
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Alexandra Tsirogianni | + 1616 word(s) | 1616 | 2021-08-19 11:22:34 | | | |
| 2 | Beatrix Zheng | + 166 word(s) | 1782 | 2021-08-27 12:17:44 | | |
Video Upload Options
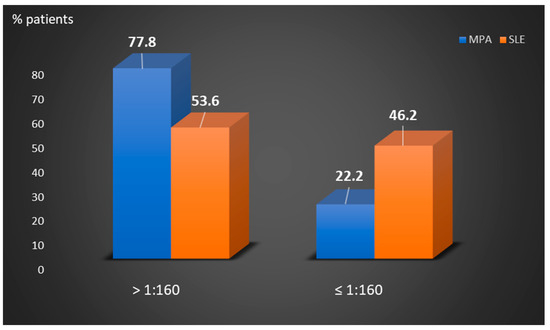
Perinuclear anti-neutrophilic cytoplasmic antibodies (P-ANCA) recognize heterogeneous antigens, including myeloperoxidase (MPO), lactoferrin, elastase, cathepsin-G and bactericidal/permeability-increasing protein. Although P-ANCA have diagnostic utility in vasculitides, they may also be found in patients with various other systemic autoimmune rheumatic diseases (SARDs). Nevertheless, the clinical significance and the targets recognized by P-ANCA in such patients remain unclear. For this purpose, herein we investigated the occurrence of ANCA-related antigenic specificities in 82 P-ANCA-positive sera by multiplex ELISA, as well as their association with other autoantibodies. The P-ANCA-positive sera corresponded to patients with vasculitides (n = 24), systemic lupus erythematosus (n = 28), antiphospholipid syndrome (n = 5), Sjögren’s syndrome (n = 7), rheumatoid arthritis (n = 3), systemic scleroderma (n = 1), sarcoidosis (n = 1) and Hashimoto′s thyroiditis (n = 13). In most P-ANCA-positive patients studied (51/82, 62.3%), these autoantibodies occurred in high titers (>1:160). The analysis of P-ANCA-positive sera revealed reactivity to MPO in only 50% of patients with vasculitides, whereas it was infrequent in the other disease groups studied. Reactivity to other P-ANCA-related autoantigens was also rarely detected. Our findings support that high P-ANCA titers occur in SARD. The P-ANCA-positive staining pattern is associated with MPO specificity in vasculitides, while in other autoimmune diseases, it mostly involves unknown autoantigens.
1. Introduction
2. Analysis on Results
2.1. Patients’ Characteristics
2.2. P-ANCA Titers and Serum Autoantigen Specificity Per Autoimmune Disease
| Patient Groups | P-ANCA Serum Titers (No Positive) | ||||||
|---|---|---|---|---|---|---|---|
| ≥1:640 | 1:320 | 1:160 | 1:80 | 1:40 | 1:20 | ||
| Vasculitides | MPA (n = 18) | 9 | 5 | 1 | 1 | 1 | 1 |
| BD (n = 2) | 1 | 1 | 0 | 0 | 0 | 0 | |
| Aortitis (n = 1) | 1 | 0 | 0 | 0 | 0 | 0 | |
| HSP (n = 2) | 0 | 0 | 1 | 1 | 0 | 0 | |
| CV (n = 1) | 0 | 1 | 0 | 0 | 0 | 0 | |
| SLE (n = 28) | 9 | 6 | 3 | 7 | 23 | 0 | |
| APS (n = 5) | 1 | 1 | 1 | 1 | 0 | 1 | |
| SS (n = 7) | 5 | 0 | 0 | 0 | 0 | 2 | |
