
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Leonidas Palaiodimos | + 2033 word(s) | 2033 | 2021-09-09 08:09:22 | | | |
| 2 | Lindsay Dong | -6 word(s) | 2027 | 2021-10-27 05:02:18 | | |
Video Upload Options
Acute lower extremity proximal deep venous thrombosis (DVT) requires accurate diagnosis and treatment in order to prevent embolization and other complications. Point-of-care ultrasound (POCUS), a clinician performed, and clinician interpreted bedside ultrasound examination has been increasingly used for DVT evaluation mainly in the urgent and critical care setting, but also in the ambulatory clinics and the medical wards.
1. Introduction
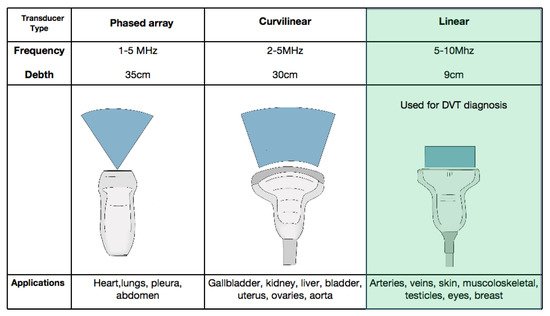
2. Equipment and Current Technology
3. Patient Preparation
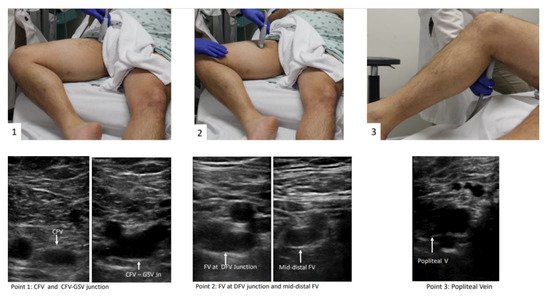
The patient should be positioned supine and the head should be elevated to 30° preferably, which can help blood pooling in the veins of the lower extremities and aid in visualization of the vasculature [15]. Then the examiner should externally rotate the patient’s hip and bend the knee slightly into what is known as the “frog leg” position [15]. This is the most popular position because it enlarges the femoral veins and brings it closer to the field of vision for the plane of the ultrasound probe. In addition, the “frog leg” position allows the examiner to scan the inguinal region and the popliteal fossa without having to reposition the patient [16]. When possible, prone position can help in examining the popliteal veins [17]. The examiner is typically most comfortable standing at the patient’s side, ipsilateral to the extremity being evaluated. When using a cart-based ultrasound machine, it should be positioned within the examiner’s reach at the head of the bed. The bed height should be elevated for examiner comfort [12]. The patient preparation and positioning are depicted in Figure 2.
4. Protocols
There is variability in the definition of POCUS protocols to evaluate for DVT and their names, as well as the levels they include, can be a source of confusion for learners. The two main types of POCUS examinations that have been studied for the diagnosis of DVT are called “2-point” and “3-point” exams, which is somewhat of a misnomer because they both involve scanning more levels or segments of vein than that. Even within 3-point protocols, there is variability in the levels of proximal lower extremity vein included. The term “compression ultrasound” is used historically to refer to bedside ultrasound in B-mode without Doppler. This involves inspection for echogenic thrombus and if a thrombus is not seen, testing for compressibility of the visualized segment of vein with the probe in the transverse orientation [12]. For the purpose of this entry, the term POCUS is used and unless otherwise specified refers to B-mode inspection for thrombus and the compression ultrasound technique.

5. Sensitivity and Specificity
Overall, the existing studies have shown that POCUS has excellent diagnostic accuracy for evaluation of acute proximal DVT. However, it should be emphasized that these studies have significant heterogeneity as far as the setting (ICU, ED, medical ward), as well as the preceding training of the clinicians performing POCUS (resident vs. attending). Therefore, extrapolating these findings to different users with varied training must be undertaken with caution.
