Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Maria Jesus Vinolo-Gil | + 3116 word(s) | 3116 | 2021-10-09 04:27:46 | | | |
| 2 | Rita Xu | Meta information modification | 3116 | 2021-11-25 05:09:45 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Vinolo-Gil, M.J. Cerebral Palsy. Encyclopedia. Available online: https://encyclopedia.pub/entry/16365 (accessed on 08 February 2026).
Vinolo-Gil MJ. Cerebral Palsy. Encyclopedia. Available at: https://encyclopedia.pub/entry/16365. Accessed February 08, 2026.
Vinolo-Gil, Maria Jesus. "Cerebral Palsy" Encyclopedia, https://encyclopedia.pub/entry/16365 (accessed February 08, 2026).
Vinolo-Gil, M.J. (2021, November 25). Cerebral Palsy. In Encyclopedia. https://encyclopedia.pub/entry/16365
Vinolo-Gil, Maria Jesus. "Cerebral Palsy." Encyclopedia. Web. 25 November, 2021.
Copy Citation
Cerebral palsy (CP) is defined as a group of permanent disorders in the development of movements and postures, provoking limitations on activity, attributed to non-progressive disturbances that occurred in the development of the foetal or infant brain.
cerebral palsy
music-therapy
physiotherapy
motor function
1. Introduction
Cerebral palsy (CP) is defined as a group of permanent disorders in the development of movements and postures, provoking limitations on activity, attributed to non-progressive disturbances that occurred in the development of the foetal or infant brain. Motor disorders of CP are often accompanied by alterations to sensation, perception, cognition, communication, and behaviour due to epilepsy and secondary musculoskeletal problems [1].
CP affects approximately 1 out of 500 new-borns, with an estimated prevalence of 17 million people worldwide [2], which establishes it as the most common motor disability during childhood [3].
Physical therapy (PT) plays a key role in its treatment through several therapeutic interventions that achieve improved physiological and functional outcomes [4]. Based on recent evidence, current goal-oriented functional approaches are considered effective, although more research is needed to determine the best ways to achieve even more improved functional outcomes in children with CP [5]. Music therapy (MT) might be a new avenue that, in combination with PT, would help to improve motor function in patients with CP [6][7].
In the words of Jackson and his collaborators, "Music therapy is a paramedical specialization based scientifically on clinical–therapeutic methods and establishes a working methodology and a series of techniques with the objective of promoting positive cognitive, physical, mental, and social changes in individuals with health or behaviour disorders" [8]. Through the use of rhythmic, harmonic, and melodic sounds by means of improvisations, musical compositions, reproduction of sounds, and other techniques, an improvement in communication, expression, organization, learning, and mobilization is achieved by also obtaining a rehabilitative effect [9][10].
Several studies have demonstrated the positive effect of MT on numerous conditions, such as cancer [11], burns [12], and cognitive deterioration [13], on diverse factors, such as breathing, blood flow, heart rate, blood pressure, acceleration of the metabolism, and oxygenation and on different emotional states, such as anguish, anxiety, tension, stress, and fear [14]. MT has also been used in people with CP in order to determine its influence on muscle tone [15][16][17].
Bean and Oldfield (2001) performed a series of exercises for the development of specific movements in children with CP, creating musical activities for the development of functional skills [18]. This active work was also used by Lasse Hjelm, the author of the functionally oriented music therapy (FMT) method, who commented: "music therapy focused on human body functions is often indicated in motor impairments and is highly applicable in people with CP” [19]. Another example of the application of active musical activities for the development of motor skills in people with CP was carried out by Hatampour and his collaborators [20].
In terms of functional capacity, certain authors have advanced the traditional concepts of music and education, such as Richardson, who adjusted Zoltán Kodály’s methodology for children with disabilities, using more concrete techniques that helped the development of motor skills, such as manual signal tests [21], an adaptation of Orff Schulwerk’s methodology, or the Suzuki method [22]. Significant results [23] were also found through the use of music to motivate patients during physiotherapy sessions.
At the beginning of the 1990s, the first clinical collaborations between music therapists and physiotherapists began, leading to the beginnings of neurological music therapy (NMT). NMT is an evidence-based system of clinical interventions or techniques for retraining the sensory–motor area, speech and language, and cognitive functions that may be impaired following an injury of neurological origin [24]. Additionally, it can promote neuroplasticity by motor control learning through therapeutic instrumental music performance (TIMP) [25].
