Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Patrizia Limonta | + 2981 word(s) | 2981 | 2021-05-14 11:18:45 | | | |
| 2 | Vivi Li | Meta information modification | 2981 | 2021-06-04 03:17:58 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Limonta, P. Natural Compounds and Prostate Cancer. Encyclopedia. Available online: https://encyclopedia.pub/entry/10489 (accessed on 07 February 2026).
Limonta P. Natural Compounds and Prostate Cancer. Encyclopedia. Available at: https://encyclopedia.pub/entry/10489. Accessed February 07, 2026.
Limonta, Patrizia. "Natural Compounds and Prostate Cancer" Encyclopedia, https://encyclopedia.pub/entry/10489 (accessed February 07, 2026).
Limonta, P. (2021, June 03). Natural Compounds and Prostate Cancer. In Encyclopedia. https://encyclopedia.pub/entry/10489
Limonta, Patrizia. "Natural Compounds and Prostate Cancer." Encyclopedia. Web. 03 June, 2021.
Copy Citation
Prostate cancer (PCa) represents a major cause of cancer mortality among men in developed countries. Patients with recurrent disease initially respond to androgen-deprivation therapy, but the tumor eventually progresses into castration-resistant PCa; in this condition, tumor cells acquire the ability to escape cell death and develop resistance to current therapies. Thus, new therapeutic approaches for PCa management are urgently needed. In this setting, natural products have been extensively studied for their anti-PCa activities, such as tumor growth suppression, cell death induction, and inhibition of metastasis and angiogenesis.
prostate cancer
natural compounds
phytochemicals
chemoprevention
novel therapeutic strategies
1. Introduction
Globally, prostate cancer (PCa) is the most frequently diagnosed tumor in men, being particularly common in Western countries [1]. In about 90% of cases, PCa is still organ-confined or only locally advanced at diagnosis, which makes it effectively treatable with prostatectomy or local radiotherapy. However, 30–40% of patients usually experience progression of disease [2]; at this stage, where tumor growth depends on androgens, the most effective treatment is represented by androgen-deprivation therapy, aimed at blocking hormone secretion and/or activity. This therapy is based on pharmacological castration, obtained by administration of GnRH agonists, alone or in combination with antiandrogens [3][4]; more recently, two major clinical trials, CHAARTED and STAMPEDE, have also demonstrated benefits of early initiation of chemotherapy concomitantly with hormonal therapy [5][6]. However, despite a good initial response, relapse occurs in the majority of patients within 2–3 years, and the tumor progresses towards a condition of resistance to castration [7]. Improved therapeutic options for castration-resistant patients are needed, since taxane-based (i.e., docetaxel) treatment and immunotherapy, as well as the novel therapies with enzalutamide and abiraterone, generally offer a progression-free survival of a few months [8][9]. Parallelly, bone metastases, occurring in 80% of advanced PCas and usually treated with radiation therapy and chemotherapy, are associated with considerable morbidity, adversely affect quality of life and several skeletal-related events [4][10]. Therefore, in the last years natural compounds have gained a lot of interest, due to their various anti-cancer effects. In fact, accumulating evidence has highlighted that nutraceuticals can exert growth-suppressing, pro-death, anti-metastatic, and anti-angiogenic activity in PCa cell lines and xenografts, while sparing normal prostate epithelial cells [11]. In particular, several mechanisms are involved in the anti-PCa actions of these molecules, including inhibition of androgen receptor (AR) axis and targeting of cancer stemness [12][13].
2. Natural Compounds with Potential to Treat Prostate Cancer
Data from literature have pointed out that several natural products can selectively target numerous molecules and signaling pathways implicated in tumor development and progression [11][12][13]. Many of them have been tested in in vitro and in vivo studies, while some clinical trials have been conducted or are currently ongoing [11][12][13]. Among these naturally occurring molecules, quercetin, fisetin, luteolin, apigenin, curcumin, resveratrol, genistein, silibinin, kaempferol, epigallocatechin-3-gallate (EGCG), tocotrienols, sulforaphane, ginsenosides, ursolic acid, berberine, honokiol, xanthoumol, oridonin, and tannic acid have shown outstanding potential as anti-PCa agents in in vitro and preclinical experiments (Figure 1).
