
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Shekh Md Mahmudul Islam | + 4582 word(s) | 4582 | 2020-07-23 08:43:45 | | | |
| 2 | Rita Xu | -800 word(s) | 3782 | 2020-07-24 08:27:46 | | |
Video Upload Options
Non-contact vital signs monitoring using microwave Doppler radar has shown great promise in healthcare applications. Recently, this unobtrusive form of physiological sensing has also been gaining attention for its potential for continuous identity authentication, which can reduce the vulnerability of traditional one-pass validation authentication systems. Physiological Doppler radar is an attractive approach for continuous identity authentication as it requires neither contact nor line-of-sight and does not give rise to privacy concerns associated with video imaging.
1. Introduction
Doppler radar has been used in widespread applications, including weather forecasting, vehicle speed measurement, structural health monitoring, and the monitoring of air and sea traffic [1]. This technology has most recently been recognized for promise in healthcare applications though long term unobtrusive physiological monitoring [2][3][4][5][6]. The fundamental Doppler principle is illustrated in Figure 1a, where a reflected signal undergoes a phase shift due to the subtle movement of the chest surface caused by heartbeat and respiration [4][5][6][7][8]. Doppler radar remote life sensing of humans has been widely reported, with proof of concepts demonstrated for various applications [7][8]. This non-contact and non-invasive form of measurement has several potential advantages in medicine, especially for the monitoring of neonates or infants at risk of sudden infant death syndrome [9], adults with sleep disorders [10], and burn victims [11][12]. In addition, separation of respiratory signatures in a multi-subject environment has also been investigated [13][14][15][16]. Moreover, this form of respiration monitoring reduces patient discomfort and distress as electrodes need not be attached to the body. The inherent advantage of this unobtrusive non-contact measurement technique broadens potential applications beyond healthcare to include occupancy sensing [17] and related energy management in smart homes [18][19] and baby monitoring [20].
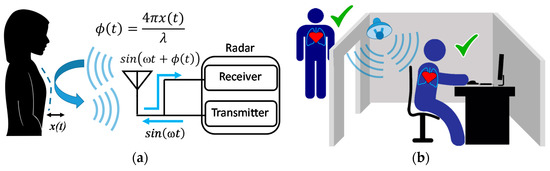
Figure 1. Basic principle of Doppler radar physiological sensing (a), and non-contact continuous identity authentication concept (b). A radar system typically consists of a transmitter and a receiver. When a transmitted signal of frequency ω is reflected its phase changes, φ (t), in direct proportion to the subtle motion.
Growing interest in physiological motion sensing through radar has led to the development of new front-end architectures [20][21], baseband signal processing methods [22], and system-level integration [21][23] to improve detection accuracy and robustness [24]. A review of recent advances in Doppler radar sensors has been reported by Li et al. [25]. One example is the application of this non-invasive technology to monitor infants for sudden infant death syndrome (SIDS) [26][27] which is one of the leading causes of infant mortality. Moreover, Doppler radar has also been implemented to monitor the health and behavior of terrestrial and aquatic animals [28][29][30]. Sleep monitoring is another emerging application where radar alleviates the measurement interference introduced by the conventional use of obtrusive devices such torso straps and or spirometers [31]. A clinical study was performed to comparatively monitor patients suffering from sleep apnea using a radar sensor in conjunction with traditional intrusive sleep monitoring equipment, where the radar was found to provide stand-alone detection of most apnea events, as well as complementary detail to facilitate conventional diagnostics [31]. Furthermore, Food and Drug Administration (FDA) approval for the first commercial use of wireless, non-contact respiratory devices in the Unites States was granted in 2009 [32].
Beyond health sensing, Doppler radar also holds great promise to enhance system security and privacy, particularly in the area of user authentication as illustrated in Figure 1b. Existing system authentication methods predominately employ a one-off, interruptive approach, which authenticates only at the initial log-in of a session [33][34][35][36], with users actively engaging an input device or biometric reader. Such designs are vulnerable to open session exploitations and may interfere with user activity. There have been many studies focused on continuity in user authentication. Several have explored sensing technologies to acquire common physiological traits, including fingerprint [37], palm print [38], and iris [39], used to monitor and authenticate users throughout a session. Recent advancements in wearable sensors and pattern recognition further enable system architects to collect more subtle physiological patterns, such as those associated with electroencephalogram (EEG) [40], finger-vein [41], and gait [42], to verify users implicitly and continuously. Compared to these contact-based solutions, continuous authentication using non-contact, unobtrusive techniques, such as Doppler radar, can further improve system usability and expand the range of applications into domains with known privacy concerns [43][44]. For example, various visible and thermal-based cameras are employed to acquire face and gait features for user verification [45][46][47]. However, image-based approaches suffer from several irreconcilable dilemmas, including a lack of privacy and degraded performance under a low light ambient conditions [48][49]. Alternatively, a solution leveraging unobtrusive radar measurement of cardiopulmonary motion can be immune to such deficiencies and achieve consistent and reliable recognition under privacy-sensitive conditions [49][50][51][52][53][54].
2. Radar-based Continuous Identity Authentication Research
Identity authentication using microwave Doppler radar is gaining attention as it can add an extra layer of security to the vulnerable traditional one-pass validation approach (e.g., fingerprint, password, and facial/iris) [58]. Pattern recognition and unique identification are always challenging for this non-contact technology because of variations in human breathing patterns due to physical activity and emotional stress [55]. As future big data analyses emerge and machine learning algorithms improve, Doppler radar-measured physiological signals can be turned into increasingly useful data and knowledge [58]. In particular, diverse respiratory motion patterns have good potential to be used as biometric identifiers [58][64][65][66][67][68][69][70][71][72].
Identity theft continues to pose everyday challenges for consumers and the associated threat is increased as traditional identity authentication systems are targeted [58][69]. Traditional identity authentication methods, such as fingerprint, password, and facial recognition, all require an initial spot check at the start of user session, which potentially conveys personal information like bank account, social security number, and credit card and social networking account details [72]. In 2018, over 14 million people were victims of identity fraud in the United States [69]. Identity fraud can be significantly reduced by implementing multi-factor authentication systems, which can be further enhanced through integration of unobtrusive continuous radar-based identity authentication [58].
