Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Maria Jesus Vinolo-Gil and Version 2 by Rita Xu.
Cerebral palsy (CP) is defined as a group of permanent disorders in the development of movements and postures, provoking limitations on activity, attributed to non-progressive disturbances that occurred in the development of the foetal or infant brain.
- cerebral palsy
- music-therapy
- physiotherapy
- motor function
1. Introduction
Cerebral palsy (CP) is defined as a group of permanent disorders in the development of movements and postures, provoking limitations on activity, attributed to non-progressive disturbances that occurred in the development of the foetal or infant brain. Motor disorders of CP are often accompanied by alterations to sensation, perception, cognition, communication, and behaviour due to epilepsy and secondary musculoskeletal problems [1].
CP affects approximately 1 out of 500 new-borns, with an estimated prevalence of 17 million people worldwide [2], which establishes it as the most common motor disability during childhood [3].
Physical therapy (PT) plays a key role in its treatment through several therapeutic interventions that achieve improved physiological and functional outcomes [4]. Based on recent evidence, current goal-oriented functional approaches are considered effective, although more research is needed to determine the best ways to achieve even more improved functional outcomes in children with CP [5]. Music therapy (MT) might be a new avenue that, in combination with PT, would help to improve motor function in patients with CP [6][7][6,7].
In the words of Jackson and his collaborators, "Music therapy is a paramedical specialization based scientifically on clinical–therapeutic methods and establishes a working methodology and a series of techniques with the objective of promoting positive cognitive, physical, mental, and social changes in individuals with health or behaviour disorders" [8]. Through the use of rhythmic, harmonic, and melodic sounds by means of improvisations, musical compositions, reproduction of sounds, and other techniques, an improvement in communication, expression, organization, learning, and mobilization is achieved by also obtaining a rehabilitative effect [9][10][9,10].
Several studies have demonstrated the positive effect of MT on numerous conditions, such as cancer [11], burns [12], and cognitive deterioration [13], on diverse factors, such as breathing, blood flow, heart rate, blood pressure, acceleration of the metabolism, and oxygenation and on different emotional states, such as anguish, anxiety, tension, stress, and fear [14]. MT has also been used in people with CP in order to determine its influence on muscle tone [15][16][17][15,16,17].
Bean and Oldfield (2001) performed a series of exercises for the development of specific movements in children with CP, creating musical activities for the development of functional skills [18]. This active work was also used by Lasse Hjelm, the author of the functionally oriented music therapy (FMT) method, who commented: "music therapy focused on human body functions is often indicated in motor impairments and is highly applicable in people with CP” [19]. Another example of the application of active musical activities for the development of motor skills in people with CP was carried out by Hatampour and his collaborators [20].
In terms of functional capacity, certain authors have advanced the traditional concepts of music and education, such as Richardson, who adjusted Zoltán Kodály’s methodology for children with disabilities, using more concrete techniques that helped the development of motor skills, such as manual signal tests [21], an adaptation of Orff Schulwerk’s methodology, or the Suzuki method [22]. Significant results [23] were also found through the use of music to motivate patients during physiotherapy sessions.
At the beginning of the 1990s, the first clinical collaborations between music therapists and physiotherapists began, leading to the beginnings of neurological music therapy (NMT). NMT is an evidence-based system of clinical interventions or techniques for retraining the sensory–motor area, speech and language, and cognitive functions that may be impaired following an injury of neurological origin [24]. Additionally, it can promote neuroplasticity by motor control learning through therapeutic instrumental music performance (TIMP) [25].
Other music therapy techniques have also been used, such as patterned sensory enhancement (PSE), which uses musical elements to translate the components of a movement into sound patterns in order to give temporal, spatial, and force cues about the movement to improve its execution [26], or rhythmic auditory stimulation (RAS), which uses rhythmic sensory stimuli to improve motor control in rehabilitation [27].
People with CP have affected gross motor function and manual function but may be able to integrate rhythm and movement and use musical instruments in their therapy, taking advantage of all the benefits of this technique for neuroplasticity and motor control [28]. Alves-Pinto et al. (2015) showed that functional rehabilitation in people with CP is not due to chance, since MT introduces changes in the internal mechanisms underlying motor function [29].