Other music therapy techniques have also been used, such as patterned sensory enhancement (PSE), which uses musical elements to translate the components of a movement into sound patterns in order to give temporal, spatial, and force cues about the movement to improve its execution [26], or rhythmic auditory stimulation (RAS), which uses rhythmic sensory stimuli to improve motor control in rehabilitation [27].
People with CP have affected gross motor function and manual function but may be able to integrate rhythm and movement and use musical instruments in their therapy, taking advantage of all the benefits of this technique for neuroplasticity and motor control [28]. Alves-Pinto et al. (2015) showed that functional rehabilitation in people with CP is not due to chance, since MT introduces changes in the internal mechanisms underlying motor function [29].
Several studies can also be found on elderly people [30], patients with Parkinson’s [31][32], or patients with cerebrovascular accidents [33] that analyse how a combination of PT and MT achieves improvements in motor function. However, there are few trials in which they are used for the treatment of CP [28].
2. Selection of Studies
The search strategy was carried out on 17 databases, from which we obtained 151 articles. Of these, 5 belonged to Web of Science, 5 to PubMed, 3 to CINALH, 1 to Medline, 6 to PEDro, 44 to ProQuest, 22 to Ovid, 6 to Scopus, 3 to Cochrane Plus, 1 to ABI Inform/ProQuest, 18 to JSTOR, 0 to EBSCO, 26 to ScienceDirect, 1 to Emerald, 0 to PROSPERO, 0 to SSRN, 8 to PsycInfo, 2 to TESEO, 0 to OpenGrey, 1 to Grey Literature Database, and 1 to Music Therapy Conference Proceedings.
After filtering by eligibility criteria, focusing on the efficacy of the treatment on cerebral palsy to improve the motor function through MT and PT and eliminating duplicate articles, 30 documents were obtained. After reading them, eight articles were judged to be valid for the review. The main steps related to the bibliographic search phase are presented in Figure 1 using a flowchart.
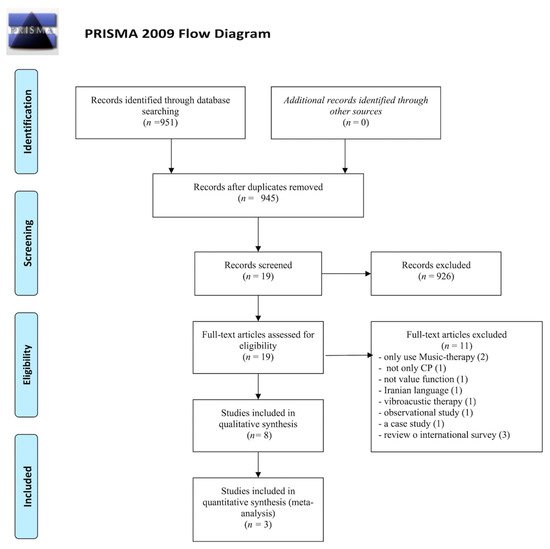
Figure 1. Information flowchart of the different phases of the systematic review, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
3. Study Design and Characteristics
Eight studies with a total of 234 participants diagnosed with cerebral palsy aged between 4 [25] and 52 [34] years were included in this systematic review. The main findings of the systematic review are presented in Table 1. The type of cerebral palsy, the average age of the patients, the “motor function” outcome, as well as the most relevant results are described in Table 1. Table 2 shows intervention details.
Table 1. Results of studies included within the systematic review.