In this section, radar-based sensing authentication is categorized in two different ways, based either on breathing-related features, or heart-based features. Breathing motion is generally periodic, and respiratory-related features can be extracted from the time domain signature of the reflected phase signal and rate information extracted by performing an FFT [4][5][6]. Heartbeat motion is modulated on top of respiratory motion and the larger resulting breathing signal is dominant over the heartbeat signal [4]. This leads to a classical problem in FFT, where the stronger signal at given frequency leaks into other frequencies and can mask a weaker signal at nearby frequencies [4][5]. Generally, the radar captured signal is filtered outside the 0.005–0.5-Hz frequency band for extracting respiration information and 0.8–2 Hz for extracting heartbeat-related information. All the All the radar authentication research cited in this paper is focused on extracting two separate distinguishable features, based on either respiration or heartbeat. Extracting both simultaneously has the potential for stronger authentication; however, such a process may increase computational complexity. Table 1 provides a summary of published work on radar-based non-contact continuous identity authentication considered in this paper. In the next two subsections, details are provided on these two different unique features (breathing and heart, respectively), including related identification demonstrations along with associated challenges for further development. There have also been attempts to use Doppler modulation of WiFi signals to authenticate people and this research is described in the third subsection.
Table 1. Systematic review on radar-based non-contact continuous identity authentication.
| Reference Year of Publication | Hardware (RF Frequency) | Identification Features | Outcome |
|---|---|---|---|
| [52] A. Rahman et al., 2016 | 2.4 GHz Doppler Radar |
|
|
| [58] F. Lin et al., 2017 | 2.4 GHz Doppler Radar |
|
|
| [68] A. Rahman et al., 2018 | 2.4 GHz Doppler Radar |
|
|
| [70] S. M. M. Islam et al., 2019 | 2.4 GHz Doppler Radar |
|
|
| [71] S. M. M. Islam et al., 2020 | 2.4 GHz Doppler Radar |
|
|
| [72] S. M. M. Islam et al., 2020 | 2.4 GHz and 24-GHz Doppler Radar |
|
|
| [73] D. Rissacher et al., 2015 | 2.4 GHz Doppler Radar |
|
|
| [74] K. Shi et al., 2018 | 24 GHz Doppler Radar |
|
|
| [75] T. Okano et al., 2017 | 24 GHz Doppler Radar |
|
|
| [76] P. Cao et al., 2020 | 24 GHz Doppler Radar |
|
|
| [77] J. Zhang et al., 2016 | WiFi router & Laptop |
|
|
| [78] J. Liu et al., 2020 | WiFi router & Laptop |
|
|
2.1. Radar-Based Identity Authentication through Respiration Related Features
One of the first attempts at radar-based identity authentication using breathing pattern was reported by a research group at the University of Hawaii, where they integrated a neural network classifier to recognize individual human beings [52]. In this work they extracted three different respiratory features (peak power spectral density, linear envelop error, and packing density) from respiratory motion measurements, as illustrated in Figure 3. A 2.4 GHz quadrature direct conversion. Doppler radar system was used for this experiment, assembled from coaxial components. A data acquisition system recorded the data and post processing was performed in MATLAB (MathWorks, Natick, MA, USA). Three subjects with similar breathing rates were selected and various features were investigated, such as power spectral density, linear envelop error, and packing density, which convey the breathing energy and air flow profile related phenomena. The research concentrated on using the Levenberg–Marquadrt back propagation algorithm to perform classification [52]. Figure 4 illustrates the experimental setup and reported results for training and applying a neural network classifier to recognition of the Doppler radar physiological measurements [52]. The overall classification accuracy was above 90%, which clearly illustrates that the proposed technique can be effective for this application. However, this work was limited to identifying only three participants. Another issue is that the experiment was entirely focused on measuring a single subject at a time.
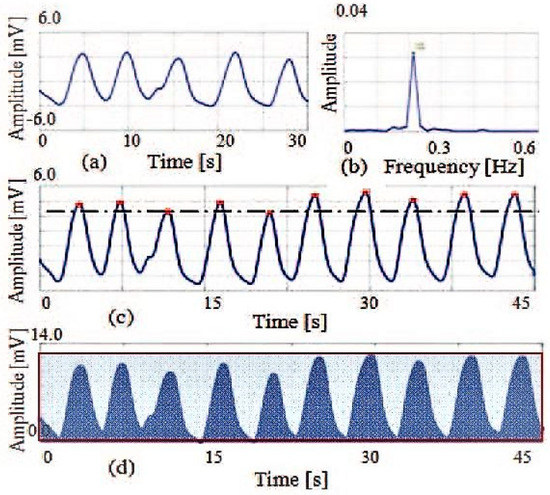
Figure 3. Radar-measured respiratory features from 30 second epochs. Pioneering efforts at recognizing subject identity from radar measured respiratory signals (a) involved extraction of three different features: breathing rate (b), linear envelop error (c), and packing density (d). Linear envelop error shows the peak distribution differences and packing density illustrates the differences in air flow profile with the inhale and exhale area episodes. Taken from [52].
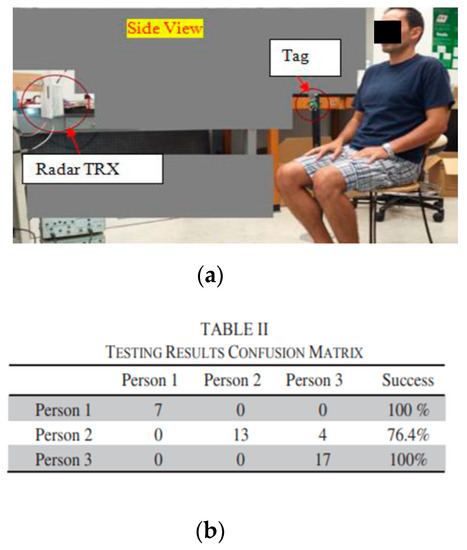
Figure 4. Human identification experiment using a radar system. The test set-up is shown, (a), along with the neural network recognition results, (b). From [52].
