
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Raphael Werner | + 2448 word(s) | 2448 | 2021-12-22 02:06:54 | | | |
| 2 | Conner Chen | Meta information modification | 2448 | 2022-01-06 01:51:29 | | |
Video Upload Options
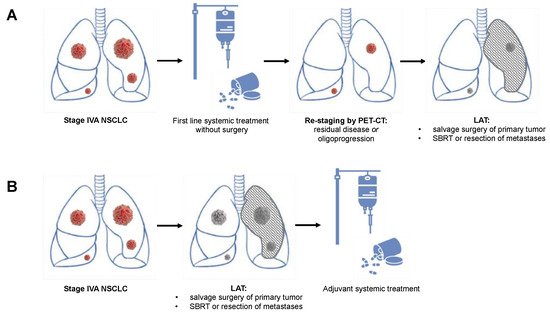
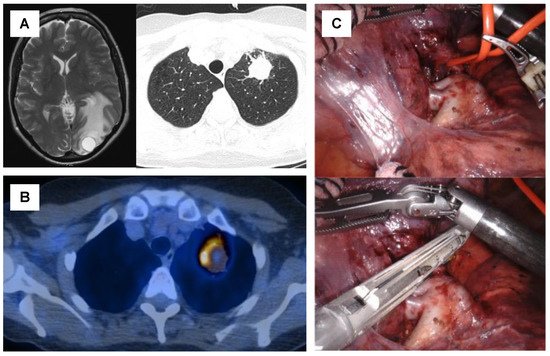
In oligometastatic NSCLC, the treatment of all tumor sites should be technically feasible with tolerable toxicity. It was thus proposed that oligometastatic NSCLC should include five or fewer metastases in three or fewer organs. Notably, the primary tumor and an involvement of mediastinal lymph nodes are excluded as a metastatic site, while pulmonary or pleural metastases are counted as a metastatic site. Patients with diffuse serosal metastases (meningeal, pericardial, pleural, or peritoneal) or bone marrow involvement are as well excluded from the definition of oligometastatic NSCLC, for they cannot be treated with radical intent. In general, most (oligo) metastases of NSCLC are found in the brain (35.5%), followed by the contralateral lung (33.6%), the adrenal glands (10%), bones (8.5%), and the liver (2.4%). One-fourth of all patients with metastatic non-small cell lung cancer presents with a limited number of metastases and relatively low systemic tumor burden. This oligometastatic state with limited systemic tumor burden may be associated with remarkably improved overall and progression-free survival if both primary tumor and metastases are treated radically combined with systemic therapy. This local aggressive therapy (LAT) requires a multidisciplinary approach including medical oncologists, radiation therapists, and thoracic surgeons.
1. Surgical Treatment for Oligometastatic Non-Small Cell Lung Cancer
| Study Abbreviation | ClinicalTrails.gov Identifier |
Phase | Setting | Type of Systemic Treatment | Type of LAT | Timing of LAT | n | No. of Metastases | Primary End Points |
Planned Completion |
|---|---|---|---|---|---|---|---|---|---|---|
| 14-18 CHESS | NCT03965468 | II | Synchronous oligometastatic NSCLC | Durvalumab, Carboplatin, Paclitaxel | Primary: Surgery or radical radiotherapyMetastases: SBRT | Neoadjuvant systemic treatment | 47 | Max. 3 | PFS | 12/2021 |
| OMEGA | NCT03827577 | III | Oligometastatic NSCLC | Standard medical therapy | Surgery, Radiotherapy, RFA | Neoadjuvant systemic treatment or primary LAT | 195 | Max. 3 | OS | 09/2022 |
| n/a | NCT02759835 | II | EGFR-mutated OPD NSCLC | Osimertinib | Surgery, SBRT, radiofrequency ablation | LAT after oligoprogression under first-lineOsimertinib | 37 | n/a | PFS | 09/2022 |
| n/a | NCT02316002 | II | Oligometastatic NSCLC | Adjuvant Pembrolizumab | Completed first-line treatment (surgery, SBRT, radiotherapy, chemotherapy) | Any first-line treatment followed by adjuvant pembrolizumab | 51 | n/a | PFS | 09/2022 |
| LONESTAR | NCT03391869 | III | Stage IV NSCLC (incl. OMD subgroup) | Nivolumab and ipilimumab | Surgery, radiotherapy | Combined neoadjuvant and adjuvant immunotherapy | 270 | n/a | OS | 12/2022 |
| NORTHSTAR | NCT03410043 | II | EGFR-mutatedStage IIIB or IV NSCLC (incl. OMD subgroup) | Osimertinib | Surgery, radiotherapy | Combined neoadjuvant and adjuvant Osimertinib | 143 | n/a | PFS | 01/2023 |
| LAT-FLOSI | NCT04216121 | IIb | EGFR-mutated OPD NSCLC | Osimertinib | Surgery, SBRT | LAT after oligoprogression under first-lineOsimertinib | 39 | Max. 3 | PFS | 08/2023 |
2. Radiation Therapy for Oligometastatic Non-Small Cell Lung Cancer
3. Patient Selection Criteria for Local Aggressive Therapy
3.1. Site of the Primary Tumor
3.2. Site of Metastases
3.3. Mediastinal Lymph Node Involvement
3.4. Synchronous and Metachronous Metastases
3.5. Performance Status
References
- Ashworth, A.; Rodrigues, G.; Boldt, G.; Palma, D. Is there an oligometastatic state in non-small cell lung cancer? A systematic review of the literature. Lung Cancer 2013, 82, 197–203.