Several studies can also be found on elderly people [30], patients with Parkinson’s [31][32][31,32], or patients with cerebrovascular accidents [33] that analyse how a combination of PT and MT achieves improvements in motor function. However, there are few trials in which they are used for the treatment of CP [28].
2. Selection of Studies
The search strategy was carried out on 17 databases, from which we obtained 151 articles. Of these, 5 belonged to Web of Science, 5 to PubMed, 3 to CINALH, 1 to Medline, 6 to PEDro, 44 to ProQuest, 22 to Ovid, 6 to Scopus, 3 to Cochrane Plus, 1 to ABI Inform/ProQuest, 18 to JSTOR, 0 to EBSCO, 26 to ScienceDirect, 1 to Emerald, 0 to PROSPERO, 0 to SSRN, 8 to PsycInfo, 2 to TESEO, 0 to OpenGrey, 1 to Grey Literature Database, and 1 to Music Therapy Conference Proceedings.
After filtering by eligibility criteria, focusing on the efficacy of the treatment on cerebral palsy to improve the motor function through MT and PT and eliminating duplicate articles, 30 documents were obtained. After reading them, eight articles were judged to be valid for the review. The main steps related to the bibliographic search phase are presented in Figure 1 using a flowchart.
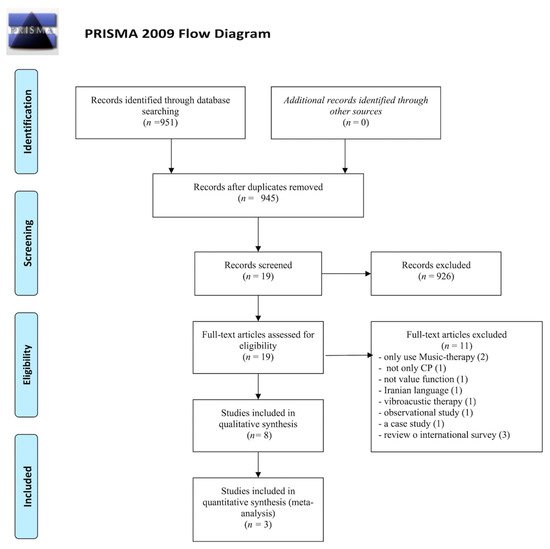
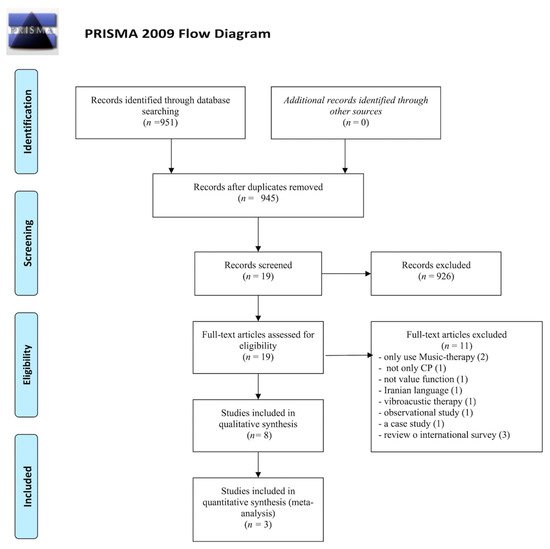
Figure 1. Information flowchart of the different phases of the systematic review, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
3. Study Design and Characteristics
Eight studies with a total of 234 participants diagnosed with cerebral palsy aged between 4 [25] and 52 [34][40] years were included in this systematic review. The main findings of the systematic review are presented in Table 1. The type of cerebral palsy, the average age of the patients, the “motor function” outcome, as well as the most relevant results are described in Table 1. Table 2 shows intervention details.
Table 1.