Subsequent research by the same group reported on continuous authentication based on dynamic segmentation where they used inhale and exhale area ratios of the captured respiratory pattern as unique features for six different participants [68]. Dynamic segmentation evaluates the displacement and identifying points in the range of 30–70% of both exhale and inhale episodes, which defines four boundary points of a trapezium [65]. The ratio of these two areas provides a useful feature which indicates how quickly the next cycle of inhalation begins [68]. Figure 5 illustrates the inhale/exhale area ratio features for two different subjects, which differ significantly. Based on extracted unique features, a K-nearest algorithm was integrated to identify each person, which showed a classification accuracy of almost 90% [68]. In order to increase the accuracy of the proposed method, minor component analysis was performed on subject data sets which showed overlapping inhale/exhale area ratios. For minor-component analysis, a linear demodulation technique was employed [68]. The variation in minor component shows the radar cross section and high frequency component of respiration and heart signal modulation. Higuchi fractal dimension analysis was performed on minor components of the radar captured signals to identify overlapped inhale/exhale area ratios of subjects, which increased the classification accuracy to 95% [68]. The proposed method clearly shows efficacy. However, the number of subjects of tested was small and further investigation is required to establish larger data set functionality.
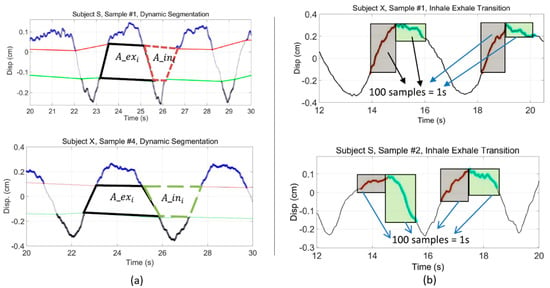
Figure 5. Respiratory pattern classifiers used for subject recognition. Dynamically segmented inhale/exhale area ratios of two subjects significantly differs, (a), as do signal patterns relating to the dynamics of breathing near the points where the inhale and exhale transition occurs, (b). From [68].
Another limitation of this approach is the reliance on two different parameters (inhale/exhale area ratio and minor component analysis). Further investigations also demonstrated that, as inhale/exhale ratio become more similar, false classification may occur [70]. To increase performance further, an FFT based feature extraction approach was applied with an integrated support-vector machines (SVM) classifier using a radial basis function [70]. The performance of the proposed system increased as the FFT based feature extraction approach contains all breathing dynamics related features (breathing rate, breathing depth, inhale rate, exhale rate and airflow profile). Figure 6 illustrates the FFT based feature extraction approach used for six different participants. As the data set and number of participants was small, continued experimentation remains needed to verify the efficacy of the FFT-based feature extraction approach. For further investigation, the feasibility of the FFT-based approach for extracting identifying features from radar respiratory traces for sedentary subjects was tested, along with measurements of the subjects just after performing physiological activities (walking upstairs) [69]. It was found that subject recognition still worked but was not as effective after performing short exertions as it was for sedentary subjects [71]. Experimental results demonstrated that, after short exertion, the dynamically segmented exhale area and breathing depth increased by more than 1.4 times for all participants, which made evident the uniqueness of the residual heart volume after expiration for recognizing each subject, even after short exertions [71]. They also integrated a machine learning classifier SVM, with a radial basis function kernel which resulted in an accuracy of 98.55% for subjects in a sedentary condition and almost 92% for a combined mixture of conditions (sedentary and after short exertions) [71]. Furthermore, they also investigated identity authentication of patients with obstructive sleep apnea (OSA) symptoms based on extracting respiratory features (peak power spectral density, packing density, and linear envelop error) for radar captured paradoxical breathing patterns, in a small-scale clinical sleep study integrating three different machine learning classifiers (SVM, k-nearest neighbor (KNN), and random forest). Their proposed OSA-based authentication method was tested and validated for five OSA patients with 93.75% accuracy, using a KNN classifier which outperformed other classifiers [72]. This study was limited to only six supine subjects in the controlled environment of a sleep center.
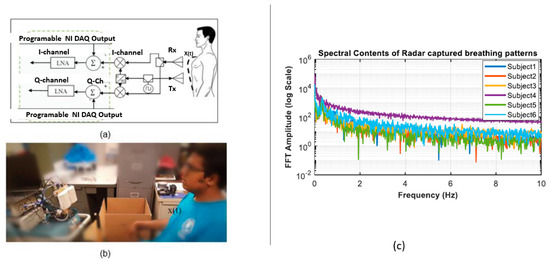
Figure 6. FFT/SVM based subject recognition study. A 2.4-GHz radar system (a) was used to measure subjects in seated position (b) and FFT-based extracted features up to 10 Hz were used to identify six different participants (c). From [70].
2.2. Radar-Based Identity Authentication through Heart-Based Features
One of the first attempts at recognizing people from their heart-based features (cardiac cycle) from Doppler radar was reported on by a research group at Clarkson University [73]. They used a 2.4-GHz heterodyne radar system from which cardiac data was extracted, and an ensemble average was computed using ECG as time reference [73]. A continuous wavelet transform was integrated to provide time-frequency analysis of the average radar-measured cardiac cycle and a k-nearest neighbor algorithm was used to recognize people with an accuracy of 82%. This was the first reported attempt for applying cardiac-based features using a cardiac-radar system as biometric identification tool [73]. The low classification accuracy occurred as there was overlap in the ensemble average of the cardiac cycle; therefore, further investigation and experimentation is required to demonstrate efficacy for more reliable recognition of subjects from radar captured signals.
A study conducted by a research group at the University of Buffalo [58] proposed a continuous identity authentication system named “Cardiac Scan”. This system used a 2.4-GHz Doppler radar transceiver with two antennas (one for transmit and another for receive functions) each having a beam width of 45°.