| RA (n = 3) | 2 | 0 | 0 | 1 | 0 | 0 | |
| SSCL (n = 1) | 0 | 1 | 0 | 0 | 0 | 0 | |
| Sarcoidosis | (n = 1) | 0 | 0 | 1 | 0 | 0 | 0 |
| Hashimoto | (n = 13) | 2 | 1 | 4 | 2 | 1 | 3 |
| Autoimmune Diseases | Antigens Recognized by P-ANCA Positive Sera (No Positive) | ||||||
|---|---|---|---|---|---|---|---|
| MPO | Elastase | Cathepsin G | BPI | Lactoferrin | MPO/Lactoferrin | ||
| Vasculitides | MPA (n = 18) | 11 | 0 | 0 | 0 | 0 | 0 |
| BD (n = 2) | 1 | 0 | 0 | 0 | 0 | 0 | |
| Aortitis (n = 1) | 0 | 0 | 0 | 0 | 0 | 0 | |
| HSP (n = 2) | 0 | 0 | 0 | 0 | 0 | 0 | |
| CV (n = 1) | 0 | 0 | 0 | 0 | 1/1 (100) | 0 | |
| SLE (n = 28) | 1 | 0 | 0 | 0 | 1/28 (3.6) | 1/28 (3.6) | |
| APS (n = 5) | 1 | 0 | 0 | 0 | 0 | 0 | |
| SS (n = 7) | 0 | 1 | 0 | 0 | 0 | 0 | |
| RA (n = 3) | 1 | 0 | 0 | 0 | 0 | 0 | |
| SSCL (n = 2) | 1 | 0 | 0 | 0 | 0 | 0 | |
| Sarcoidosis (n = 1) | 0 | 0 | 0 | 0 | 0 | 0 | |
| Hashimoto (n = 13) | 0 | 0 | 0 | 0 | 0 | 0 | |
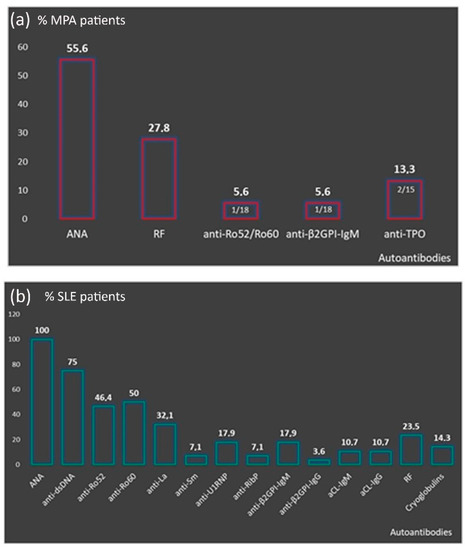
2.3. Autoantibody Profile of P-ANCA Positive Patients and P-ANCA Related Specificity
2.4. Disease Features of P-ANCA Positive Patients
3. Current Insights
References
- Savige, J.; Pollock, W.; Trevisin, M. What do antineutrophil cytoplasmic antibodies (ANCA) tell us? Best Pract. Res. Clin. Rheumatol. 2005, 19, 263–276.
- Kitching, A.R.; Anders, H.J.; Basu, N.; Brouwer, E.; Gordon, J.; Jayne, D.R.; Kullman, J.; Lyons, P.A.; Merkel, P.A.; Savage, C.O.S.; et al. ANCA-associated vasculitis. Nat. Rev. Dis. Primers 2020, 6, 71.
- Lionaki, S.; Blyth, E.R.; Hogan, S.L.; Hu, Y.; Senior, B.A.; Jennette, C.E.; Nachman, P.H.; Jennette, J.C.; Falk, R.J. Classification of antineutrophil cytoplasmic autoantibody vasculitides: The role of antineutrophil cytoplasmic autoantibody specificity for myeloperoxidase or proteinase 3 in disease recognition and prognosis. Arthritis Rheum. 2012, 64, 3452–3462.
- Falk, R.J.; Jennette, J.C. Anti-neutrophil cytoplasmic autoantibodies with specificity for myeloperoxidase in patients with systemic vasculitis and idiopathic necrotizing and crescentic glomerulonephritis. N. Engl. J. Med. 1988, 318, 1651–1657.
- Comarmond, C.; Crestani, B.; Tazi, A.; Hervier, B.; Adam-Marchand, S.; Nunes, H.; Cohen-Aubart, F.; Wislez, M.; Cadranel, J.; Housset, B.; et al. Pulmonary fibrosis in antineutrophil cytoplasmic antibodies (ANCA)-associated vasculitis: A series of 49 patients and review of the literature. Medicine 2014, 93, 340–349.