6. Pre-Test Probability and D-Dimer
7. Time and Resources
8. Education
9. Limitations
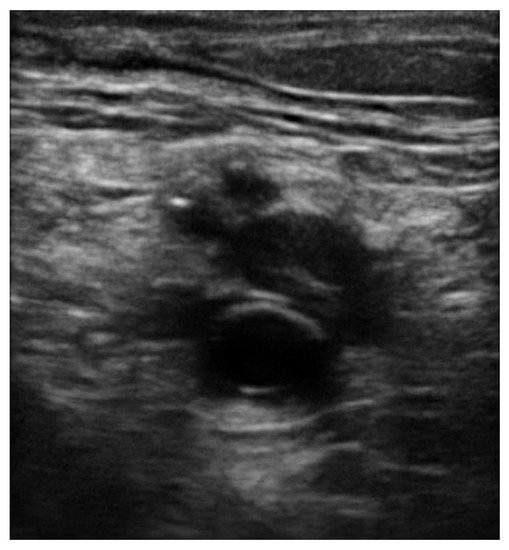
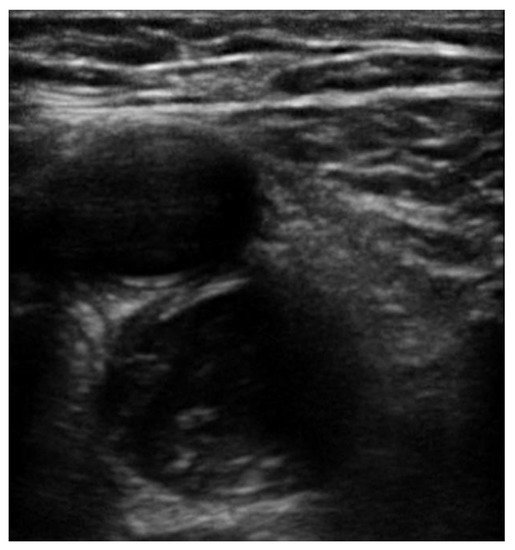
The pooled proportions of the false-negative rate of the 2-point and 3-point POCUS have been estimated around 4% and are similar between the 2 protocols [31][32]. A false negative evaluation for DVT would mean underdiagnosing thrombosis potentially leading to life-threatening pulmonary embolism. The pooled proportions of the false-negative rate of the 2-point POCUS and 3-point POCUS have been estimated around 4% and are similar between the two protocols [31][32]. Whether a full examination for distal DVT is appropriate or is still a debate, there are publications showing that 48% of patient with PE have contemporary isolated distal clots while this percentage for negative PE population is only 12% [33]. Unfortunately, these patients would be considered false negative while performing a standard POCUS protocol instead of a full CUS performed by a radiologist [34][35]. POCUS can also have false positives around 4% as reported by Fischer et al., which can lead to unnecessary anticoagulation treatment and risk of bleeding or other complications [11][36]. There are several potential causes of a false positive POCUS evaluation for DVT worth noting. Superficial thrombophlebitis can be mistaken for DVT, however the major difference is that superficial veins do not accompany arteries while deep veins do [37]. A Baker’s cyst appears as a circular anechoic structure in the popliteal fossa that can resemble a non-compressible vein [38]. Enlarged inguinal lymph nodes can appear similar to a vein with a clot because of their oval structure, anechoic rim with hyperechoic center, but are easy to distinguish from a vein by scanning through to see that the structure is self-contained and even easier when the true CFV and arteries are found in a different fascial plane. Rarely, pseudoaneurysms and groin hematomas can be falsely diagnosed as DVT by non-experienced performers [38][39]. An important technical consideration for POCUS performers learning to evaluate for DVT is knowing how much to compress the vein. If the operator does not apply enough pressure or if the ultrasound probe is not perpendicular to the vein, this can lead to false positives [40]. Another cause of false-positive POCUS examination for DVT is the presence of “rouleaux formation” that is an accumulation of erythrocytes lying over the venous valves represented by spontaneously echogenic blood flow inside the vessel. While rouleaux is a common finding and usually does not have a clinical impact, it is important to highlight that this can also be frequently observed when there is a proximal venous obstruction, and thus a more proximal DVT must be ruled out. In contrast to a real condition of thrombosis, veins with rouleaux formation are compressible [41]. While POCUS can be immensely helpful in the rapid diagnosis of DVT at the bedside, equivocal findings should prompt further evaluation by radiology or a vascular lab-performed duplex ultrasound study.