The radar power consumption was 650 mW with a 5V-volt source and 130 mA of current [58]. The customized Doppler radar was placed in front of the subject at 1 meter [58]. Figure 7 shows the experimental set up of the proposed cardiac scan system, from which five different points were extracted from the radar captured respiration patterns which were hypothesized to fully represent cardiac motion. Based on the hypothesis the experiment illustrated that these heart-based geometry measures differ from person to person due to difference in size, position and anatomy of the heart, chest configuration, and various other factors [58]. From their experimental results, it was also clear that no two subjects had the same heart, tissue, and blood circulation system, as there were significant differences in their cardiac cycle points measured in the radar data set [58]. Figure 8 illustrates the cardiac motion marker for one segment captured from the radar respiration measurement. In this work, the user’s cardiac-motion related features were stored in the system. A SVM with a radial basis function (RBF) kernel classifier was employed to uniquely identify different participants. A study of a 78 subject data set was reported, and the proposed system achieved an accuracy of 98.61% and a 4.42% equal error rate [58]. One of the limitations of the above proposed technique is that the complete study was performed with healthy sedentary persons and only for single-subject measurements. If subjects have cardiovascular diseases, unique identification may be problematic as the cardiac cycle would be affected. Further study is also required to verify that the proposed heart-based cardiac cycle points remain consistent after subjects perform varying degrees of physiological activity.
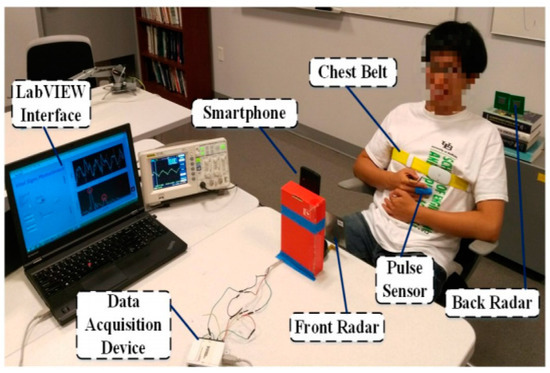
Figure 7. Experimental setup for cardiac scan continuous authentication system using microwave Doppler radar. A data acquisition device and LABVIEW interfaces were used to capture signals. A pulse sensor and chest belt were used for reference measurements. From [58].
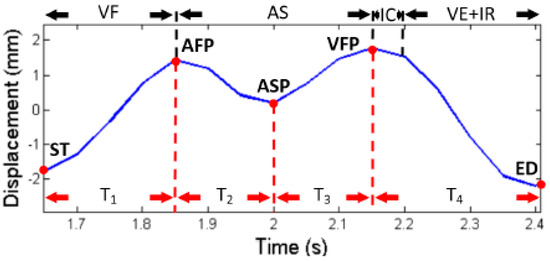
Figure 8. Cardiac motion marker. The cardiac motion cycle defined by five different points (red dots) within five different points of displacement and timing was calculated as a unique feature for recognizing people. From [58].
In another reported study, cardiac measurement of different persons was used to uniquely identify each using a 24-GHz continuous wave radar system employing six-port measurement technology [71]. Figure 9 represents the hardware setup used for this experiment. A six-port measurement system consists of two input ports and four output ports. The two input signals are superimposed to extract phase shift information due to chest displacement. This particular work focused on extracting heartbeat signal information for each participant, as the exact position and angle of the heart in the thorax, as well as the anatomy of the thorax itself, is a little different for every person due to varying tissue and muscle/fat components [74]. Due to these differences, the radar-captured heartbeat signal involved different propagation and attenuation characteristics. As each person has a different heart position and dimensions, dominant features exist in the heartbeat signal which form a complex and unique pattern. Figure 10 illustrates the heartbeat signal variation for each participant. Initially a 5-second heartbeat signal was used for identifying unique features for each participant. Integrated machine learning classifiers were also used to recognize people. A quadratic SVM outperformed other classifiers, with an accuracy of 74.2%. To increase the accuracy, a 7-second heartbeat segment was used, which increased the classification accuracy to 94.6%. The study provides a clear indication that heart-based geometry can be used as a unique feature to identify people. However, validation for this study only included four different participants. Thus, further investigation is required for larger data sets having varying conditions, especially those involving measurements made after physical activities.
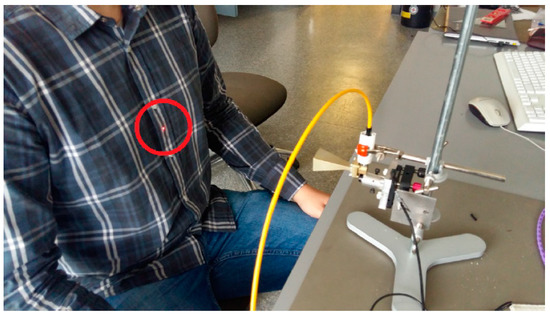
Figure 9. Experimental setup for unique identification of a human from radar captured respiration pattern which includes six-port technology. From [74].
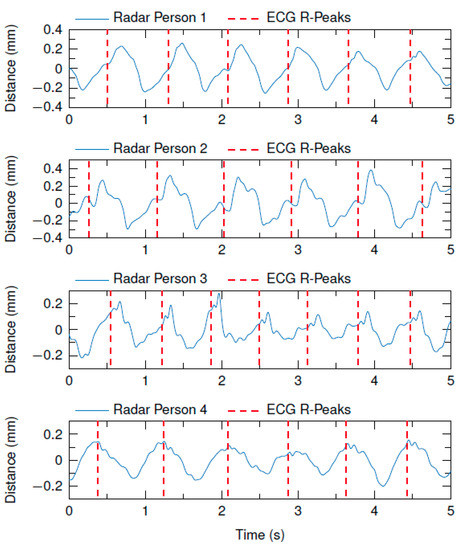
Figure 10. Heartbeat curves recorded by a 24-GHz radar for four subjects. Each signal is periodic but for each subject the pattern is a bit different which serves as a unique feature for recognition of identity. From [74].
