
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Omar Hahad | + 2690 word(s) | 2690 | 2020-06-22 05:46:00 | | | |
| 2 | Omar Hahad | -3 word(s) | 2687 | 2020-06-23 14:49:37 | | | | |
| 3 | Rita Xu | -982 word(s) | 1705 | 2020-06-30 07:35:03 | | | | |
| 4 | Rita Xu | -15 word(s) | 1690 | 2020-10-26 10:33:09 | | |
Video Upload Options
Air pollution is a heterogeneous mixture of various constituents resulting from the complex interaction of multiple emissions and chemical reactions. This mixture comprises solid particles and liquid droplets suspended in the air, i.e., PM2.5, that can include organic carbon (OC), elemental or black carbon (EC), nitrates, sulfates, and metals (e.g., iron, vanadium, nickel, copper, and manganese) as well as gases (e.g., ground level ozone (O3), carbon monoxide (CO), sulfur dioxide (SO2), oxides of nitrogen (NOx)) gaseous organic compounds (e.g., non-methane volatile organic compounds (VOCs), polycyclic aromatic hydrocarbons (PAHs) and polychlorinated biphenyls (PCBs)), bacterial endotoxins (mostly bound to solid particles or liquid aerosols). There are two possible ways by which air pollutants enter the CNS, either through direct transport of particles into the CNS or via systemic inflammation upon initial recruitment of immune cells in the lung tissue. Once in the organism, the adverse effects of fine particulates on the brain rely mainly on three mechanisms. First, they can induce the release of proinflammatory mediators leading to chronic respiratory and systemic inflammation, thereby affecting the BBB and ultimately triggering neural-immune interaction and resulting in increased production of ROS and chronic oxidative stress. Second, the particles can damage the BBB through the direct formation of ROS and thereby alter the permeability of the barrier. Third, there can be mechanical stimulation of specific mechano-receptors in pulmonary tissue leading to the lung arc reflex and sympathetic activation with the release of vasoconstrictors such as catecholamines.
1. Air Pollution Mixtures and Sources
Air pollution is a heterogeneous mixture of various constituents resulting from the complex interaction of multiple emissions and chemical reactions. This mixture comprises solid particles and liquid droplets suspended in the air, i.e., PM2.5, that can include organic carbon (OC), elemental or black carbon (EC), nitrates, sulfates, and metals (e.g., iron, vanadium, nickel, copper, and manganese) as well as gases (e.g., ground level ozone (O3), carbon monoxide (CO), sulfur dioxide (SO2), oxides of nitrogen (NOx)) gaseous organic compounds (e.g., non-methane volatile organic compounds (VOCs), polycyclic aromatic hydrocarbons (PAHs) and polychlorinated biphenyls (PCBs)), bacterial endotoxins (mostly bound to solid particles or liquid aerosols) [1]. In the urban environment, over 90% of the pollutant mass is from gases or vapor-phase compounds, while anthropogenic combustion-derived particles are of special concern from a public health perspective due to their potential systemic toxicity owing to features such as high particle counts, high surface area to mass ratio, inflammatory and oxidative stress potential, and insoluble components, leading to facile distal airway and systemic penetration [1]. Types of atmospheric particles include coarse particles with an aerodynamic diameter between 2.5 and 10 µm (PM10), fine particles with a diameter less than 2.5 µm (PM2.5), and ultrafine particles with a diameter less than 0.1 µm (PM0.1), interconnected with the general notion that smaller particles may be more potent in inducing adverse health effects than larger particles [2]. There are four main types of sources of air pollution with fossil fuels and biomass combustion, and industry, agriculture, and wind-blown dust are also predominant sources of fine particulates in the air (Figure 1). Furthermore, it is important to note that, besides emission intensities related to e.g., the amount of fuel combusted, the number of animals in animal husbandry, industrial production levels, and distances traveled or similar activity data, air pollution is strongly influenced by climate and weather conditions [3]. For instance, factors such as wind direction and speed, atmospheric stability, and solar radiation are important determinants of the spatial (fine particles can travel more than 100 km from their place of generation) and temporal variation in air pollutants with some of the most aggressive of them being generated during hot periods with a high UV index [3]. Interestingly, air pollution and climate change influence each other via complex interactions in the atmosphere, both of which, in turn, affect public health [4]. Herein, increasing levels of pollutants such as sulfate and O3 can modify the energy balance of the atmosphere and earth’s surface, leading to climate change that alters the physical and chemical state of the atmosphere [5].