- Berzenji, L.; Debaenst, S.; Hendriks, J.M.H.; Yogeswaran, S.K.; Lauwers, P.; Van Schil, P.E. The role of the surgeon in the management of oligometastatic non-small cell lung cancer: A literature review. Transl. Lung Cancer Res. 2021, 10, 3409–3419.
- Suzuki, S.; Goto, T. Role of Surgical Intervention in Unresectable Non-Small Cell Lung Cancer. J. Clin. Med. 2020, 9, 3881.
- Zheng, Y.; Jaklitsch, M.T.; Bueno, R. Neoadjuvant Therapy in Non–Small Cell Lung Cancer. Surg. Oncol. Clin. N. Am. 2016, 25, 567–584.
- Liang, H.; Yang, C.; Gonzalez-Rivas, D.; Zhong, Y.; He, P.; Deng, H.; Liu, J.; Liang, W.; He, J.; Li, S. Sleeve lobectomy after neoadjuvant chemoimmunotherapy/chemotherapy for local advanced non-small cell lung cancer. Transl. Lung Cancer Res. 2021, 10, 143–155.
- Yang, C.-F.J.; McSherry, F.; Mayne, N.R.; Wang, X.; Berry, M.F.; Tong, B.; Harpole, D.H.; D’Amico, T.A.; Christensen, J.D.; Ready, N.E.; et al. Surgical Outcomes After Neoadjuvant Chemotherapy and Ipilimumab for Non-Small Cell Lung Cancer. Ann. Thorac. Surg. 2018, 105, 924–929.
- Weder, W.; Collaud, S.; Eberhardt, W.E.; Hillinger, S.; Welter, S.; Stahel, R.; Stamatis, G. Pneumonectomy is a valuable treatment option after neoadjuvant therapy for stage III non-small-cell lung cancer. J. Thorac. Cardiovasc. Surg. 2010, 139, 1424–1430.
- Beattie, R.; Furrer, K.; Dolan, D.P.; Curioni-Fontecedro, A.; Lee, D.N.; Frauenfelder, T.; Hoeller, S.; Weder, W.; Bueno, R.; Opitz, I.; et al. Two centres experience of lung cancer resection in patients with advanced non-small cell lung cancer upon treatment with immune checkpoint inhibitors: Safety and clinical outcomes. Eur. J. Cardio-Thorac. Surg. 2021, 60, 1297–1305.
- Dickhoff, C.; Otten, R.H.J.; Heymans, M.; Dahele, M. Salvage surgery for recurrent or persistent tumour after radical (chemo)radiotherapy for locally advanced non-small cell lung cancer: A systematic review. Ther. Adv. Med. Oncol. 2018, 10.
- Kaba, E.; Ozyurtkan, M.O.; Ayalp, K.; Cosgun, T.; AlOmari, M.R.; Toker, A. Salvage thoracic surgery in patients with lung cancer: Potential indications and benefits. J. Cardiothorac. Surg. 2018, 13, 13.
- Romero-Vielva, L.; Viteri, S.; Moya-Horno, I.; Toscas, J.I.; Maestre-Alcácer, J.A.; Cajal, S.R.Y.; Rosell, R. Salvage surgery after definitive chemo-radiotherapy for patients with Non-Small Cell Lung Cancer. Lung Cancer 2019, 133, 117–122.
- Bauman, J.E.; Mulligan, M.S.; Martins, R.G.; Kurland, B.; Eaton, K.D.; Wood, D.E. Salvage Lung Resection After Definitive Radiation (>59 Gy) for Non-Small Cell Lung Cancer: Surgical and Oncologic Outcomes. Ann. Thorac. Surg. 2008, 86, 1632–1639.
- Casiraghi, M.; Maisonneuve, P.; Piperno, G.; Bellini, R.; Brambilla, D.; Petrella, F.; De Marinis, F.; Spaggiari, L. Salvage Surgery After Definitive Chemoradiotherapy for Non–small Cell Lung Cancer. Semin. Thorac. Cardiovasc. Surg. 2017, 29, 233–241.