Another study used a 24-GHz radar system to extract heartbeat related unique features to recognize eleven different participants [75]. An autoregressive (AR) model-based frequency analysis was introduced, which is superior to FFT, having a window length of 100 milliseconds, from which power spectral density could be calculated [75]. Each peak in this analysis represents the contraction and extraction of the heart. The first peak was used as a reference and then a period of 0.2 s before and after, 0.4 s, was used as a template. Template matching was used to detect all heartbeats. The average of the power spectral density was used as a unique identification number for each participant. Figure 11 illustrates the power spectral density features extracted from the radar respiration signal and PSD profile for eleven different participants. The success rate was 92.8%. The proposed method clearly demonstrates heart-based PSD feature extraction efficacy for recognizing people. However, if the position between the radar and human subject changes or the heart rate fluctuates greatly then the proposed method produces false classification. Motion artifacts and multi-subject scenarios were not considered and remain a significant challenge for this approach.
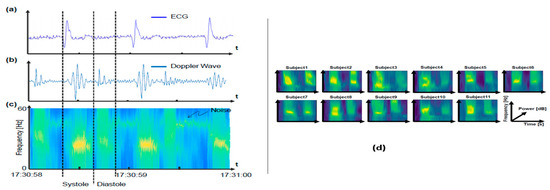
Figure 11. Measured 24-GHz heartbeat patterns for autoregressive PSD analysis based subject recognition. Measurement of heartbeats are shown for electrocardiogram (reference) (a), Doppler radar (b), PSD of Doppler sensor output (c), and (d) PSD for 15-s Doppler radar for eleven participants [75].
Recently, another study demonstrated the efficacy of radar-based identity authentication using a short-time Fourier Transform (STFT) [76]. Each person sat a 1.5 m distance and physiological signatures were recorded for about 6 seconds of the breathing pattern, using a 24-GHz continuous wave radar. An STFT was used to characterize the micro-Doppler signature of ten different participants, followed by basic image transformation methods like translation, rotation, zoom, mirror, and cropping. The STFT image was used to represent heart-based features for each different subject. A deep convolutional neural network (DCNN) was used to classify subjects based on their radar captured micro-Doppler signatures. Figure 12 illustrates the STFT images for four participants which are significantly different for each subject and include unique features for identification. From the spectrogram, three different heart-based features were extracted, such as the period of the heartbeat, the energy of the heartbeat, and the bandwidth of the signal. A deep convolutional neural network was then trained, and the resulting classification accuracy was almost 98.5%.
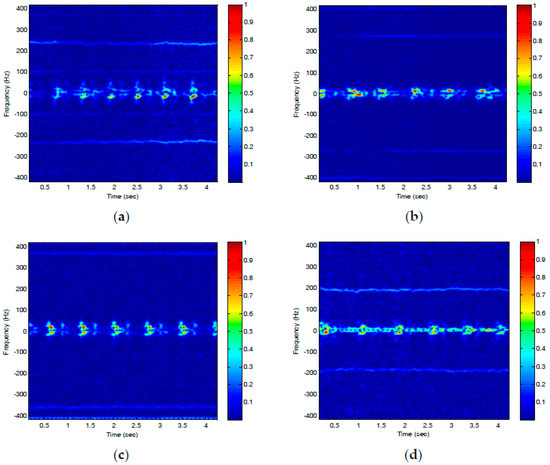
Figure 12. (a–d) Short time Fourier transform (STFT) of four different participants for extracting micro-Doppler signatures. The images for four different participants clearly have significantly different spectral content. From [76].
To extract heart-based or respiratory information, data segmentation generally plays an important role. Segments correspond to the FFT window size and should contain at least one full respiration cycle and multiple cardiac cycles [58][70]. The number of segments used for a data set also plays an important role for authentication time and accuracy [58]. Increasing the FFT window size will bring a benefit in resolution as a higher number of samples are included in the operation, but this will also increase the time delay and complexity of authentication and is not generally justified for real-time operation.
References
- Watson-Watt, R. Radar in war and in peace. Nature 1945, 156, 319–324.
- Lin, J.C. Microwave sensing of physiological movement and volume change: A review Bioelectromagnetics 1992, 13, 557–565, doi:10.1002/bem.2250130610.
- Chen, K.-M.; Misra, D.; Wang, H.; Chuang, H.-R.; Postow, E. An X-band microwave life-detection system. IEEE Trans. Biomed. Eng. 1986, BME-33, 697–701, doi:10.1109/TBME.1986.325760.
- Droitcour, A.; Lubecke, V.; Lin, J.; Boric-Lubecke, O. A microwave radio for Doppler radar sensing of vital signs. In Proceedings of the 2001 IEEE MTT-S International Microwave Symposium Digest (Cat. No.01CH37157), Phoenix, AZ, USA, 20–24 May 2001; Volume 1, pp. 175–178, doi:10.1109/MWSYM.2001.966866.
- Bugaev, A.S.; Vasil’ev, I.A.; Ivashov, S.V.; Chapurskii, V.V. Radar methods of detection of human breathing and heartbeat. J. Commun. Technol. Electron. 2006, 51, 1154–1168, doi:10.1134/S1064226906100056.
- Soldovieri, F.; Catapano, I.; Crocco, L.; Anishchenko, L.N.; Ivashov, S.I. A feasibility study for life signs monitoring via a continuous-wave radar. Int. J. Antennas Propag. 2012, 2012, 1–5, doi:10.1155/2012/420178.
- Chuang, H.-D.; Chen, Y.F.; Chen, K.-M. Automatic clutter-canceler for microwave life-detection systems. IEEE Trans. Instrum. Meas. 1991, 40, 747–750, doi:10.1109/19.85346.
- Lin, J. Noncontact measurement of cardiopulmonary movements: A review of system architectures and the path to micro-radars. In Proceedings of the 2013 IEEE MTT-S International Microwave Workshop Series on RF and Wireless Technologies for Biomedical and Healthcare Applications (IMWS-BIO), Singapore, 9–11 December 2013; pp. 1–3, doi:10.1109/IMWS-BIO.2013.6756241.