| Study | N Age/Mean (SD) Age Range (Years) |
Type of PCI | “Motor Function” Outcome | t/w min Weeks |
Results |
|---|---|---|---|---|---|
| Kwak [35] (NRCT) |
n = 25 Con: 9 Exp1: 9 Exp2: 7 6–20 |
Spastic cerebral palsy | 14-meter walkway Gait parameter (cadence, stride length, velocity, symmetry) |
5 t/w 30 min 3 weeks |
Exp1: improved stride length (t = −3109, p = 0.014), velocity (t = −3029, p = 0.016) and symmetry (t = −3029, p = 0.016) |
| Kim et al. [36] (NRCT) |
n = 44 Con: 30 healthy people Exp: 14 with CP 25.64 ± 7.31 |
Bilateral spasticity |
Temporal and kinematic gait parameters GDI Asymmetry |
1 session | Kinematic changes of pelvic and hip movement, and GDI was significantly changed with RAS (p < 0.05) Improved temporospatial asymmetry in household ambulators |
| Kim et al. [37] (RCT) |
n = 39 Con: 19 27.3 (2.5) Exp: 20 27.3 (2.4) |
Bilateral spasticity |
Temporal and kinematic parameters of the gait GDI |
3 t/w 30 min 3 weeks |
Exp: improved cadence, velocity, step length, stride length (p < 0.05), previous pelvic tilt, hip flexion (p < 0.05), GDI (p < 0.05) Con: improved Ri and Re (p < 0.05). |
| Peng et al. [26] (RCT) |
n = 23 8.7 (2) Con: NA Exp: NA |
Spastic diplegia |
Kinematic parameters Movement time NJI Flex trunk angles COM address |
1 session | Maximum knee extension power (p = 0.009), >total extension power (p = 0.015), >COM fluidity (p = 0.01), <movement time (p = 0.003), and remained without music |
| Hamed et al. [38] (RCT) |
n = 30 Con: 15 7.07 (0.82) Exp: 15 Exp: 7.03 (0.76) |
Spastic hemiparesis |
Running speed Stride length Cadence Cycle time |
5 t/w 60min 12 weeks |
Exp: improved velocity (p < 0.0001) and cadence (p < 0.008) Exp: velocity 0.68 ± 0.09 m/s Con: 0.420 ± 11 m/s for control group (t = 6.2) (p < 0.0001) Exp: cadence 124.3 ± 4.3 steps/min Con: 128.7 ± 4.1 steps/min (t = 2.8) (p < 0.008) |
| Efraimidou et al. [34] (RCT) |
n = 10 Con: 5 38.80 (12.28) Exp: 5 35.20 (13.01) |
Spastic hemiparesis |
TUG Lift and walk test MWT Berg’s Scale Static and dynamic balance with EPS platform |
2 t/w 50 min 8 weeks |
Exp: improvement in gait and balance (p ≤ 0.05) Improvement in gait time (s) (F1,8 = 13.60, p = 0.006, η2 = 0.630), in normal gait speed (m/s) (F1,8 = 8.53, p = 0.019, η2 = 0.516), but not in fast gait speed (m/s) (F1,8 = 4.84, p = 0.059, η2 = 0.377) Statistically significant differences in intervention group between the two measurements regarding static and dynamic balance score (t = −8.63, df = 4, p = 0.001) |
| Wang et al. [39] (RCT) |
n = 45 Con: 24 9 (1.99) Exp: 21 8.98 (2.61) |
Spastic diplegia |
GMFM PEDI STS |
3t/w 6 weeks |
Exp: improvements in gross motor function capacity (p < 0.05) maintained 6–12 weeks (p < 0.13). No improvements in daily functioning, strength, and walking speed. |
| Marrades-Caballero et al. [25] (crossover) |
n = 18 10 (6) |
Severe bilateral |
UL functionality Chailey skill levels |
16 weeks | Improved Chailey Levels of Ability (p = 0.002): “activities” section (p = 0.007), “arm and hand position” section (p = 0.027) and locomotor stages (p = 0.008). Persisted for 4 months. |
SD: standard deviation; Con: control group; Exp: experimental group; NRCT: nor randomized controlled trial; RCT: randomized controlled trial; GDI: step deviation index; NA: not available; NDT: neurodevelopmental therapy/Bobath; t/w: times per week; MRI: maximum repetition; Ri: internal rotation; Re: external rotation; STS: sit to stand test; COM: centre of mass; NJI: normalized jerk index; TUG: timed up and go; MWT: 10-meter walk test; BBS: Berg’s balance scale; GMFM: gross motor function measure; PEDI: paediatric evaluation of disability inventory; UL: upper limb.
Table 2. Type of intervention.