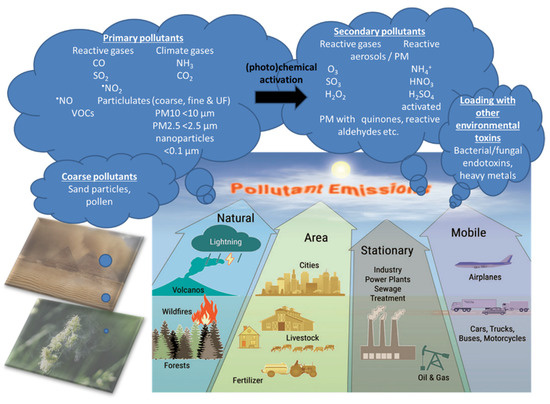
Figure 1. There are four main types of air pollution sources including natural, area, stationary, and mobile sources producing PM0.1, PM2.5, PM10, reactive gases including volatile organic compounds (VOCs). Primary pollutants (the indicated gases and solid particles) may undergo further toxification in the environment, e.g., by photochemical reactions by UV light producing more reactive gases or more toxic carbohydrate products on the particle surface (termed particle “aging”) [3] as well as loading of the particles with heavy/transition metals and bacterial/fungal endotoxins, leading to secondary biological toxicity [6][7][8]. The majority of coarse particles come from sediments (desert sand) and pollen from plants. Modified from Münzel et al. [9] with permission. Copyright 2020, Mary Ann Liebert, Inc., publishers. Open access source for sandstorm and plant pollen images can be found at Pixabay (http://pixabay.com/de/).
2. Pathophysiology of Air-Pollution-Induced Disorders
Since cardiovascular risk factors and diseases are triggered to a large amount by air pollution and impact a high proportion of global deaths, e.g., by inducing noncommunicable diseases, great efforts were made to explore, understand, and prevent the adverse cardiovascular effects of sustained exposure to air pollutants. On the basis of the Global Exposure-Mortality Model (GEMM), we have even shown that air pollution is a larger contributor to global mortality (8.79 million excess deaths) than one of the most important health risk factors, namely tobacco smoking (7.2 million excess deaths attributed to tobacco smoking as estimated by the WHO [10]), with a population average loss of life expectancy of 2.9 vs. 2.2 years for air pollution vs. tobacco smoking [11]. We recently reviewed the effects of gaseous and solid constituents of air pollution with a particular focus on the effect of fine particles on vascular endothelial function and clinical cardiovascular outcomes, indicating that vascular inflammation and oxidative stress are common denominators of the cardiovascular effects of air pollution [2]. Vascular endothelial dysfunction is regarded as an early subclinical key event in the development of dysregulated blood pressure and manifestation of atherosclerotic cardiovascular disease, which is not only due to classical risk factors (smoking, high cholesterol, diabetes mellitus, and hypertension) but also appears to be a consequence of environmental hazards such as air pollution [9][12]. Increasing evidence from human and animal studies suggests that exposure to ambient air pollutants leads to a pathological state of the vascular endothelium that is characterized by an imbalance between the formation and degradation of nitric oxide (•NO) [2]. Since the half-life and biological activity of •NO as a free radical is strongly related to the existence of ROS such as the superoxide ion, reduction and decreased activity of •NO as well as the direct physical damage to endothelial cells due to redox imbalance impairs several crucial functions of an intact endothelium to maintain its vasodilatory, antithrombotic, anti-inflammatory, and antioxidant effects. Thus, the persistent physiological detriments from the long-term exposure to air pollution can lead to atherosclerotic plaque formation and, over time, subsequently to various cerebro/cardiovascular disease phenotypes such as stroke, arterial hypertension, coronary heart disease, myocardial infarction, heart failure, and arrhythmia [13].