- Sonobe, M.; Yutaka, Y.; Nakajima, D.; Hamaji, M.; Menju, T.; Ohsumi, A.; Chen-Yoshikawa, T.F.; Sato, T.; Date, H. Salvage Surgery After Chemotherapy or Chemoradiotherapy for Initially Unresectable Lung Carcinoma. Ann. Thorac. Surg. 2019, 108, 1664–1670.
- Kobayashi, A.K.; Horinouchi, H.; Nakayama, Y.; Ohe, Y.; Yotsukura, M.; Uchida, S.; Asakura, K.; Yoshida, Y.; Nakagawa, K.; Watanabe, S.-I. Salvage surgery after chemotherapy and/or radiotherapy including SBRT and proton therapy: A consecutive analysis of 38 patients. Lung Cancer 2020, 145, 105–110.
- Ohtaki, Y.; Shimizu, K.; Suzuki, H.; Suzuki, K.; Tsuboi, M.; Mitsudomi, T.; Takao, M.; Murakawa, T.; Ito, H.; Yoshimura, K.; et al. Salvage surgery for non-small cell lung cancer after tyrosine kinase inhibitor treatment. Lung Cancer 2021, 153, 108–116.
- Jones, G.; Lengel, H.; Hsu, M.; Tan, K.; Caso, R.; Ghanie, A.; Connolly, J.; Bains, M.; Rusch, V.; Huang, J.; et al. Management of Synchronous Extrathoracic Oligometastatic Non-Small Cell Lung Cancer. Cancers 2021, 13, 1893.
- Wang, Z.; Gao, S.-G.; Xue, Q.; Guo, X.-T.; Wang, L.-X.; Yu, X.; Yang, Y.-K.; Mu, J.-W. Surgery of primary non-small cell lung cancer with oligometastasis: Analysis of 172 cases. J. Thorac. Dis. 2018, 10, 6540–6546.
- Arrieta, O.; Escamilla-López, I.; Lyra-González, I.; Barrón, F.; Ramírez-Tirado, L.A.; Vergara, E.; Corona-Cruz, J.; Maldonado, F.; Jiménez-Fuentes, E. Radical aggressive treatment among non-small cell lung cancer patients with malignant pleural effusion without extra-thoracic disease. J. Thorac. Dis. 2019, 11, 595–601.
- Amini, A.; Verma, V.; Simone, C.B., II; Chetty, I.J.; Chun, S.G.; Donington, J.; Edelman, M.J.; Higgins, K.A.; Kestin, L.L.; Movsas, B.; et al. American Radium Society Appropriate Use Criteria for Radiation Therapy in Oligometastatic or Oligoprogressive Non-Small Cell Lung Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2021, in press.
- Theelen, W.S.M.E.; Chen, D.; Verma, V.; Hobbs, B.P.; Peulen, H.M.U.; Aerts, J.G.J.V.; Bahce, I.; Niemeijer, A.L.N.; Chang, J.Y.; de Groot, P.M.; et al. Pembrolizumab with or without radiotherapy for metastatic non-small-cell lung cancer: A pooled analysis of two randomised trials. Lancet Respir. Med. 2021, 9, 467–475.
- Congedo, M.T.; Cesario, A.; Lococo, F.; De Waure, C.; Apolone, G.; Meacci, E.; Cavuto, S.; Granone, P. Surgery for oligometastatic non–small cell lung cancer: Long-term results from a single center experience. J. Thorac. Cardiovasc. Surg. 2012, 144, 444–452.
- De Ruysscher, D.; Wanders, R.; Hendriks, L.E.; van Baardwijk, A.; Reymen, B.; Houben, R.; Bootsma, G.; Pitz, C.; van Eijsden, L.; Dingemans, A.M.C.; et al. Progression-Free Survival and Overall Survival Beyond 5 Years of NSCLC Patients With Synchronous Oligometastases Treated in a Prospective Phase II Trial (NCT 01282450). J. Thorac. Oncol. 2018, 13, 1958–1961.
- Iyengar, P.; Wardak, Z.; Gerber, D.E.; Tumati, V.; Ahn, C.; Hughes, R.S.; Dowell, J.E.; Cheedella, N.; Nedzi, L.; Westover, K.D.; et al. Consolidative Radiotherapy for Limited Metastatic Non-Small-Cell Lung Cancer: A Phase 2 Randomized Clinical Trial. JAMA Oncol. 2018, 4, e173501.
- Collen, C.; Christian, N.; Schallier, D.; Meysman, M.; Duchateau, M.; Storme, G.; De Ridder, M. Phase II study of stereotactic body radiotherapy to primary tumor and metastatic locations in oligometastatic nonsmall-cell lung cancer patients. Ann. Oncol. 2014, 25, 1954–1959.