- Yan, Y.; Li, C.; Yu, X.; Weiss, M.D.; Lin, J. Verification of a non-contact vital sign monitoring system using an infant simulator. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 2-6 September 2009; pp. 4836–4839, doi:10.1109/IEMBS.2009.5332668.
- Baboli, M.; Singh, A.; Soll, B.; Boric-Lubecke, O.; Lubecke, V.M. Wireless sleep apnea detection using continuous wave quadrature Doppler radar. IEEE Sens. J. 2020, 20, 538–545, doi:10.1109/JSEN.2019.2941198.
- Boric-Lubecke, O.; Lubecke, V.M.; Droitcour, A.D.; Park, B.K.; Singh, A. Doppler Radar Physiological Sensing; Willey-IEEE Press, New Jersey, USA, 2016.
- Gao, J.; Ertin, E.; Kumar, S.; Alabsi, M. Contactless sensing of physiological signals using wideband RF probes. In Proceedings of the 2013 Asilomar Conference on Signals, System and Computers, Pacific Grove, CA, USA, 3–6 November 2013; pp. 1230–1233.
- Islam, S.M.M.; Boric-Lubecke, O.; Lubekce, V.M. Concurrent respiration monitoring of multiple subjects by phase-comparison monopulse radar using Independent Component Analysis (ICA) with JADE Algorithm and Direction of Arrival (DOA) IEEE Access 2020, 8, 73558–73569, doi:10.1109/ACCESS.2020.2988038.
- Mercuri, M.; Lorato, I.R.; Liu, Y.-H.; Wieringa, F.; Hoof, C.V.; Torfs, T. Vital-sign monitoring and spatial tracking of multiple people using a contactless radar-based sensor. Nat. Electron. 2019, 2, 252–262, doi:10.1038/s41928-019-02586.
- Su, W.-C.; Tang, M.-C.; Arif, R.E.; Horng, T.-S.; Wang, F.-K. Stepped-frequency continuous-wave radar with self-injection-locking technology for monitoring multiple human vital signs. IEEE Trans. Microw. Theory Tech. 2019, 67, 5396–5405, doi:10.1109/TMTT.2019.2933199.
- Lee, H.; Kim, B.-H.; Park, J.-K.; Yook, J.-G. A novel vital-sign sensing algorithm for multiple subjects based on 24-GHz FMCW doppler radar. Remote Sens. 2019, 11, 1237–1252, doi:10.3390/rs11101237.
- Yavari, E.; Song, C.; Lubecke, V.; Boric-Lubecke, O. Is there anybody in there? Intelligent radar occupancy sensors. IEEE Microw. 2014, 15, 57–64, doi:10.1109/MMM.2013.2296210.
- Lin, J.C. Noninvasive microwave measurement of respiration. Proc. IEEE 1975, 63, 1530–1530, doi:10.1109/PROC.1975.9992.
- Greneker, E.F. Radar sensing of heartbeat and respiration at a distance with applications of the technology. In Proceedings of the IEEE Radar Conference, Edinburg, UK, 14–16 October 1997; pp. 150–154, doi:10.1049/cp:19971650.
- Hafner, N.; Mostafanezhad, I.; Lubecke, V.M.; Boric-Lubecke, O.; Host-Madsen, A. Non-contact cardiopulmonary sensing with a baby monitor. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 2300–2302, doi:10.1109/IEMBS.2007.4352785.
- Gu, C.; Li, C.; Lin, J.; Long, J.; Huangfu, J.; Ran, L. Instrument-based non-contact Doppler radar vital sign detection system using heterodyne digital quadrature demodulation architecture. IEEE Trans. Instrum. Meas. 2009, 59, 1580–1588.
- Mostafanezhad, I.; Boric-Lubecke, O.; Lubecke, V.M.; Mandic, D.P. Application of empirical mode decomposition in removing fidgeting interference in Doppler radar life signs monitoring devices. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2–6 September 2009; pp. 340–343.
- Yunqiang, Y.; Fathy, A.E. Development and implementation of a real time see-through-wall radar system based on FPGA. IEEE Geosci. Remote Sens. Lett. 2013, 10, 328–331.
- Zhu, Z.; Zhang, X.; Lv, H.; Lu, G.; Jing, X.; Wang, J. Human-target detection and surrounding structure estimation under a simulated rubble via UWB radar. IEEE Geosci. Remote Sens. Lett. 2013, 10, 328–331.
- Li, C.; Lubecke, V.M.; Boric-Lubecke, O.; Lin, J. A review on recent advances in doppler radar sensor for non-contact healthcare monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2046–2060, doi:10.1109/TMTT.2013.2256924.
- Capp, P.K.; Pearl, P.L.; Lewin, D. Pediatric sleep disorders. Prim. Care 2005, 32, 549–562.
- Forster, H.; Ipsiroglu, O.; Kerbl, R.; Paditz, E. Sudden infant death and pediatric sleep disorders. Wien. Klin. Wochenschr. 2003, 115, 847–849.
- Singh, A.; Lee, S.; Buttler, M.; Lubekce, V.M. Activity monitoring and motion classification of the lizard chamaeleon jacksonii using multiple doppler radars. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 4525–4528, doi:10.1109/EMBC.2012.6346973.
- Singh, A.; Hafner, N.; Buttler, M.; Lubekce, V.M. A data efficient method for characterization of chameleon tongue motion using Doppler radar. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 574–577, doi:10.1109/EMBC.2012.6345996.
- Drazen, N.H.; Lubekce, V.M. Fish heart rate monitoring by body-contact Doppler radar. IEEE Sens. J. 2013, 13, 408–414, doi:10.1109/JSEN.2012.2210400.
- Singh, A.; Baboli, M.; Gao, X.; Yavari, E.; Padasdao, B.; Soll, B.; Boric-Lubecke, O.; Lubecke, V. Considerations for integration of a physiological radar monitoring system with gold standard clinical sleep monitoring systems. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 2120–2123, doi:10.1109/EMBC.2013.6609952.