Likewise, emerging evidence from human and animal studies suggests an increased risk of cerebrovascular and neuropsychiatric disorders with sustained exposure to air pollutants affecting the CNS by a variety of cellular, molecular, inflammatory, and oxidative stress pathways. However, the understanding of the underlying mechanisms remains still incomplete and complex interactions with other risk and lifestyle factors are very likely. Deeper insight into these associations is of great importance and should receive more attention, since neurological, cerebrovascular and mental disorders are among the largest causes of disability-adjusted life years and global deaths with 30% of all strokes being related to air pollution [14]. There are two possible ways by which air pollutants enter the CNS, either through direct transport of particles into the CNS or via systemic inflammation upon initial recruitment of immune cells in the lung tissue [15]. Herein, nasal inhalation and airflow constitute a direct access route in humans with the olfactory region being unique in the CNS due to its direct contact with the environmental air. Smaller particles may cross the nose-brain barrier and reach the brain via olfactory receptor neurons or the trigeminal nerve, which then can travel across the CNS and reach other brain regions. On the other hand, particles can enter the circulation via the lungs through breathing and reach the alveolar region. At this point, they can translocate to the systemic circulation through a transition process (nanoparticles probably directly, microparticles most likely via uptake by phagocytic cells and their transmigration from the lung tissue to the circulation) [16] and subsequently across the BBB to the brain parenchyma by simple diffusion or energy-dependent active transport. Once in the organism, the adverse effects of fine particulates on the brain rely mainly on three mechanisms [17]. First, they can induce the release of proinflammatory mediators leading to chronic respiratory and systemic inflammation [18], thereby affecting the BBB and ultimately triggering neural-immune interaction and resulting in increased production of ROS and chronic oxidative stress contributing to an Alzheimer phenotype in exposed children [19]. Second, the particles can damage the BBB through the direct formation of ROS and thereby alter the permeability of the barrier [20][21]. Third, there can be mechanical stimulation of specific mechano-receptors in pulmonary tissue leading to the lung arc reflex [22][23] and sympathetic activation with the release of vasoconstrictors such as catecholamines [24]. Taken together, these mechanisms are central in promoting brain inflammation, neuronal dysfunction, and neuropathology (Figure 2) (reviewed in [25][26][27][28]).
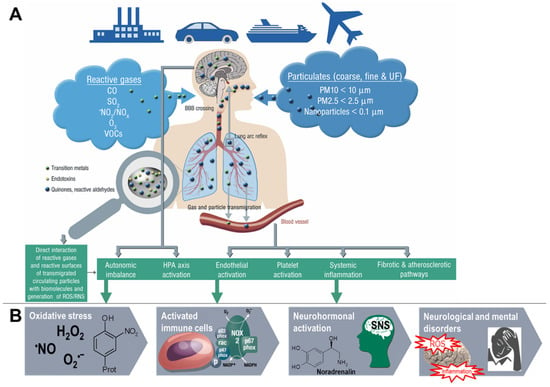
Figure 2. Summary of pathophysiological mechanisms by which air pollutants cause increased oxidative stress, and inflammation, thereby contributing to cerebrovascular, neurological, mental, and cardiorespiratory disorders. (A) Uptake and cardiorespiratory health effects triggered by air pollution constituents. (B) Key events that contribute to neurological and mental by air pollution constituents. Ambient PM particles are often loaded with environmental toxins stemming from particle “aging” by UV-induced photoreactions or modifications upon interaction with reactive gases in the atmosphere [3]. In addition, loading of the particles with environmental endotoxins and heavy metals enhances their direct biochemical reactivity [6][7][8]. Summarized from Münzel et al. [2] (A) and Daiber et al. [29] (B) with permission. Copyright © 2020, Oxford University Press (A) and © 2020 International Union of Biochemistry and Molecular Biology (B). SNS, sympathetic nervous system; UF, ultrafine.
References
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., 3rd; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al.et al Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2012, 121, 2331–2378.
- Munzel, T.; Gori, T.; Al-Kindi, S.; Deanfield, J.; Lelieveld, J.; Daiber, A.; Rajagopalan, S; E ects of gaseous and solid constituents of air pollution on endothelial function. Eur. Heart. J. 2018, 39, 3543–3550.
- Ulrich Pöschl; Manabu Shiraiwa; Multiphase Chemistry at the Atmosphere–Biosphere Interface Influencing Climate and Public Health in the Anthropocene. Chemical Reviews 2015, 115, 4440-4475, 10.1021/cr500487s.