| Study | Intervention |
|---|---|
| Kwak et al. [35] | Con: conventional gait training with a physical therapist Exp1: gait training + RAS A music therapist provided verbal instructions. A drum was used to emphasize the beat. A computer speaker system played the prescribed music (4/4 m, 105–120 beats per minute). The tempo of the music was increases by 10% (2nd week) and 15% (3rd week). Depending on individual needs, the physical therapist and music therapist developed muscle strengthening exercises using PSE and TIMP. Exp2: gait training + self-guided RAS A tape and instructions were given. The researcher demonstrated how they could feel the beat and how they could walk with the prescribed music for 30 min of daily self-training. |
| Kim et al. [36] | -Gait training without RAS -Gait training with RAS 1. A subject walked barefoot along a 10 m walkway three times at the individual’s preferred walking speed without RAS. 2. Walking cadence (steps/min) was calculated based on the gait parameters in Step 1. 3. The tempo of metronome beats (bpm) was set to participant’s cadence obtained in Step 2. 4. RAS was provided by the music therapists, playing a simple rhythm pattern using chord progression on a keyboard with metronome beats. 5. The same chord pattern was repeated providing a continuous timing cue and period sequence for 1–2 min to help a subject adapt to RAS immediately. 6. A subject walked 10 m three times again with RAS. |
| Kim et al. [37] | Con: NDT. Gait training Exp: Gait training with RAS 1. A participant walked barefoot along the walkway (10 m) three times, at the individual’s preferred walking speed, before rhythmic auditory stimulation application. 2. The individual’s cadence (steps/min) was calculated based on the gait parameters in Step 1. 3. The tempo of metronome beats (bpm) was set to the participant’s cadence obtained in Step 2. 4. RAS was provided by music therapists, who played a simple rhythm pattern synchronized with the beats of a metronome, using chord progressions on a keyboard. |
| Peng et al. [26] | Con: STS with 50% of 1RM without PSE, 8 reps Exp: STS with 50% of 1RM, 5 reps with PSE and 3 reps without PSE The individualized PSE music was composed by a music therapist with an electronic keyboard using GarageBand software on a Mac Mini at an intensity of 75 dBA, varying the tempo, harmonies, metre. |
| Hamed et al. [38] | Con: NDT + usual gait training -NDT: approximation of the upper and lower limbs in a regular and rhythmic manner, facilitation of righting, equilibrium, and protective reactions, training of postural stability and equal weight shift, stretching and strengthening exercises of the upper and lower limbs and back muscles. -Gait training program without pedometer Exp: same + pedometer-based gait training programme. A talking pedometer was fastened to a belt or waistband. It played seven melodies while walking or jogging, and the tempo synchronized with walking speed. The activities included walking forward, backward, and sideways between parallel bars, on a walking line, and on a balance beam; stepping forward on a stepper (stairs); and training of walking with different obstacles and on different floor surfaces. |
| Efraimidou et al. [34] | Con: ball and puck training program Exp: The program included gait and balance with music exercises according to RAS. -Warm-up period: stretching exercises accompanied with music tracks of 4/4 m and a tempo of 70 beats per minute -Main part: Participants walked to the rhythm veer (music tracks of 4/4, 90 beats/min). Then they continued to move with pace in a straight line for a distance of 10 m with forward, backward, right, and left steps, as well as standing on one leg with change for some seconds. -Cool-down: relaxation exercises, breathing and music (4/4, 70 beats/min) |
| Wang et al. [39] | Con: Loaded STS exercise with weighted body vest. 3 sets: -1st and 3rd: load at 20% of 1RM, 10 reps -2nd: 50% of 1RM until fatigue Exp: To prescribe the PSE music, loaded STS 50% of 1RM, 6 reps. The fastest three STS movements were selected as references to prescribe PSE music using an electronic keyboard and GarageBand software on a Mac (Apple Inc., Cupertino, CA, USA). Music provided cueing of the movement period. Caregivers supervised. Every 2 weeks, the music therapist adjusted musical elements according to the individual’s needs. |
| Marrades-Caballero et al. [25] | Con: physiotherapy (no technique specified), 1 t/w Exp: NMT sessions by two music therapists. The music was live and customized according to each patient. Small percussion instruments, Spanish guitar, keyboard, and drums were played. Two types of activities: -At the beginning, patients chose and played the musical instruments using their own movement strategies (hitting, rubbing, crashing) to generate rhythmic music patterns. Music therapists played along. -Task-specific training with varied and incremental levels of difficulty. Music therapists composed small pieces of music testing different music parameters trying to trigger forearm pronation and supination, elbow flexion and extension, and shoulder flexion. The activities were performed in a prone position or sitting in their wheelchairs and were aimed at challenging upper-limb movements and head and trunk control. |
Con: control group; Exp: experimental group; NDT: neurodevelopmental therapy/Bobath; RAS: rhythmic auditory stimulation; t/w: times per week; MRI: maximum repetition; STS: sit to stand test; Rep: repetitions; PSE: patterned sensory enhancement; TIMP: therapeutic instrumental music performance; NMT: neurologic music therapy.
Different types of CP were studied: spastic diplegia [26][39], spastic hemiplegia [34][38], bilateral spasticity [36][37], spastic CP [35], and severe bilateral CP [25].