Results of studies included within the systematic review.
| Study | N Age/Mean (SD) Age Range (Years) |
Type of PCI | “Motor Function” Outcome | t/w min Weeks |
Results | ||||
|---|---|---|---|---|---|---|---|---|---|
| Kwak [35] (NRCT) | Kwak [41] (NRCT) |
n | = 25 Con: 9 Exp1: 9 Exp2: 7 6–20 |
Spastic cerebral palsy | |||||
| Chailey skill levels | |||||||||
| 16 weeks | |||||||||
| Improved Chailey Levels of Ability ( | |||||||||
| p | = 0.002): “activities” | section ( | p | = 0.007), “arm and hand position” section ( | p | = 0.027) and locomotor stages ( | p | = 0.008). Persisted for 4 months. |
SD: standard deviation; Con: control group; Exp: experimental group; NRCT: nor randomized controlled trial; RCT: randomized controlled trial; GDI: step deviation index; NA: not available; NDT: neurodevelopmental therapy/Bobath; t/w: times per week; MRI: maximum repetition; Ri: internal rotation; Re: external rotation; STS: sit to stand test; COM: centre of mass; NJI: normalized jerk index; TUG: timed up and go; MWT: 10-meter walk test; BBS: Berg’s balance scale; GMFM: gross motor function measure; PEDI: paediatric evaluation of disability inventory; UL: upper limb.
Table 2.
Type of intervention.
| Study | Intervention | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kwak et al. [35] | Kwak et al. [41] | Con: conventional gait training with a physical therapist Exp1: gait training + RAS A music therapist provided verbal instructions. A drum was used to emphasize the beat. A computer speaker system played the prescribed music (4/4 m, 105–120 beats per minute). The tempo of the music was increases by 10% (2nd week) and 15% (3rd week). Depending on individual needs, the physical therapist and music therapist developed muscle strengthening exercises using PSE and TIMP. | 14-meter walkway Gait parameter (cadence, stride length, velocity, symmetry) |
5 t/w 30 min 3 weeks |
Exp2: gait training + self-guided RAS A tape and instructions were given. The researcher demonstrated how they could feel the beat and how they could walk with the prescribed music for 30 min of daily self-training. | Exp1: improved stride length ( | t | = −3109, | p | = 0.014), velocity ( | t | = −3029, | p | = 0.016) and symmetry ( | t | = −3029, | p | = 0.016) | |||||||||
| Kim et al. [36] (NRCT) | Kim et al. [42] (NRCT) |
||||||||||||||||||||||||||
| Kim et al. [36] | Kim et al. [42] | n | = 44 Con: 30 healthy people Exp: 14 with CP 25.64 ± 7.31 |
-Gait training without RAS -Gait training with RAS 1. A subject walked barefoot along a 10 m walkway three times at the individual’s preferred walking speed without RAS. 2. Walking cadence (steps/min) was calculated based on the gait parameters in Step 1. 3. The tempo of metronome beats (bpm) was set to participant’s cadence obtained in Step 2. 4. RAS was provided by the music therapists, playing a simple rhythm pattern using chord progression on a keyboard with metronome beats. 5. The same chord pattern was repeated providing a continuous timing cue and period sequence for 1–2 min to help a subject adapt to RAS immediately. | Bilateral spasticity |
Temporal and kinematic gait parameters GDI Asymmetry |
1 session | 6. A subject walked 10 m three times again with RAS. | Kinematic changes of pelvic and hip movement, and GDI was significantly changed with RAS ( | p | < 0.05) Improved temporospatial asymmetry in household ambulators |
||||||||||||||||
| Kim et al. [37] (RCT) | Kim et al. [43] (RCT) |
||||||||||||||||||||||||||
| Kim et al. [37] | Kim et al. [43] | n | = 39 Con: 19 27.3 (2.5) Exp: 20 27.3 (2.4) |
Con: NDT. Gait training Exp: Gait training with RAS 1. A participant walked barefoot along the walkway (10 m) three times, at the individual’s preferred walking speed, before rhythmic auditory stimulation application. 2. The individual’s cadence (steps/min) was calculated based on the gait parameters in Step 1. 3. The tempo of metronome beats (bpm) was set to the participant’s cadence obtained in Step 2. | Bilateral spasticity |
4. RAS was provided by music therapists, who played a simple rhythm pattern synchronized with the beats of a metronome, using chord progressions on a keyboard. | Temporal and kinematic parameters of the gait GDI |
3 t/w 30 min 3 weeks |