- Hans Orru; K. L. Ebi; B. Forsberg; The Interplay of Climate Change and Air Pollution on Health. Current Environmental Health Reports 2017, 4, 504-513, 10.1007/s40572-017-0168-6.
- European Commission. Air Pollution and Climate Change. Available online: https://ec.europa.eu/environ-ment/integration/research/newsalert/pdf/24si_en.pdf (accessed on 4 May 2020).
- David Peden; Pollutants and asthma: role of air toxics. Environmental Health Perspectives 2002, 110, 565-568, 10.1289/ehp.110-1241207.
- Per E. Schwarze; J. Øvrevik; R. B. Hetland; R. Becher; F. R. Cassee; M. Låg; M. Løvik; E. Dybing; M. Refsnes; Importance of Size and Composition of Particles for Effects on Cells In Vitro. Inhalation Toxicology 2007, 19, 17-22, 10.1080/08958370701490445.
- Ryohei Miyata; Stephan F. Van Eeden; The innate and adaptive immune response induced by alveolar macrophages exposed to ambient particulate matter. Toxicology and Applied Pharmacology 2011, 257, 209-226, 10.1016/j.taap.2011.09.007.
- Thomas Münzel; Sebastian Steven; Ms. Katie Frenis; Jos Lelieveld; Omar Hahad; Andreas Daiber; Environmental Factors Such as Noise and Air Pollution and Vascular Disease. Antioxidants & Redox Signaling 2020, -, -, 10.1089/ars.2020.8090.
- World Health Organization. Report on the Global Tobacco Epidemic, 2017 Monitoring Tobacco Use and Prevention Policies. Available online: https://apps.who.int/iris/bitstream/handle/10665/255874/9789241512824-eng.pdf?sequence=1 (accessed on 4 May 2020).
- Lelieveld, J.; Pozzer, A.; Poschl, U.; Fnais, M.; Haines, A.; Munzel, T. Loss of life expectancy from air pollution compared to other risk factors: A worldwide perspective. Cardiovasc. Res. 2020.
- Daiber, A.; Steven, S.; Weber, A.; Shuvaev, V.V.; Muzykantov, V.R.; Laher, I.; Li, H.; Lamas, S.; Munzel, T; Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017, 174, 1591–1619.
- Munzel, T.; Sinning, C.; Post, F.; Warnholtz, A.; Schulz, E; Pathophysiology, diagnosis and prognostic implications of endothelial dysfunction. Ann. Med. 2008, 40, 180–196.
- Valery Feigin; Gregory A Roth; Mohsen Naghavi; Priya Parmar; Rita Krishnamurthi; Sumeet Chugh; George A. Mensah; Bo Norrving; Ivy Shiue; Marie Ng; et al.Kara EstepKelly CercyChristopher J L MurrayMohammad H Forouzanfar Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet Neurology 2016, 15, 913-924, 10.1016/s1474-4422(16)30073-4.
- Gabriele Cipriani; Sabrina Danti; Cecilia Carlesi; Gemma Borin; Danger in the Air: Air Pollution and Cognitive Dysfunction. American Journal of Alzheimer's Disease & Other Dementiasr 2018, 33, 333-341, 10.1177/1533317518777859.
- Simon J. Wilson; Mark R. Miller; David Newby; Effects of Diesel Exhaust on Cardiovascular Function and Oxidative Stress. Antioxidants & Redox Signaling 2018, 28, 819-836, 10.1089/ars.2017.7174.
- Paula Valencia Moulton; Wei Yang; Air Pollution, Oxidative Stress, and Alzheimer's Disease. Journal of Environmental and Public Health 2012, 2012, 472751, 10.1155/2012/472751.
- Xiaoquan Rao; Jixin Zhong; Robert D. Brook; Sanjay Rajagopalan; Effect of Particulate Matter Air Pollution on Cardiovascular Oxidative Stress Pathways. Antioxidants & Redox Signaling 2018, 28, 797-818, 10.1089/ars.2017.7394.
- Lilian Calderón-Garcidueñas; Anna C. Solt; Carlos Henríquez-Roldán; Ricardo Torres-Jardón; Bryan Nuse; Lou Herritt; Rafael Villarreal-Calderón; Norma Osnaya; Ida Stone; Raquel García; et al.Diane M. BrooksAngelica González-MacielR Reynoso-RoblesRicardo Delgado-ChávezWilliam Reed Long-term Air Pollution Exposure Is Associated with Neuroinflammation, an Altered Innate Immune Response, Disruption of the Blood-Brain Barrier, Ultrafine Particulate Deposition, and Accumulation of Amyloid β-42 and α-Synuclein in Children and Young Adults. Toxicologic Pathology 2008, 36, 289-310, 10.1177/0192623307313011.