With respect to the motor function outcome, the following were analysed: kinematic parameters and temporal data (such as cadence, velocity, step length, trunk flexion angles, centre of mass movement, and symmetry) [26][35][37][38], GDI step deviation index [36][37], normalized jerk index (NJI) [26], lift and walk test [34], 10 meter gait test [34], Berg balance scale [34], TUG [34], balance [34], gross motor function measure (GMFM) [39], paediatric evaluation of disability inventory (PEDI) [39], STS [39], upper limb functionality [25], Chailey’s ability levels, and Communication Function Classification System (CFCS) [25].
As for the interventions used, the studies analysed present different characteristics in terms of the performance within the treatment sessions. The differences reside in previous trainings, duration of treatment or session, number of sessions, and number of participants, all of them variables for measuring function and performance of the techniques, either by repetition or by working time.
Working sessions during treatment vary across studies, being at least one session [26][36], and at most 60 sessions [38], with studies normally lasting from 3 to 12 weeks. The duration of the sessions varied between 30 min [35][37][40] and 60 min [38], and the frequency varied between twice a week [34] and five times a week [35][38].
In terms of PT techniques, the most frequent was gait retraining [35][36][38][41], followed by neurodevelopmental therapy (NDT) [25][37][38]; two articles used resistance techniques [26][39], and one used technique for sports training with a ball and a disc [34].
With respect to MT techniques, rhythmic auditory stimulation (RAS) was used in three of the trials [34][36][37], sensory enhancement pattern (PSE) was used in another two [26][39], a pedometer with music was also used [38], and the last one was based on a programme of instrumental music performance using neurological music therapy (TIMP) [25]. Five articles used an electronic keyboard [25][26][36][37][39].
Some cooperative work has been carried out between specialized physiotherapists and music therapists to adapt the different musical pieces to the patients’ characteristics so that they could achieve the goals proposed.
As regards the statistical evaluation in the studies analysed, for kinematic parameters of the pelvis and hip joint evaluated in the sagittal plane, Kim et al. [36] found significant changes with RAS: anterior pelvic tilt at initial contact was significantly ameliorated by RAS (15.09 ± 9.78 degrees, vs. 17.27 ± 7.64 degrees without RAS; t = 2.874, p = 0.008 by paired t-test), and angles of maximal and minimal hip flexion during a gait cycle were both significantly reduced with RAS (49.20 ± 10.99 degrees to 47.82 ± 10.87 degrees in maximal flexion, t = 2.373, p = 0.025; 9.17 ± 10.99 degrees to 7.52 ± 11.88 degrees in minimal flexion, t = 2.468, p = 0.020). However, in a later study [35], RAS aggravated maximal internal rotation in the transverse plane (p < 0.05). With respect to the findings in the knee, Peng et al. [26] achieved a small but significant difference in peak knee extensor power per limb (p = 0.04), with an effect size of 0.23, and total extensor power per limb, with p = 0.03 and an effect size of 0.35.
About gait tests, Efraimidou et al. [34] revealed a statistically significant main effect of time or group in gait time (s) (F1,8 = 13.60, p = 0.006, η2 = 0.630) in the TUG-test and on normal gait speed (m/s) (F1,8 = 8.53, p = 0.019, η2 = 0.516), but not on fast gait speed (m/s) (F1,8 = 4.84, p = 0.059, η2 = 0.377) in 10MWT. The ANOVA repeated measurement test revealed a statistically significant main effect of time or group on Berg Balance score (F1,8 = 18.01, p = 0.003, η2 = 0.692) in BBS.
Previously, Hamed et al. [38] noted that velocity was 0.68 ± 0.09 m/s (0.26 ± 0.07 change score) for the study group and 0.42 ± 0.11 m/s (0.060 ± 0.05 change score) for the control group (t = 6.2) (p < 0.0001); stride length was 0.52 ± 0.07 metres vs. 0.34 ± 0.07 metres for control (t = 6.25) (p < 0.0010); however, cadence was much less significant at 124.3 ± 4.3 steps/min (−5.8 ± 2.1 change score) for the study group and 128.7 ± 4.1 steps/min (−0.86 ± 0.05 change score) for the control group (t = 2.8) (p < 0.008). Meanwhile, Kwak et al. [35] observed increased stride length (t = −3.109, p = 0.014) and velocity (t = −3.029, p = 0.016) in the therapist-guided training group.
