on MRI or hypometabolic areas of nuclear medicine imaging are often detectable. The region or side involved in interictal EEG discharges tends to be concordant with lesions on brain imaging. Resection surgery can be performed based on presurgical evaluations. Potential focal onset ES (type 2) originates from the unilateral hemisphere; however, it is clinically not lateralized due to the rapid propagation of epileptic activity via the corpus callosum. The epileptogenic hemisphere is relatively difficult to identify using presurgical evaluations, which do not clearly show localized/lateralized or discordant localization/lateralization among the studies, and which only became apparent after CC. Additional resection surgery is sometimes performed in the newly evident epileptogenic region. There are two types of generalized onset ES in which epileptogenic cortices are equally distributed in bilateral hemispheres. However, the role of the corpus callosum in the emergence of ES differs between these types. In generalized onset ES or bilaterally independent focal onset (asymmetrical) ES with low callosal modulation (type 3), intrahemispheric modulations in each hemisphere predominates in the emergence of the ES. CC cannot prevent the emergence of ES. However, in generalized onset ES with high callosal modulation (type 4), interhemispheric modulation among the bilateral hemispheres via the corpus callosum predominates in the emergence of the ES, and CC can achieve seizure freedom without additional resection. In these cases, ictal EEG is visually bilateral and synchronous on slow waves
[10]. Computed frequency analyses of presurgical scalp EEG recordings have shown small phase lags of ictal slow and beta waves among the bilateral hemispheres and less power and connectivity on interictal records
[8][11][8,11].
Figure 1. Four pattern types from the viewpoint of cortical excitation and the role of the corpus callosum and the characteristics, clinical features, neuroimaging, EEG, and surgical strategy. Type 1: Focal onset epileptic spasms (ES) are caused predominantly by unilateral cortices and tend to show a uniformly lateralized seizure type. These ES emerge with little or no contribution from the corpus callosum. Unilateral epileptogenic lesions on MRI or hypometabolic areas of nuclear medicine imaging are often detectable. The region or side of interictal EEG discharges tends to be concordant with lesions on brain imaging. Resection surgery can be performed based on presurgical evaluations. Type 2: Potential focal onset ES originates from the unilateral hemisphere; however, rapid bilateral propagation of epileptic excitations via the corpus callosum often emerge as generalized onset (symmetrical) ES. The epileptogenic hemisphere is relatively difficult to identify with presurgical evaluations, which were revealed to be not clearly localized/lateralized or had discordant localization/lateralization among the studies, and became apparent after corpus callosotomy (CC). Additional resection surgery is sometimes performed in the newly evident epileptogenic region. Type 3: Generalized onset ES or bilaterally independent focal onset (asymmetrical) ES with low callosal modulation can emerge predominantly through intrahemispheric modulations in each hemisphere. CC cannot prevent the emergence of ES. Type 4: Generalized onset ES with high callosal modulation occurs through predominant interhemispheric modulation via the corpus callosum, and CC can achieve seizure freedom without additional resection. Abbreviations: CC, corpus callosotomy; ES, epileptic spasms; MRI, magnetic resonance imaging; NMI, nuclear medicine imaging; NA, not applicable.
8.4. Surgical Selection Flow Proposals
5.4. Surgical Selection Flow Proposals
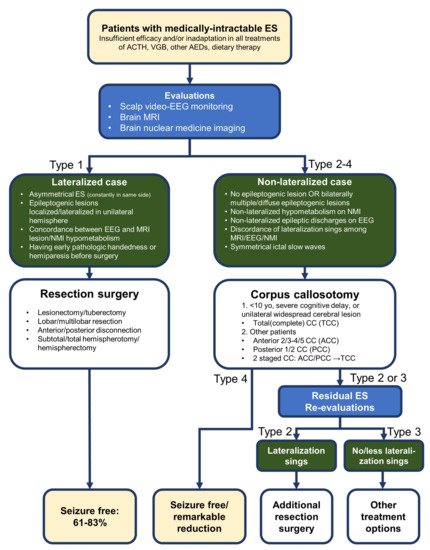
Proposals for flow of surgical selection (resection surgery or CC) in patients with intractable ES are shown in
Figure 2. In the schema, those patients with ES whose treatment had failed or who were not suitable for treatment with ACTH, vigabatrin, or other antiepileptic drugs, were evaluated using scalp video-EEG monitoring, brain MRI, and brain nuclear medicine imaging. If the epileptogenic region is localized in the unilateral hemisphere—which has been confirmed comprehensively using the following lateralization signs: asymmetrical ES (consistently in the same side), an epileptogenic lesion within the unilateral hemisphere, concordance of localization of interictal discharges on EEG and MRI lesions, and concordance of localization of interictal discharges on EEG and hypometabolism in nuclear medicine imaging—then resection surgery should be selected. If patients have no or fewer lateralization signs, that is, no or bilateral multiple epileptogenic lesions, non-lateralized epileptogenic findings on EEG or nuclear medicine imaging, symmetrical ictal slow waves and/or discordance of these signs, then CC is selected as first-line treatment. Patients who continue to have ES can receive additional resection surgery if re-evaluations (mainly neurophysiological examinations) show lateralization signs. If additional resection surgery is not appropriate, treatments using vagus nerve stimulation, dietary therapy, and other antiepileptic drugs can be attempted.
Figure 2. Selection flow of surgery for medically-intractable epileptic spasms (ES). If the epileptogenic region is identified in the unilateral hemisphere on the basis of lateralization signs—asymmetrical ES, epileptogenic lesion localized or lateralized in the unilateral hemisphere, concordance between localization of interictal discharges on EEG and MRI lesions, and concordance between localization of interictal discharges on EEG and hypometabolism in nuclear medicine imaging—the patient is presumed as lateralized case (ES type 1 in Figure 1) and resection surgeries (including frontal/posterior disconnection, subtotal or total hemispherotomy/hemispherectomy) are selected. Patients with early pathologic handedness or hemiparesis before surgery are considered relatively good candidates for resection surgery. If the patients have no, less or discordant lateralization signs—no or bilaterally multiple epileptogenic lesions, non-lateralized epileptogenic findings on EEG or nuclear medicine imaging, symmetrical ictal slow waves and/or discordance among findings of EEG/MRI and nuclear medicine imaging—the patient is presumed as non-lateralized case (ES type 2–4 in Figure 1) and corpus callosotomy (CC) is selected first. The ratio of seizure freedom in CC is estimated at 25–79% from previous studies (Table 1). If the patient is under 10 years of age, presenting severe cognitive impairment or unilateral widespread cerebral lesion, total CC is selected. In other patients, anterior, or posterior is initially recommended (the patients with unilateral widespread cerebral lesion can be considered for hemispherotomy/hemispherectomy). Additional total CC (two-staged CC) is considered in the patients with residual ES. Type 4 ES mostly ceases only by CC. If re-evaluations (mainly neurophysiological examinations) show lateralization signs, the ES is thought of as type 2 and additional resection surgery is recommended (seizure freedom: 43–71%). If the ES remains after CC (no change, bilaterally independent or milder ES than before), other treatments including antiepileptic drugs, dietary therapy and/or vagus nerve stimulations are selected.