- Kai Sensors Receives FDA Clearance For Its Wireless, Non-Contact Respiratory Device. Available online: https://www.meddeviceonline.com/doc/kai-sensors-receives-fda-clearance-for-its-0001 (accessed on June 17, 2009).
- Gennarelli, G.; Crocco, L.; Solodovieri, F. Doppler radar for real-time surveillance. In Proceedings of the 2018 18th Mediterranean Microwave Symposium (MMS), Istanbul, Turkey, 31 October–2 November 2018; pp. 387–390, doi:10.1109/MMS.2018.8612032.
- Lee, Y.S.; Pathirana, P.N.; Evans, R.J.; Steinfort, C.L. Monitoring and analysis of respiratory patterns using microwave doppler radar. IEEE J. Transl. Eng. Health Med. 2014, 2, 1–12, doi:10.1109/JTEHM.2014.4365776.
- Chaos Computer Club (CCC), Chaos Computer Club Breaks Apple touch ID. September 2013. Available online: https://www.ccd.de/en/updates/2013/ccc-breaks-apple-touchid (accessed on 22 September, 2013).
- Chaos Computer Club (CCC), Fingerprints Biometric Hacked Again. December 2014. Available online: https://www.ccd.de/en/updates/2014/ursel (accessed on 10 November 2016).
- Zhang, Q.; Yin, Y.; Yang, G. Unmatched minutiae: Useful information to boost fingerprint recognition. Neurocomputing 2016, 171,1401–1413.
- Marceo, A.; Crater, M; Strommback B. Palm prints. In Encyclopedia of Forensic Sciences; Academic Press: Waltham, MA, USA, 2013; pp. 29–36.
- Nguyen, K.; Fookes, C.; Jillela, R.; Sridharan, S.; Ross, A. Long range iris recognition: A survey. Pattern Recognit. 2017, 72, 123–143, doi:10.1016/j.patcog.2017.05.021.
- Thomas, K.P.; Vinod, A.P. Towards EEG based biometric systems: The great potential of Brain-wave based biometrics. IEEE Trans. Syst. Man Cybern. Syst 2017, 3, 6–15.
- Lu, Y.; Wu, S.; Fang, Z.; Xiong, N.; Yoon, S.; Park, D.S. Exploring finger vein based personal authentication for secure IOT. Future Gener. Comput. Syst. 2017, 77, 149–160.
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Towards pervasive gait analysis with wearable sensors: A systematic review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537.
- Ricanek, K.; Savvides, M.; Woodard, D.L.; Dozier, G. Unconstrained biometric identification: Emerging technologies. J. Comput. 2010, 43, 56–62.
- Liu, T.; Liang, Z.Q. Lightweight biometric sensing for walker classification using narrowband RF. Sensors 2010, 17, 56–62.
- Derbel, A.; Vivet, D.; Emile, B. Access control based on gait analysis and face recognition. Electron. Lett. 2015, 51, 751–752.
- Balazia, M.; Plataniotis, K.N. Human gait recognition from motion capture data in signature process. IET Biomed. 2017, 6, 129–137.
- Springer, S.; Seligmann, G.Y. Validity of the kinetic for Gait Assessment: A focused review. Sensors 2016, doi:10.3390/s16020194.
- Tang, J.; Luo, J.; Tjahjadi, T.; Gao, Y. 2.5D multi-view gait recognition based on point cloud registration. Sensors 2014, 14, 6124–6143.
- Van Dorp, P.; Groen, F.C. Feature-based human motion parameter estimation with radar. IET Radar Sonar Navig. 2008, 2, 135–145.
- Chen, V.C. Doppler signatures of radar backscattering from objects with micro-motions. IET Signal Process. 2008, 2, 291–300.
- Geisheimer, J.L.; Marshall, W.S.; Greneker, E.A. Continuous-wave (CW) radar for gait analysis. In Proceedings of the 35th IEEE Aslimar Conference on Signal, Systems and Computers, Pacific Grove, CA, USA, 4–7 November 2001; Volume 1, pp. 834–838.
- Rahman, A.; Yavari, E.; Lubecke, V.M.; Lubekce, O.-B. Noncontact Doppler radar unique identification system using neural network classifier on life signs. In Proceedings of the 2016 IEEE Topical Conference on Biomedical Wireless Technologies, Networks, and Sensing Systems (BioWireless), Austin, Tx, USA, 24 January 2016; pp. 46–48, doi:10.1109/BIOWIRELESS.2016.7445558.
- Pavlo, O.M.; Jaakko, T.A.; K.; Karen, O.E.; Alexander, V.T. Target Classification by using pattern features extracted from bispectrum-based radar doppler signatures. In Proceedings of the 2011 12th International Radar Symposium (IRS), Leipzig, Germany, 7–9 September 2011; pp. 791–796.
- A. D. Droitcour, G.T.A. Kovacs, O. Boric- Lubecke and K. Shenoy. Engineering, Measurement of Heart and Respiration Rates with a Single-Chip. Ph.D. Thesis, Stanford University, Stanford, CA, USA, 2006.
- Benchetrit, G. Breathing pattern in humans: Diversity and individuality. Respir. Physiol. 2000, 122, 123–129.
- Vander, A.; Sherman, J.; Luciano, D. Human Physiology: The Mechanism of Body Function, 7th ed.; McGraw Hill: San Francisco, CA, USA, 1998.
- Opie, L.H. Mechanisms of cardiac contraction and relaxation. In Heart Disease: A Textbook of Cardiovascular Medicine; Braunwald, E., Zipes, D.P., Libby, P., Eds.; W.B. Saunders Company: New York, NY, USA, 2001; pp. 443–478.
- Lin, F.; Song, C.; Zhuang, Y.; Xu, W.; Li, C.; Ren, K. Cardiac scan: A non-contact and continuous heart-based user authentication system. In Proceedings of the 23rd Annual Conference on Mobile Computing and Communication (MobiCom), Snowbird, UT, USA, 16–20 October 2017; pp. 315–328, doi:10.1145/3117811.3117839.