On the other hand, Wang [39] showed GMFM score means at four time points and observed in both groups significant main time effects of GMFM scores in Dimensions D (F = 8.9–32.2, p ≤ 0.005) and E (F = 6.4–16.4, p ≤ 0.016) and the Goal Dimension (F = 12.7–28.3, p ≤ 0.001). Additionally, significant group by time interactions were found in Dimension D at T1 (after 6 weeks of training) (p = 0.004, mean adjusted difference = 3.6, ES 0.54) and T2 (at 6 weeks) (p = 0.004, mean adjusted difference = 3.8, ES 0.54), with greater improvements in the PSE group than in the no-music group. However, the music effects did not maintain at T3 (at 12 weeks following the end of the training) (p = 0.06, ES 0.34). For the goal score, significant interactions were found at T1 (p < 0.001, ES 0.7), T2 (p = 0.004), ES 0.54, and T3 (p = 0.013, ES 0.46). The Functional Skills Scale scores of the PEDI mobility domain increased in both groups from T0 (at baseline) to T1, T0 to T2, and T0 to T3, resulting in significant main effects of time (F = 9.4–12.6, 0.001 ≤ p ≤ 0.004) [37].
Values of STS 1RM increased in both groups, resulting in a significant main effect of time at all time points (F = 11.3–15.6, p ≤ 0.002), but no interaction was found (p = 0.06–0.15) [39].
Finally, the only study that did not assess the lower limb, Marrades et al. [25], found significant differences in the Total Chailey Test (p = 0.002), arm and hand position section (p = 0.027), activities (p = 0.007), and locomotor stages (p = 0.008).
References
- Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Fabiola, R.; Jacobsson, B. A Report: The Definition and Classification of Cerebral Palsy April 2006 Peter Rosenbaum (Definition Panel Chair) MD. Available online: https://wzukusers.storage.googleapis.com/user-32163818/documents/5a917ab76f3ffKJVJWSW/A report the definition CP.pdf (accessed on 17 January 2019).
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral palsy. Nat. Rev. Dis. Primers 2016, 2, 15082.
- Ruiz Brunner, M.d.l.M.; Cuestas, E. La construcción de la definición parálisis cerebral: Un recorrido histórico hasta la actua-lidad. Rev. Fac. Cienc. Med. Cordoba 2019, 76, 113.
- Gulati, S.; Sondhi, V. Cerebral Palsy: An Overview. Indian J. Pediatr. 2017, 85, 1006–1016.
- Ganesh, G.; Das, S. Evidence-based approach to physical therapy in cerebral palsy. Indian J. Orthop. 2019, 53, 20–34.
- Hasanah, I.; Haikal, Z. The Effects of Music Therapy on Cortisol Levels as a Biomarker of Stress in Children; IntechOpen: Rijeka, Croatia, 2021.
- Nasuruddin, M.G. The Confluence Between Arts and Medical Science—Music and movement therapy for children with Cerebral Palsy. Malays. J. Med. Sci. 2010, 17, 1–4.
- Jackson, N.A. Professional Music Therapy Supervision: A Survey. J. Music Ther. 2008, 45, 192–216.
- Jones, J.D. Songs composed for use in music therapy: A survey of original songwriting practices of music therapists. J. Music Ther. 2006, 43, 94–110.
- Correa, A.G.D.; Ficheman, I.K.; do Nascimento, M.; Lopes, R.d.D. Computer Assisted Music Therapy: A Case Study of an Aug-mented Reality Musical System for Children with Cerebral Palsy Rehabilitation. In Proceedings of the 2009 Ninth IEEE International Conference on Advanced Learning Technologies, Riga, Latvia, 15–17 July 2009; pp. 218–220. Available online: http://ieeexplore.ieee.org/document/5194207/ (accessed on 18 January 2019).
- Dileo, C.; Bradt, J.; Grocke, D.; Magill, L. Music interventions for improving psychological and physical outcomes in cancer patients. In Cochrane Database of Systematic Reviews; Dileo, C., Ed.; John Wiley & Sons, Ltd: Chichester, UK, 2008.
- Li, J.; Zhou, L.; Wang, Y. The effects of music intervention on burn patients during treatment procedures: A systematic review and meta-analysis of randomized controlled trials. BMC Complement. Altern. Med. 2017, 17, 158.
- Clark, I.; Taylor, N.; Baker, F. Music interventions and physical activity in older adults: A systematic literature review and meta-analysis. J. Rehabil. Med. 2012, 44, 710–719.
- Mendes, M.V.d.S.; Cavalcante, S.A.; de Oliveira, E.F.; Pinto, D.M.R.; Barbosa, T.S.M.; de Camargo, C.L.; Mendes, M.V.d.S.; Cavalcante, S.A.; de Oliveira, E.F.; Pinto, D.M.R.; et al. Crianças com Retardo do Desenvolvimento Neuropsicomotor: Musicoterapia Promovendo Qualidade de Vida. Rev. Bras. Enferm. 2015, 68, 797–802. Available online: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672015000500797&lng=pt&tlng=pt (accessed on 18 January 2019).