- Sada, K.E.; Yamamura, M.; Harigai, M.; Fujii, T.; Dobashi, H.; Takasaki, Y.; Ito, S.; Yamada, H.; Wada, T.; Hirahashi, J.; et al. Classification and characteristics of Japanese patients with antineutrophil cytoplasmic antibody-associated vasculitis in a nationwide, prospective, inception cohort study. Arthritis Res. Ther. 2014, 16, R101.
- Stone, J.H.; Merkel, P.A.; Spiera, R.; Seo, P.; Langford, C.A.; Hoffman, G.S.; Kallenberg, C.G.; St Clair, E.W.; Turkiewicz, A.; Tchao, N.K.; et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N. Engl. J. Med. 2010, 363, 221–232.
- Unizony, S.; Villarreal, M.; Miloslavsky, E.M.; Lu, N.; Merkel, P.A.; Spiera, R.; Seo, P.; Langford, C.A.; Hoffman, G.S.; Kallenberg, C.M.; et al. Clinical outcomes of treatment of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis based on ANCA type. Ann. Rheum. Dis. 2016, 75, 1166–1169.
- Terrier, B.; Saadoun, D.; Sene, D.; Ghillani, P.; Amoura, Z.; Deray, G.; Fautrel, B.; Piette, J.C.; Cacoub, P. Antimyeloperoxidase antibodies are a useful marker of disease activity in antineutrophil cytoplasmic antibody-associated vasculitides. Ann. Rheum. Dis. 2009, 68, 1564–1571.
- Moiseev, S.; Cohen Tervaert, J.W.; Arimura, Y.; Bogdanos, D.P.; Csernok, E.; Damoiseaux, J.; Ferrante, M.; Flores-Suarez, L.F.; Fritzler, M.J.; Invernizzi, P.; et al. 2020 international consensus on ANCA testing beyond systemic vasculitis. Autoimmun. Rev. 2020, 19, 102618.
- Galeazzi, M.; Morozzi, G.; Sebastiani, G.D.; Bellisai, F.; Marcolongo, R.; Cervera, R.; De Ramon Garrido, E.; Fernandez-Nebro, A.; Houssiau, F.; Jedryka-Goral, A.; et al. Anti-neutrophil cytoplasmic antibodies in 566 European patients with systemic lupus erythematosus: Prevalence, clinical associations and correlation with other autoantibodies. European Concerted Action on the Immunogenetics of SLE. Clin. Exp. Rheumatol. 1998, 16, 541–546.
- Cambridge, G.; Williams, M.; Leaker, B.; Corbett, M.; Smith, C.R. Anti-myeloperoxidase antibodies in patients with rheumatoid arthritis: Prevalence, clinical correlates, and IgG subclass. Ann. Rheum. Dis. 1994, 53, 24–29.
- Font, J.; Ramos-Casals, M.; Cervera, R.; Bosch, X.; Mirapeix, E.; Garcia-Carrasco, M.; Morla, R.M.; Ingelmo, M. Antineutrophil cytoplasmic antibodies in primary Sjogren’s syndrome: Prevalence and clinical significance. Br. J. Rheumatol. 1998, 37, 1287–1291.
- Moxey, J.; Huq, M.; Proudman, S.; Sahhar, J.; Ngian, G.S.; Walker, J.; Strickland, G.; Wilson, M.; Ross, L.; Major, G.; et al. Significance of anti-neutrophil cytoplasmic antibodies in systemic sclerosis. Arthritis Res. 2019, 21, 57.
- Aringer, M.; Costenbader, K.; Daikh, D.; Brinks, R.; Mosca, M.; Ramsey-Goldman, R.; Smolen, J.S.; Wofsy, D.; Boumpas, D.T.; Kamen, D.L.; et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 1151–1159.
- Kida, I.; Kobayashi, S.; Takeuchi, K.; Tsuda, H.; Hashimoto, H.; Takasaki, Y. Antineutrophil cytoplasmic antibodies against myeloperoxidase, proteinase 3, elastase, cathepsin G and lactoferrin in Japanese patients with rheumatoid arthritis. Mod. Rheumatol. 2011, 21, 43–50.
- Talor, M.V.; Stone, J.H.; Stebbing, J.; Barin, J.; Rose, N.R.; Burek, C.L. Antibodies to selected minor target antigens in patients with anti-neutrophil cytoplasmic antibodies (ANCA). Clin. Exp. Immunol. 2007, 150, 42–48.