References
- Heit, J.A. Epidemiology of venous thromboembolism. Nat. Rev. Cardiol. 2015, 12, 464–474.
- Calder, K.K.; Herbert, M.; Henderson, S.O. The mortality of untreated pulmonary embolism in emergency department patients. Ann. Emerg. Med. 2005, 45, 302–310.
- de Valois, J.; van Schaik, C.; Verzijlbergen, F.; van Ramshorst, B.; Eikelboom, B.; Meuwissen, O. Contrast venography: From gold standard to ‘golden backup’ in clinically suspected deep vein thrombosis. Eur. J. Radiol. 1990, 11, 131–137.
- Pomero, F.; Dentali, F.; Borretta, V.; Bonzini, M.; Melchio, R.; Douketis, J.D.; Fenoglioet, L.M. Accuracy of emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: A systematic review and meta-analysis. Thromb. Haemost. 2013, 109, 137–145.
- Burnside, P.R.; Brown, M.D.; Kline, J.A. Systematic review of emergency physician-performed ultrasonography for lower-extremity deep vein thrombosis. Acad. Emerg. Med. 2008, 15, 493–498.
- Kapoor, S.; Chand, S.; Dieiev, V.; Fazzari, M.; Tanner, T.; Lewandowski, D.C.; Nalla, A.; AbdulFattah, O.; Aboodi, M.S.; Shiloh, A.L.; et al. Thromboembolic events and role of point of care ultrasound in hospitalized Covid-19 patients needing intensive care unit admission. J. Intensive Care Med. 2020.
- Patrawalla, P.; Eisen, L.A.; Shiloh, A.L.; Shah, B.J.; Savenkov, O.; Wise, W.; Evans, L.; Mayo, P.H.; Szyld, D. Development and validation of an assessment tool for competency in critical care ultrasound. J. Grad. Med. Educ. 2015, 7, 567–573.
- American College of Emergency Physicians. ACEP emergency ultrasound guidelines—2001. Ann. Emerg. Med. 2001, 38, 470–481.
- Ultrasound guidelines: Emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann. Emerg. Med. 2017, 69, e27–e54.
- Chen, S.; Zhang, D.; Zheng, T.; Yu, Y.; Jiang, J. DVT incidence and risk factors in critically ill patients with COVID-19. J. Thromb. Thrombolysis 2021, 51, 33–39.
- Fischer, E.A.; Kinnear, B.; Sall, D.; Kelleher, M.; Sanchez, O.; Mathews, B.; Schnobrich, D.; Olson, A.P.J. Hospitalist-operated compression ultrasonography: A point-of-care ultrasound study (HOCUS-POCUS). J. Gen. Intern. Med. 2019, 34, 2062–2067.
- Soni, N.J.; Arntfield, R.; Kory, P. Point of Care Ultrasound, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2020.
- Zuker-Herman, R.; Dangur, I.A.; Berant, R.; Cohen Sitt, E.; Baskin, L.; Shaya, Y.; Shiber, S. Comparison between two-point and three-point compression ultrasound for the diagnosis of deep vein throm-bosis. J. Thromb Thrombolysis 2018, 45, 99–105.
- Baker, M.; Anjum, F.; dela Cruz, J. Deep Venous Thrombosis Ultrasound Evaluation; StatPearls Publishing: Treasure Island, FL, USA, 2021.