- Sayeh Heidari Nejad; Ryusuke Takechi; Ben Mullins; Corey Giles; Alexander Larcombe; Dean Bertolatti; Krassi Rumchev; Satvinder Dhaliwal; John C. L. Mamo; The effect of diesel exhaust exposure on blood-brain barrier integrity and function in a murine model. Journal of Applied Toxicology 2014, 35, 41-47, 10.1002/jat.2985.
- Somayeh Hajipour; Yaghoub Farbood; Mohammad Kazem Gharib-Naseri; Gholamreza Goudarzi; Mohammad Rashno; Heidar Maleki; Nima Bakhtiari; Ali Nesari; Seyed Esmaeil Khoshnam; Mahin Dianat; et al.Behjat SarkakiAlireza Sarkaki Exposure to ambient dusty particulate matter impairs spatial memory and hippocampal LTP by increasing brain inflammation and oxidative stress in rats. Life Sciences 2020, 242, 117210, 10.1016/j.lfs.2019.117210.
- Ryan K. Robinson; Mark A. Birrell; John J. Adcock; Michael A. Wortley; Eric D. Dubuis; Shu Chen; Catriona M. McGilvery; Sheng Hu; Milo S.P. Shaffer; Sara J. Bonvini; et al.Sarah A. MaherI.S. MudwayAlexandra E. PorterChris CarlstenTeresa D. TetleyMaria G. Belvisi Mechanistic link between diesel exhaust particles and respiratory reflexes. Journal of Allergy and Clinical Immunology 2017, 141, 1074-1084.e9, 10.1016/j.jaci.2017.04.038.
- Christina M. Perez; Mehdi S. Hazari; Aimen K. Farraj; Role of Autonomic Reflex Arcs in Cardiovascular Responses to Air Pollution Exposure. Cardiovascular Toxicology 2014, 15, 69-78, 10.1007/s12012-014-9272-0.
- Hajat, A.; Diez Roux, A.V.; Castro-Diehl, C.; Cosselman, K.; Golden, S.H.; Hazlehurst, M.F.; Szpiro, A.; Vedal, S.; Kaufman, J.D; The Association Between Air Pollution And Stress Hormones: Evidence From The Multi-Ethnic Study Of Atherosclerosis. Environ. Health Perspect. 2019, 127, 57007.
- Richard L. Jayaraj; Eric A. Rodriguez; Yi Wang; Michelle L. Block; Outdoor Ambient Air Pollution and Neurodegenerative Diseases: the Neuroinflammation Hypothesis. Current Environmental Health Reports 2017, 4, 166-179, 10.1007/s40572-017-0142-3.
- Amedeo D'angiulli; Severe Urban Outdoor Air Pollution and Children’s Structural and Functional Brain Development, From Evidence to Precautionary Strategic Action. Frontiers in Public Health 2018, 6, 95, 10.3389/fpubh.2018.00095.
- Chong Chen; Shin Nakagawa; Planetary Health and the Future of Human Capacity: The Increasing Impact of Planetary Distress on the Human Brain. Challenges 2018, 9, 41, 10.3390/challe9020041.
- Michelle L. Block; Lilian Calderón-Garcidueñas; Air pollution: mechanisms of neuroinflammation and CNS disease. Trends in Neurosciences 2009, 32, 506-516, 10.1016/j.tins.2009.05.009.
- Andreas Daiber; Swenja Kröller‐Schön; Katie Frenis; Matthias Oelze; Sanela Kalinovic; Ksenija Vujacic‐Mirski; Marin Kuntic; Maria Teresa Bayo Jimenez; Johanna Helmstädter; Sebastian Steven; et al.Bato KoracThomas Münzel Environmental noise induces the release of stress hormones and inflammatory signaling molecules leading to oxidative stress and vascular dysfunction-Signatures of the internal exposome. BioFactors 2019, 45, 495-506, 10.1002/biof.1506.