- Aubert, A.E.; Welkenhuysen, L.; Montald, J.; de Wolf, L.; Geivers, H.; Minten, J.; Kesteloot, H.; Geest, H. Laser method for recording displacement of the heart and chest wall. J. Biomed. Eng. 1984, 6, 134–140.
- Reinvuo, T.; Hannula, M.; Sorvoja, H. Measurement of respiratory rate with high resolution accelerometer and EMFit pressure sensor. In Proceedings of the 2006 IEEE Sensors Applications Symposium, Houston, TX, USA, 7–9 February 2006; pp. 192–195, doi: 10.1109/SAS.2006.1634270.
- Hung, P.; Bonnet, S.; Guillemaud, R.; Castelli, E.; Yen, P. Estimation of respiratory waveform using an accelerometer. In Proceedings of the 2008 5th IEEE International Symposium on Biomedical Imaging: From Nano to Macro, Paris, France, 14–17 May 2008; pp. 1493–1496, doi: 10.1109/ISBI.2008.4541291.
- Hall, J.E. Gayton and Hall Textbook of Medical Physiology; Elsevier Health Sciences: Amsterdam, The Netherlands, 2010.
- Barrett, K.E.; Barman, S.M.; Boitano, S. Ganong’s Review of Medical Physiology; McGraw Hill: New Delhi, India, 2010.
- Li, M.; Li, X. Verification based ECG biometrics with cardiac irregular conditions using heartbeat level and segment level information fusion. In Proceedings of the IEEE 20th International Conference on Acoustic Speech and Signal Processing (ICASSP), Florence, Italy, 4–9 May, pp. 3769–3773, doi: 10.1109/ICASSP.2014.6854306.
- Shepherd, S. Continuous authentication by analysis of keyboard typing characteristics in security and detection. in European convention on security and detection , Brighton, UK, 1995, doi:10.1049/cp:19950480.
- Weldon, M.K. The Future X Network: A Bell Lab Perspective; CRC Press: Boca Raton, FL, USA, 2015.
- Mostafanezhad, I.; Boric-Lubecke, O.; Lubecke, V. A coherent low IF receiver architecture for Doppler radar motion detectors used in life signs monitoring. In Proceedings of the 2010 IEEE Radio and Wireless Symposium (RWS), New Orleans, LA, USA, 10–14 January 2010, pp. 571-574, doi: 10.1109/RWS.2010.5434190.
- Rahman, A.; Lubecke, V.M.; Boric-Lubecke, O.; Prins, J.H.; Sakamoto, T. Doppler radar techniques for accurate respiration characterization and subject identification. IEEE J. Emerg. Sel. Top. Circuits Syst. 2018, 8, 350–359, doi:10.1109/JETCAS.2018.2818181.
- Facts+Statistics: Identity Theft and Cybercrime. Available online: https://www.iii.org/fact-statistic/facts-statistics-identity-theft-and-cybercrime (accessed on 7 January, 2019 ).
- Islam, S.M.M.; Rahman, A.; Prasad, N.; Boric-Lubecke, O.; Lubecke, V.M. Identity authentication system using support vector machine on radar respiration measurement. In Proceedings of the 93rd ARFTG Microwave Measurement Conference (ARFTG’19), Boston, MA, USA, 2–7 June 2019; pp. 1–5, doi:10.1109/ARFTG.2019.8739240.
- Islam, S.M.M.; Sylvester, A.; Orpilla, G.; Lubecke, V.M. Respiratory feature extraction for radar-based continuous identity authentication. In Proceedings of the 2020 IEEE Radio and Wireless Symposium (RWS), San Antonio, TX, USA, 26–29 January 2020; pp. 119–122, doi:10.1109/RWS45077.2020.9050013.
- Islam, S.M.M.; Rahman, A.; Yavari, E.; Boric-Lubecke, O.; Lubecke, V.M. Identity authentication of OSA patients using microwave doppler radar and machine learning classifiers. In Proceedings of the 2020 IEEE Radio and Wireless Symposium (RWS), San Antonio, TX, USA, 26–29 January 2020; pp. 251–254, doi:10.1109/RWS45077.2020.9049983.
- Rissacher, D.; Galy, D. Cardiac radar for biometric identification using nearest neighbor for continuous wavelet transform peaks. In Proceedings of the IEEE International Conference on Identity, Security and Behavior Analysis (ISBA 2015), Hong Kong, China, 23–25 March 2015; pp. 1–6, doi:10.1109/ISBA.2015.7126536.
- Shi, K.; Will, C.; Weigel, R.; Koelpin, A. Contactless person identification using cardiac radar signals. In Proceedings of the 2018 IEEE International Instrumentation and Measurement Technology Conference (I2MTC), Houston, TX, USA, 14–17 May 2018; pp. 1–6, doi:10.1109/I2MTC.2018.8409645.
- Okano, T.; Izumi, S.; Kawaguchi, H.; Yoshimoto, M. Non-contact biometric identification and authentication using microwave Doppler sensor. In Proceedings of the 2017 IEEE Biomedical Circuits and Systems Conference (BioCAS), Torino, Italy, 19–21 October 2017; pp. 1–4, doi:10.1109/BIOCAS.2017.8325160.
- Cao, P.; Xia, W.; Li, Y. Heart id: Human identification based on radar micro-doppler signatures of the heart using deep Learning. Remote Sens. 2019, 11, 1220–1236, doi:10.3390/rs11101220.
- Zhang, J.; Wei, B.; Hu, W.; Kanhere, S.S. WiFi-ID: Human identification using WiFi signal. In Proceedings of the 2016 International Conference on Distributed Computing in Sensor Systems (DCOSS), Washington, DC, USA, 26–28 May 2016, pp. 75–82, doi:10.1109/DCOSS.2016.30.
- Liu, J.; Chen, Y.; Dong, Y.; Wang, Y.; Zhao, T.; Yao, Y.D. Continuous user verification via respiratory biometrics. In Proceedings of the IEEE Conference on Computer Communications (INFOCOM’20), Toronto, ON, Canada, 6–9 July 2020.