- Palma, D.A.; Olson, R.; Harrow, S.; Gaede, S.; Louie, A.V.; Haasbeek, C.; Mulroy, L.; Lock, M.; Rodrigues, G.B.; Yaremko, B.P.; et al. Stereotactic Ablative Radiotherapy for the Comprehensive Treatment of Oligometastatic Cancers: Long-Term Results of the SABR-COMET Phase II Randomized Trial. J. Clin. Oncol. 2020, 38, 2830–2838.
- Patchell, R.A.; Tibbs, P.A.; Walsh, J.W.; Dempsey, R.J.; Maruyama, Y.; Kryscio, R.J.; Markesbery, W.R.; Macdonald, J.S.; Young, B. A Randomized Trial of Surgery in the Treatment of Single Metastases to the Brain. N. Engl. J. Med. 1990, 322, 494–500.
- Coster, J.N.; Groth, S.S. Surgery for Locally Advanced and Oligometastatic Non–Small Cell Lung Cancer. Surg. Oncol. Clin. N. Am. 2020, 29, 543–554.
- Raz, D.J.; Lanuti, M.; Gaissert, H.C.; Wright, C.D.; Mathisen, D.J.; Wain, J.C. Outcomes of Patients With Isolated Adrenal Metastasis From Non-Small Cell Lung Carcinoma. Ann. Thorac. Surg. 2011, 92, 1788–1793.
- Opitz, I.; Patella, M.; Payrard, L.; Perentes, J.Y.; Inderbitzi, R.; Gelpke, H.; Schulte, S.; Diezi, M.; Gonzalez, M.; Krueger, T.; et al. Prognostic factors of oligometastatic non-small-cell lung cancer following radical therapy: A multicentre analysis. Eur. J. Cardio-Thorac. Surg. 2020, 57, 1166–1172.
- Casiraghi, M.; Bertolaccini, L.; Sedda, G.; Petrella, F.; Galetta, D.; Guarize, J.; Maisonneuve, P.; De Marinis, F.; Spaggiari, L. Lung cancer surgery in oligometastatic patients: Outcome and survival. Eur. J. Cardio-Thorac. Surg. 2020, 57, 1173–1180.
- Salah, S.; Tanvetyanon, T.; Abbasi, S. Metastatectomy for extra-cranial extra-adrenal non-small cell lung cancer solitary metastases: Systematic review and analysis of reported cases. Lung Cancer 2012, 75, 9–14.
- Ashworth, A.B.; Senan, S.; Palma, D.A.; Riquet, M.; Ahn, Y.C.; Ricardi, U.; Congedo, M.T.; Gomez, D.R.; Wright, G.; Melloni, G.M.; et al. An Individual Patient Data Metaanalysis of Outcomes and Prognostic Factors After Treatment of Oligometastatic Non–Small-Cell Lung Cancer. Clin. Lung Cancer 2014, 15, 346–355.
- Billing, P.S.; Miller, D.L.; Allen, M.S.; Deschamps, C.; Trastek, V.F.; Pairolero, P.C. Surgical treatment of primary lung cancer with synchronous brain metastases. J. Thorac. Cardiovasc. Surg. 2001, 122, 548–553.
- Curioni-Fontecedro, A.; Ickenberg, C.; Franzen, D.; Rogler, G.; Burger, I.A.; Broek, M.V.D. Diffuse pseudoprogression in a patient with metastatic non-small-cell lung cancer treated with Nivolumab. Ann. Oncol. 2017, 28, 2040–2041.
- Isbell, J.M.; Li, B.T.; Gomez, D.R. The emerging role of local therapy in oligometastatic non–small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2021.
- Tanvetyanon, T.; Robinson, L.A.; Schell, M.J.; Strong, V.E.; Kapoor, R.; Coit, D.G.; Bepler, G. Outcomes of Adrenalectomy for Isolated Synchronous Versus Metachronous Adrenal Metastases in Non–Small-Cell Lung Cancer: A Systematic Review and Pooled Analysis. J. Clin. Oncol. 2008, 26, 1142–1147.
- Ampil, F.; Caldito, G.; Milligan, S.; Mills, G.; Nanda, A. The elderly with synchronous non-small cell lung cancer and solitary brain metastasis: Does palliative thoracic radiotherapy have a useful role? Lung Cancer 2007, 57, 60–65.
- Frost, N.; Tessmer, A.; Schmittel, A.; van Laak, V.; Raspe, M.; Ruwwe-Glösenkamp, C.; Brunn, M.; Senger, C.; Böhmer, D.; Ochsenreither, S.; et al. Local ablative treatment for synchronous single organ oligometastatic lung cancer—A propensity score analysis of 180 patients. Lung Cancer 2018, 125, 164–173.