- Wigram, T. The effects of Vibroacoustic Therapy on Clinical and Non-Clinical. 1996. Available online: http://www.wfmt.info/Musictherapyworld/modules/archive/stuff/papers/Wigram.pdf (accessed on 28 January 2019).
- Gullickson, T. The Art and Science of Music Therapy: A Handbook. PsycCRITIQUES 1997, 42, 483. Available online: https://books.google.es/books?hl=en&lr=&id=BQpGAQAAQBAJ&oi=fnd&pg=PA194&dq=Bean,+J.+(1995).+Music+therapy+and+the+child+with+cerebral+palsy:+Directive+and+nondirective+intervention.+In+T.Wigram,+B.Saperston,+%26+R.West+(Eds.)+The+Art+and+Science+of+Music+ (accessed on 28 January 2019).
- Jesús Tiburcio Jiménez, J. Didgeridoo as an Accompanying Instrument in Physiotherapy Sessions with Children Suffering Cerebral Palsy; Artseduca. Universidad Jaume I de Castellon: Castellon, Spain, 2019; pp. 163–189.
- Bean, J.; Oldfield, A. Pied Piper: Musical Activities to Develop Basic Skills; Jessica Kingsley Publishes: London, UK, 2001; 91p, Available online: https://books.google.es/books?hl=es&lr=&id=fxsvXEKQcyEC&oi=fnd&pg=PA1&dq=Bean,+J.,+%26+Oldfield,+A.+Pied+Pieper:+Musical+Activities+to+Develop+Basic+Skills.+2+nd+ed.+London.+Jessica+Kingsley+Publishers.+2001.&ots=4GFiq7o11v&sig=w2OPoDcPxuOSCai_nZTXthSBXKM#v=onepage&q&f=false (accessed on 18 January 2019).
- Jonsson, A.-S. Functionally Oriented Music Therapy (FMT) as a Method of Improving Children’s Ability to Function at School. 2014. Available online: http://www.diva-portal.org/smash/record.jsf?pid=diva2%3A715413&dswid=1496 (accessed on 18 January 2019).
- Hatampour, R.; Zadehmohammadi, A.; Masoumizadeh, F.; Sedighi, M. The effects of music therapy on sensory motor functions of multiple handicapped People: Case study. Procedia Soc. Behav. Sci. 2011, 30, 1124–1126.
- Lathom, W. Application of Kodaly Concepts in Music Therapy. J. Music Ther. 1974, 11, 13–20.
- Darrow, A.-A. American Music Therapy Association. Introduction to Approaches in Music Therapy; American Music Therapy Association: Silver Spring, MD, USA, 2008; p. 190. Available online: https://eric.ed.gov/?id=ED504537 (accessed on 18 January 2019).
- Chesky, K.S.; Russell, I.J.; Lopez, Y.; Kondraske, G.V. Fibromyalgia Tender Point Pain: A Double-Blind, Placebo-Controlled Pilot Study of Music Vibration Using the Music Vibration Table™. J. Musculoskelet. Pain 1997, 5, 33–52.
- Conklyn, D.; Stough, D.; Novak, E.; Paczak, S.; Chemali, K.; Bethoux, F. A Home-Based Walking Program Using Rhythmic Auditory Stimulation Improves Gait Performance in Patients with Multiple Sclerosis: A Pilot Study. Neurorehabilit. Neural Repair 2010, 24, 835–842.
- Marrades-Caballero, E.; Santonja-Medina, C.S.; Sanz-Mengibar, J.M.; Santonja-Medina, F. Neurologic music therapy in upper-limb rehabilitation in children with severe bilateral cerebral palsy: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2019, 54, 866–872.
- Peng, Y.-C.; Lu, T.-W.; Wang, T.-H.; Chen, Y.-L.; Liao, H.-F.; Lin, K.-H.; Tang, P.-F. Immediate effects of therapeutic music on loaded sit-to-stand movement in children with spastic diplegia. Gait Posture 2011, 33, 274–278.
- Thaut, M.H. Neural Basis of Rhythmic Timing Networks in the Human Brain. Ann. N. Y. Acad. Sci. 2003, 999, 364–373. Available online: https://pubmed.ncbi.nlm.nih.gov/14681157/ (accessed on 8 July 2021).