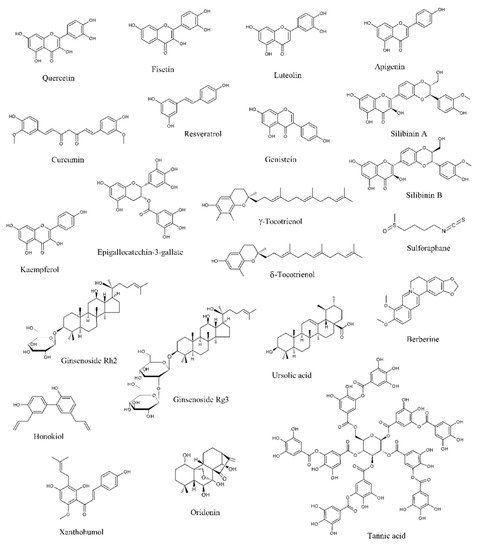
Figure 1. Chemical structures of the major anti-prostate cancer (PCa) phytochemicals.
2.1. Natural Compounds Modulating the Androgen Receptor Axis
A number of studies indicates that PCa growth and progression are driven by the AR, a ligand-dependent transcription factor and member of the nuclear receptor family [14]. The AR is encoded by the AR gene located on the X chromosome at Xq11-12 and displays a N-terminal regulatory domain, a DNA-binding domain (DBD), a ligand-binding domain (LBD), and a C-terminal domain. In the absence of androgens, particularly dihydrotestosterone (DHT) and testosterone, it is complexed with chaperone proteins, heat-shock protein 90 (Hsp90) and 70 (Hsp70), in the cell cytoplasm. Upon ligand binding, it is transferred to the nucleus, where it homodimerizes due to the interactions of dedicated motifs in the DBD and in the LBD. Then, the dimerized receptor recognizes cognate DNA response elements in regulatory regions located in proximal or more distal intra- and inter-genic regions of androgen target genes [15][16]. It then recruits different coregulator proteins and epigenetic factors to generate a transcriptionally active complex able to upregulate downstream pro-survival gene expression [14].
Given its fundamental role in PCa cell proliferation, the AR signaling represents a crucial target for PCa management. In this context, pharmacological castration obtained via androgen-deprivation therapy is currently the most effective strategy for PCa treatment. However, PCa often becomes castration resistant [8][9]. One of the mechanisms underlying this change is an enhanced AR expression in the tumor cell. In particular, it has been shown that 28% of cancers resistant to androgen-deprivation therapy display AR upregulation due to amplification of its gene [17]. Another mechanism responsible for PCa androgen-independent growth is ligand promiscuity, caused by mutations of the AR gene that lead to amino acid substitutions in the LBD and subsequent decrease in the specificity and selectivity for ligands: the most common of them are T877A, F876L, W741L, and L701H. These mutant AR proteins bind to other steroids, including progesterone, estrogens, and glucocorticoids, which can activate the AR signaling pathway and promote PCa progression [18]. AR activation via ligand-independent mechanisms represents the third mechanism of androgen-independent PCa development [19]. Indeed, it has been found that tyrosine kinase receptor-activating ligands, such as epidermal growth factor (EGF) and insulin-like growth-factor-1 (IGF-1), can activate the AR through the phosphoinositide 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) pathway [20][21][22][23][24]. Finally, various AR splice variants lacking the LBD have been recently reported: the AR N-terminal domain becomes constitutively active in the absence of the LBD, thereby promoting castration resistant proliferation [25][26].
Interestingly, various phytochemicals have been shown to modulate AR expression and activity.
Quercetin is a penta-hydroxylated flavonol, naturally occurring in tea, onions, apples, tomatoes, and capers and endowed with important chemopreventive and anti-cancer properties [27]. Yuan et al. demonstrated that in LNCaP PCa cells a protein complex containing the AR, specific protein 1 (Sp1) and c-Jun was generated in response to quercetin treatment and suppressed AR function. This resulted in the inhibition of the production of the prostate-specific, androgen-related tumor markers prostate-specific antigen (PSA) and human kallikrein-2 (hK2), as well as in the downregulation of androgen-related genes, such as ornithine decarboxylase (ODC) and NKX3.1 [28][29][30][31]. Interestingly, quercetin was also able to repress the expression of the AR splice variant 7 (AR-V7), which correlates to resistance to enzalutamide and poor prognosis, via Hsp70 inhibition [32].
Fisetin, a flavonol present in strawberries, apples, persimmons, onions, kiwi, and cucumbers, has been recently demonstrated to exert not only potent neuroprotective effects but also different anti-tumor activities [33][34]. In PCa, it was shown to specifically bind to the AR LBD. This interaction resulted in a decreased AR stability and amino-terminal/carboxyl-terminal (N-C) interaction, leading to a reduced transactivation of AR target genes. Moreover, fisetin treatment of LNCaP cells was followed by a downregulation of AR levels, due to a reduction in its promoter activity and to an increase of its degradation. In this cell line, the flavonol also synergized with bicalutamide in promoting apoptotic cell death. Finally, in AR-positive CWR22υ1 PCa cell-bearing mice, fisetin inhibited tumor growth and decreased PSA serum levels, suggesting that this compound is able to suppress AR activity also in vivo [35].