Exp: improved cadence, velocity, step length, stride length ( | p | < 0.05), previous pelvic tilt, hip flexion ( | p | < 0.05), GDI ( | p < | 0.05) Con: improved Ri and Re ( | p | < 0.05). | ||||||||||
| Peng et al. [26] (RCT) |
|||||||||||||||||||||||||||
| Peng et al. [26] | n | = 23 8.7 (2) Con: NA Exp: NA |
Spastic diplegia |
Kinematic parameters Movement time NJI Flex trunk angles COM address |
1 session | Maximum knee extension power ( | Con: STS with 50% of 1RM without PSE, 8 reps | p | = 0.009), >total extension power ( | p | = 0.015), >COM fluidity ( | p | = 0.01), <movement time ( | p | = 0.003), and remained without music | ||||||||||||
| Exp: STS with 50% of 1RM, 5 reps with PSE and 3 reps without PSE | The individualized PSE music was composed by a music therapist with an electronic keyboard using GarageBand software on a Mac Mini at an intensity of 75 dBA, varying the tempo, harmonies, metre. |
Hamed et al. [38] (RCT) | Hamed et al. [44] (RCT) |
n | = 30 | ||||||||||||||||||||||
| Hamed et al. [38] | Hamed et al. [44] | Con: 15 7.07 (0.82) Exp: 15 Exp: 7.03 (0.76) |
Con: NDT + usual gait training -NDT: approximation of the upper and lower limbs in a regular and rhythmic manner, facilitation of righting, equilibrium, and protective reactions, training of postural stability and equal weight shift, stretching and strengthening exercises of the upper and lower limbs and back muscles. -Gait training program without pedometer Exp: same + pedometer-based gait training programme. A talking pedometer was fastened to a belt or waistband. It played seven melodies while walking or jogging, and the tempo synchronized with walking speed. The activities included walking forward, backward, and sideways | Spastic hemiparesis |
between parallel bars, on a walking line, and on a balance beam; stepping forward on a stepper (stairs); and training of walking with different obstacles and on different floor surfaces. | Running speed Stride length Cadence Cycle time |
5 t/w 60min 12 weeks |
Exp: improved velocity ( | p | < 0.0001) and cadence ( | p | < 0.008) Exp: velocity 0.68 ± 0.09 m/s Con: 0.420 ± 11 m/s for control group ( | t | = 6.2) ( | p | < 0.0001) Exp: cadence 124.3 ± 4.3 steps/min Con: 128.7 ± 4.1 steps/min ( | t | = 2.8) ( | p | < 0.008) | |||||||
| Efraimidou et al. [34] (RCT) | Efraimidou et al. [40] (RCT) |
||||||||||||||||||||||||||
| Efraimidou et al. [34] | Efraimidou et al. [40] | n | = 10 Con: 5 38.80 (12.28) Exp: 5 35.20 (13.01) |
Con: ball and puck training program Exp: The program included gait and balance with music exercises according to RAS. | Spastic hemiparesis |
-Warm-up period: stretching exercises accompanied with music tracks of 4/4 m and a tempo of 70 beats per minute -Main part: Participants walked to the rhythm veer (music tracks of 4/4, 90 beats/min). Then they continued to move with pace in a straight line for a distance of 10 m with forward, backward, right, and left steps, as well as standing on one leg with change for some seconds. -Cool-down: relaxation exercises, breathing and music (4/4, 70 beats/min) | TUG Lift and walk test MWT Berg’s Scale Static and dynamic balance with EPS platform |
2 t/w 50 min 8 weeks |
Exp: improvement in gait and balance ( | p | ≤ 0.05) Improvement in gait time (s) (F1,8 = 13.60, | p | = 0.006, η | 2 | = 0.630), in normal gait speed (m/s) (F1,8 = 8.53, | p | = 0.019, η | 2 | = 0.516), but not in fast gait speed (m/s) (F1,8 = 4.84, | p | = 0.059, η | 2 | = 0.377) Statistically significant differences in intervention group between the two measurements regarding static and dynamic balance score ( | t | = −8.63, df = 4, | p | = 0.001) |
| Wang et al. [39] (RCT) | Wang et al. [45] (RCT) |
||||||||||||||||||||||||||
| Wang et al. [39] | Wang et al. [45] | n | = 45 Con: 24 9 (1.99) Exp: 21 8.98 (2.61) |
Spastic diplegia |
GMFM PEDI STS |
Con: Loaded STS exercise with weighted body vest. 3 sets: | 3t/w 6 weeks |
-1st and 3rd: load at 20% of 1RM, 10 reps | Exp: improvements in gross motor function capacity ( | p | < 0.05) maintained 6–12 weeks ( | p | < 0.13). No improvements in daily functioning, strength, and walking speed. |
||||||||||||||