- Santonja Medina, C.S. La Musicoterapia de Neurorrehabilitación Como Conector Entre el Movimiento, Las Emociones y la Cognición en Parálisis Cerebral de Tipo Severa. 2017. Available online: https://dialnet.unirioja.es/servlet/tesis?codigo=155096&info=resumen&idioma=SPA (accessed on 8 December 2020).
- Alves-Pinto, A.; Turova, V.; Blumenstein, T.; Lampe, R. The Case for Musical Instrument Training in Cerebral Palsy for Neurorehabilitation. Neural Plast. 2016, 2016, 1–9.
- Jiménez-Palomares, M.; Rodríguez-Mansilla, J.; González-López-Arza, M.V.; Rodríguez-Domínguez, M.T.; Prieto-Tato, M. Beneficios de la musicoterapia como tratamiento no farmacológico y de rehabilitación en la demencia moderada. Rev. Esp. Geriatr. Gerontol. 2013, 48, 238–242.
- Zhang, S.; Liu, D.; Ye, D.; Li, H.; Chen, F. Can music-based movement therapy improve motor dysfunction in patients with Par-kinson’s disease? Systematic review and meta-analysis. Neurol. Sci. 2017, 38, 1629–1636.
- Zhou, Z.; Zhou, R.; Wei, W.; Luan, R.; Li, W. Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: A systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 937–951. Available online: https://pubmed.ncbi.nlm.nih.gov/33517767/ (accessed on 30 July 2021).
- Jia, C.; Zhang, H.; Ni, G.; Zhang, Y.; Su, B.; Xu, X. Spasmodic hemiplegia after stroke treated with scalp acupuncture, music therapy and rehabilitation: A randomized controlled trial. Chin. Acupunct. Moxibustion 2017, 37, 1271–1275.
- Efraimidou, V.; Tsimaras, V.; Proios, M.; Christoulas, K.; Giagazoglou, P.; Sidiropoulou, M.; Orologas, A. The Effect of a Music and Movement Program on Gait, Balance and Psychological Parameters of Adults with Cerebral Palsy. J. Phys. Educ. Sport 2016, 16, 1357–1364. Available online: www.efsupit.ro (accessed on 18 January 2019).
- Kwak, E.E. Effect of Rhythmic Auditory Stimulation on Gait Performance in Children with Spastic Cerebral Palsy. J. Music Ther. 2007, 44, 198–216.
- Kim, S.J.; Kwak, E.E.; Park, E.S.; Lee, D.S.; Kim, K.J.; Song, J.E.; Cho, S.-R. Changes in gait patterns with rhythmic auditory stimulation in adults with cerebral palsy. NeuroRehabilitation 2011, 29, 233–241.
- Kim, S.J.; Kwak, E.E.; Park, E.S.; Cho, S.-R. Differential effects of rhythmic auditory stimulation and neurodevelopmental treat-ment/Bobath on gait patterns in adults with cerebral palsy: A randomized controlled trial. Clin. Rehabil. 2012, 26, 904–914. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22308559 (accessed on 18 January 2019).
- Hamed, N.S. Pedometer-based gait training in children with spastic hemiparetic cerebral palsy: A randomized controlled study. Clin. Rehabil. 2011, 25, 157–165. Available online: http://www.sagepub.co.uk/journalsPermissions.nav (accessed on 19 January 2020).
- Wang, T.-H.; Peng, Y.-C.; Chen, Y.-L.; Lu, T.-W.; Liao, H.-F.; Tang, P.-F.; Shieh, J.-Y. A Home-Based Program Using Patterned Sensory Enhancement Improves Resistance Exercise Effects for Children with Cerebral Palsy. Neurorehabilit. Neural Repair 2013, 27, 684–694.
- Torres, M.R.; Ortiz, J.A.; Codirector, O.; Enrique, Á.; Restrepo, R. Efectos de un Programa de Musicoterapia con Aplicación de RAS y TIMP, en las Funciones Motoras de 3 Niños Diagnosticados con Parálisis Cerebral con Edades entre 5 y los 10 años, que Asisten a la Asociación Aconiño en Bogotá. Estudios de Caso. 2016. Available online: https://repositorio.unal.edu.co/handle/unal/58355 (accessed on 6 December 2020).
- Martínez Morga, M.; Martínez, P.S. Plasticidad neural: La sinaptogénesis durante el desarrollo normal y su implicación en la discapacidad intelectual. Rev. Neurol. 2017, 64, S45.
More
Information
Subjects:
Acoustics
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Revisions:
2 times
(View History)
Update Date:
25 Nov 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