- Shiloh, Lower Extremity Deep Venous Thrombosis. In Point of Care Ultrasound; Soni, N.; Arntfield, R.; Kory, P. (Eds.) Elsevier Saunders: Philadelphia, PA, USA, 2015; pp. 21–213.
- Read, H.; Holdgate, A.; Watkins, S. Simple external rotation of the leg increases the size and accessibility of the femoral vein. Emerg. Med. Australas. 2012, 24, 408–413.
- Koksoy, C.; Cetinkaya, O.A. Popliteal access in the supine position for endovenous management of deep vein thrombosis. EJVES Short Rep. 2020, 46, 5–8.
- Adhikari, S.; Zeger, W.; Thom, C.; Fields, J.M. Isolated deep venous thrombosis: Implications for 2-point compression ultrasonography of the lower extremity. Ann. Emerg. Med. 2015, 66, 262–266.
- Farahmand, S.; Farnia, M.; Shahriaran, S.; Khashayar, P. The accuracy of limited B-mode compression technique in diagnosing deep venous thrombosis in lower extremities. Am. J. Emerg. Med. 2011, 29, 687–690.
- Jacoby, J.; Cesta, M.; Axelband, J.; Melanson, S.; Heller, M.; Reed, J. Can emergency medicine residents detect acute deep venous thrombosis with a limited, two-site ultrasound examination? J. Emerg. Med. 2007, 32, 197–200.
- Theodoro, D.; Blaivas, M.; Duggal, S.; Snyder, G.; Lucas, M. Real-time B-mode ultrasound in the ED saves time in the diagnosis of deep vein thrombosis (DVT). Am. J. Emerg. Med. 2004, 22, 197–200.
- Jang, T.; Docherty, M.; Aubin, C.; Polites, G. Resident-performed compression ultrasonography for the detection of proximal deep vein thrombosis: Fast and accurate. Acad. Emerg. Med. 2004, 11, 319–322.
- Kline, J.A.; O’Malley, P.M.; Tayal, V.S.; Snead, G.R.; Mitchell, A.M. Emergency clinician-performed compression ultrasonography for deep venous thrombosis of the lower extremity. Ann. Emerg. Med. 2008, 52, 437–445.
- Needleman, L.; Cronan, J.; Lilly, M.; Merli, G.; Adhikari, S.; Hertzberg, B. Ultrasound for lower extremity deep venous thrombosis: Multidisciplinary recommendations from the Society of Radiologists in Ultrasound Consensus Conference. J. Vasc. Surg. Venous Lymphat. Disord. 2019, 7, 282.
- Bates, S.M.; Jaeschke, R.; Stevens, S.M.; Goodacre, S.; Wells, P.S.; Stevenson, M.D.; Kearon, C.; Schunemann, H.J.; Crowther, M.; Pauker, S.G.; et al. Diagnosis of DVT: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012, 141 (Suppl. 2), e351S–e418S.
- Wells, P.S.; Anderson, D.R.; Rodger, M.; Forgie, M.; Kearon, C.; Dreyer, J.; Kovacs, G.; Mitchell, M.; Lewandowski, B.; Kovacs, M.J. Evaluation of D-Dimer in the diagnosis of suspected deep-vein thrombosis. N. Engl. J. Med. 2003, 349, 1227–1235.
- Qaseem, A.; Snow, V.; Barry, P.; Hornbake, E.R.; Rodnick, J.E.; Tobolic, T.; Ireland, B.; Segal, J.; Bass, E.; Weiss, K.B. Current diagnosis of venous thromboembolism in primary care: A clinical practice guideline from the American Academy of Family Physicians and the American College of Physicians. Ann. Fam. Med. 2007, 5, 57–62.
- Bahner, D.; Blaivas, M.; Cohen, H.; Fox, J.C.; Hoffenberg, S.; Kendall, J.; Langer, J.; McGahan, J.P.; Sierzenski, P.; Tayal, V.S.; et al. AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J. Ultrasound Med. 2008, 27, 313–318.