| -2nd: 50% of 1RM until fatigue Exp: To prescribe the PSE music, loaded STS 50% of 1RM, 6 reps. The fastest three STS movements were selected as references to prescribe PSE music using an electronic keyboard and GarageBand software on a Mac (Apple Inc., Cupertino, CA, USA). Music provided cueing of the movement period. Caregivers supervised. Every 2 weeks, the music therapist adjusted musical elements according to the individual’s needs. |
Marrades-Caballero et al. [25] (crossover) |
n | |||||||||||||||||||||||||
| Marrades-Caballero et al. [25] | = 18 10 (6) |
Con: physiotherapy (no technique specified), 1 t/w Exp: NMT sessions by two music therapists. The music was live and customized according to each patient. Small percussion instruments, Spanish guitar, keyboard, and drums were played. Two types of activities: -At the beginning, patients chose and played the musical instruments using their own movement strategies (hitting, rubbing, crashing) to generate rhythmic music patterns. Music therapists played along. | Severe bilateral |
-Task-specific training with varied and incremental levels of difficulty. Music therapists composed small pieces of music testing different music parameters trying to trigger forearm pronation and supination, elbow flexion and extension, and shoulder flexion. The activities were performed in a prone position or sitting in their wheelchairs and were aimed at challenging upper-limb movements and head and trunk control. | UL functionality |
Con: control group; Exp: experimental group; NDT: neurodevelopmental therapy/Bobath; RAS: rhythmic auditory stimulation; t/w: times per week; MRI: maximum repetition; STS: sit to stand test; Rep: repetitions; PSE: patterned sensory enhancement; TIMP: therapeutic instrumental music performance; NMT: neurologic music therapy.
Different types of CP were studied: spastic diplegia [26][39][26,45], spastic hemiplegia [34][38][40,44], bilateral spasticity [36][37][42,43], spastic CP [35][41], and severe bilateral CP [25].
With respect to the motor function outcome, the following were analysed: kinematic parameters and temporal data (such as cadence, velocity, step length, trunk flexion angles, centre of mass movement, and symmetry) [26][35][37][38][26,41,43,44], GDI step deviation index [36][37][42,43], normalized jerk index (NJI) [26], lift and walk test [34][40], 10 meter gait test [34][40], Berg balance scale [34][40], TUG [34][40], balance [34][40], gross motor function measure (GMFM) [39][45], paediatric evaluation of disability inventory (PEDI) [39][45], STS [39][45], upper limb functionality [25], Chailey’s ability levels, and Communication Function Classification System (CFCS) [25].
As for the interventions used, the studies analysed present different characteristics in terms of the performance within the treatment sessions. The differences reside in previous trainings, duration of treatment or session, number of sessions, and number of participants, all of them variables for measuring function and performance of the techniques, either by repetition or by working time.
Working sessions during treatment vary across studies, being at least one session [26][36][26,42], and at most 60 sessions [38][44], with studies normally lasting from 3 to 12 weeks. The duration of the sessions varied between 30 min [35][37][40][41,43,46] and 60 min [38][44], and the frequency varied between twice a week [34][40] and five times a week [35][38][41,44].
In terms of PT techniques, the most frequent was gait retraining [35][36][38][41][41,42,44,47], followed by neurodevelopmental therapy (NDT) [25][37][38][25,43,44]; two articles used resistance techniques [26][39][26,45], and one used technique for sports training with a ball and a disc [34][40].
With respect to MT techniques, rhythmic auditory stimulation (RAS) was used in three of the trials [34][36][37][40,42,43], sensory enhancement pattern (PSE) was used in another two [26][39][26,45], a pedometer with music was also used [38][44], and the last one was based on a programme of instrumental music performance using neurological music therapy (TIMP) [25]. Five articles used an electronic keyboard [25][26][36][37][39][25,26,42,43,45].
Some cooperative work has been carried out between specialized physiotherapists and music therapists to adapt the different musical pieces to the patients’ characteristics so that they could achieve the goals proposed.