- Hockberger, R.S.; Binder, L.S.; Chisholm, C.D.; Cushman, J.; Hayden, S.R.; Sklar, D.P.; Stern, S.A.; Strauss, R.W.; Thomas, H.A.; Viravec, D.R. The model of the clinical practice of emergency medicine: A 2-Year update. Ann. Emerg. Med. 2005, 45, 659–674.
- Mumoli, N.; Vitale, J.; Giorgi-Pierfranceschi, M.; Sabatini, S.; Tulino, R.; Cei, M.; Bucherini, E.; Bova, C.; Mastroiacovo, D.; Camaiti, A.; et al. General practitioner-performed compression ultrasonography for diagnosis of deep vein thrombosis of the leg: A multicenter, prospective cohort study. Ann. Fam. Med. 2017, 15, 535–539.
- Zitek, T.; Baydoun, J.; Yepez, S.; Forred, W.; Slattery, D.E. Mistakes and pitfalls associated with two-point compression ultrasound for deep vein thrombosis. West. J. Emerg. Med. 2018, 17, 201–208.
- Bledsoe, J.R.; Woller, S.C.; Stevens, S.M.; Aston, V.; Patten, R.; Allen, T.; Horne, B.D.; Dong, L.; Lloyd, J.; Snow, G.; et al. Management of low-risk pulmonary embolism patients without hospitalization: The low-risk pulmonary embolism prospective management study. Chest 2018, 154, 249–256.
- Ghaye, B.; Noukoua, C.T.; Dondelinger, R.F.; Nchimi, A. Incidence and distribution of lower extremity deep venous thrombosis at indirect computed tomography venography in patients suspected of pulmonary embolism. Thromb. Haemost. 2007, 97, 566–572.
- Elias, A.; Mallard, L.; Elias, M.; Alquier, C.; Guidolin, F.; Gauthier, B.; Viard, A.; Mahouin, P.; Vinel, A.; Boccalon, H. A single complete ultrasound investigation of the venous network for the diagnostic management of patients with a clini-cally suspected first episode of deep venous thrombosis of the lower limbs. Thromb. Haemost. 2003, 89, 221–227.
- Aleva, F.E.; Voets, L.W.L.M.; Simons, S.O.; de Mast, Q.; van der Ven, A.J.A.M.; Heijdra, Y.F. Prevalence and localization of pulmonary embolism in unexplained acute exacerbations of COPD: A systematic review and meta-analysis. Chest 2017, 151, 544–554.
- Roy, P.M.; Penaloza, A.; Hugli, O.; Klok, F.A.; Arnoux, A.; Elias, A.; Couturaud, F.; Joly, L.-M.; Lopez, R.; Faber, L.M.; et al. Triaging acute pulmonary embolism for home treatment by Hestia or simplified PESI criteria: The HOME-PE randomized trial. Eur. Heart J. 2021.
- Naringrekar, H.; Sun, J.; Ko, C.; Rodgers, S.K. It’s not all deep vein thrombosis: Sonography of the painful lower extremity with multimodality correlation. J. Ultrasound Med. 2019, 38, 1075–1089.
- Dihn, V. DVT ultrasound made easy step by step guide. Available online: www.pocus101.com (accessed on 15 April 2021).
- Montorfano, M.A.; Pla, F.; Vera, L.; Cardillo, O.; Nigra, S.G.; Montorfano, L.M. Point-of-care ultrasound and Doppler ultrasound evaluation of vascular injuries in penetrating and blunt trauma. Crit. Ultrasound J. 2017, 9, 1–14.
- Dihn, V. DVT Ultrasound Made Easy: Step-By-Step Guide. 2008. Available online: https://www.pocus101.com/dvt-ultrasound-made-easy-step-by-step-guide/ (accessed on 4 March 2021).
- Blanco, P.; Volpicelli, G. Common pitfalls in point-of-care ultrasound: A practical guide for emergency and critical care physicians. Crit. Ultrasound J. 2016, 8, 1–12.