As regards the statistical evaluation in the studies analysed, for kinematic parameters of the pelvis and hip joint evaluated in the sagittal plane, Kim et al. [36][42] found significant changes with RAS: anterior pelvic tilt at initial contact was significantly ameliorated by RAS (15.09 ± 9.78 degrees, vs. 17.27 ± 7.64 degrees without RAS; t = 2.874, p = 0.008 by paired t-test), and angles of maximal and minimal hip flexion during a gait cycle were both significantly reduced with RAS (49.20 ± 10.99 degrees to 47.82 ± 10.87 degrees in maximal flexion, t = 2.373, p = 0.025; 9.17 ± 10.99 degrees to 7.52 ± 11.88 degrees in minimal flexion, t = 2.468, p = 0.020). However, in a later study [35][41], RAS aggravated maximal internal rotation in the transverse plane (p < 0.05). With respect to the findings in the knee, Peng et al. [26] achieved a small but significant difference in peak knee extensor power per limb (p = 0.04), with an effect size of 0.23, and total extensor power per limb, with p = 0.03 and an effect size of 0.35.
About gait tests, Efraimidou et al. [34][40] revealed a statistically significant main effect of time or group in gait time (s) (F1,8 = 13.60, p = 0.006, η2 = 0.630) in the TUG-test and on normal gait speed (m/s) (F1,8 = 8.53, p = 0.019, η2 = 0.516), but not on fast gait speed (m/s) (F1,8 = 4.84, p = 0.059, η2 = 0.377) in 10MWT. The ANOVA repeated measurement test revealed a statistically significant main effect of time or group on Berg Balance score (F1,8 = 18.01, p = 0.003, η2 = 0.692) in BBS.
Previously, Hamed et al. [38][44] noted that velocity was 0.68 ± 0.09 m/s (0.26 ± 0.07 change score) for the study group and 0.42 ± 0.11 m/s (0.060 ± 0.05 change score) for the control group (t = 6.2) (p < 0.0001); stride length was 0.52 ± 0.07 metres vs. 0.34 ± 0.07 metres for control (t = 6.25) (p < 0.0010); however, cadence was much less significant at 124.3 ± 4.3 steps/min (−5.8 ± 2.1 change score) for the study group and 128.7 ± 4.1 steps/min (−0.86 ± 0.05 change score) for the control group (t = 2.8) (p < 0.008). Meanwhile, Kwak et al. [35][41] observed increased stride length (t = −3.109, p = 0.014) and velocity (t = −3.029, p = 0.016) in the therapist-guided training group.
On the other hand, Wang [39][45] showed GMFM score means at four time points and observed in both groups significant main time effects of GMFM scores in Dimensions D (F = 8.9–32.2, p ≤ 0.005) and E (F = 6.4–16.4, p ≤ 0.016) and the Goal Dimension (F = 12.7–28.3, p ≤ 0.001). Additionally, significant group by time interactions were found in Dimension D at T1 (after 6 weeks of training) (p = 0.004, mean adjusted difference = 3.6, ES 0.54) and T2 (at 6 weeks) (p = 0.004, mean adjusted difference = 3.8, ES 0.54), with greater improvements in the PSE group than in the no-music group. However, the music effects did not maintain at T3 (at 12 weeks following the end of the training) (p = 0.06, ES 0.34). For the goal score, significant interactions were found at T1 (p < 0.001, ES 0.7), T2 (p = 0.004), ES 0.54, and T3 (p = 0.013, ES 0.46). The Functional Skills Scale scores of the PEDI mobility domain increased in both groups from T0 (at baseline) to T1, T0 to T2, and T0 to T3, resulting in significant main effects of time (F = 9.4–12.6, 0.001 ≤ p ≤ 0.004) [37][43].
Values of STS 1RM increased in both groups, resulting in a significant main effect of time at all time points (F = 11.3–15.6, p ≤ 0.002), but no interaction was found (p = 0.06–0.15) [39][45].
Finally, the only study that did not assess the lower limb, Marrades et al. [25], found significant differences in the Total Chailey Test (p = 0.002), arm and hand position section (p = 0.027), activities (p = 0.007), and locomotor stages (p = 0.008).