Luteolin, a flavone abundant in rosemary, thyme, parsley, broccoli, and celery, is characterized by anti-inflammatory, neuroprotective, and anti-cancer activity [36][37]. It was observed to induce a dose- and time-dependent decrease in AR mRNA and protein expression, as well as of intracellular and secreted PSA levels, in PCa cells. In particular, it appears to promote the AR-Hsp90 complex dissociation, causing AR degradation via the proteasome-ubiquitin pathway [38].
Curcumin is a polyphenol extracted from turmeric (Curcuma longa), which has shown great therapeutic potential [39][40][41]. This compound was demonstrated not only to decrease the expression of AR and AR-related cofactors, such as activator protein-1 (AP-1), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), CREB-binding protein (CBP), and NKX3.1, but also to reduce testosterone production in PCa cell lines and xenografts. This reduction in testosterone levels was associated with a downregulation of steroidogenic acute regulatory proteins, including cytochrome P450 11A1 (CYP11A1) and 3-beta-hydroxysteroid dehydrogenase 2 (HSD3B2), and in an enhanced expression of aldo-keto reductase 1C2 (AKR1C2), a 3-ketosteroid reductase responsible for the elimination of 5alpha-DHT and subsequent inactivation of AR [42][43][44][45].
Resveratrol is a grape-derived polyphenol that possesses numerous health benefits, including various chemopreventive effects [46]. It was found to target the AR axis in different in vitro and in vivo PCa models [47][48][49][50][51]. On one hand, in LNCaP cells it inhibited β-catenin nuclear translocation through hypoxia-inducible factor 1-α (HIF-1α) downregulation, thus suppressing β-catenin-mediated AR signaling [52]; similarly, it also repressed interleukin-6 (IL-6)-induced AR transcriptional activity [53]. On the other hand, in 22RV1 cells it promoted the AR splice variant ARV7 proteasomal degradation, by enhancing its polyubiquitination. These data indicate that resveratrol could be used not only for the treatment of androgen-responsive PCa but also for the management of the ARV7-positive castration-resistant tumor [54].
Genistein is a common phytoestrogen that can be obtained from soybeans [55]. Indeed, it was shown to inhibit the AR signaling via estrogen receptor-β (ER-β) and estrogen-related pathways, as well as through suppression of Akt/Forkhead box O3a (FOXO3a)/glycogen synthase kinase 3β (GSK-3β) and histone deacetylase 6 (HDAC6)-Hsp90 function, needed to stabilize the AR [56][57][58][59]. Notably, in a recent study by Mahmoud et al., genistein was also demonstrated to bind to both the wild and the T877A-mutant types of AR, specifically competing with androgens. In particular, while it suppressed proliferation of AR wild-type LAPC-4 cells, it exerted a dual role in T877A-mutated LNCaP and PC3 cell lines, by stimulating cell growth at lower doses and inducing cell death at higher concentrations [60]. Finally, in PCa cells genistein downregulated prostate androgen-regulated transcript-1 (PART-1) gene expression induced by DHT, thus affecting cell proliferation [61].
2.2. Natural Compounds Affecting Proliferation
Numerous natural compounds have been reported to exert growth-suppressive and anti-proliferative activities in PCa cells and xenografts.
Epidermal growth factor receptor (EGFR) is a receptor tyrosine kinase whose activation is associated with an increase in cell growth and survival, which explains why EGFR is commonly overexpressed/overactivated in tumors of epithelial origin, including PCa. In particular, after binding to its specific ligands, such as EGF and transforming growth factor α (TGFα), it triggers several downstream signaling pathways, including PI3K/Akt/mTOR, mitogen-activated protein kinases (MAPKs), Hedgehog (Hh) signaling, and NF-κB [76]. Many phytochemicals, including quercetin, luteolin, resveratrol, genistein, and berberine, have been shown to reduce EGFR levels, as well as to suppress its intrinsic tyrosine kinase activity and its ligand-induced activation, in different PCa cell lines and in vivo models [77][78][79][80][81].
The IGF axis is a complex signaling network implicated in different tumorigenic processes, particularly in cancer proliferation, survival, and metabolism. It involves the interaction between the peptide-ligands IGF1 and IGF2 and the receptors IGF1R and IGF2R, and its activation elicits downstream signals, such as the PI3K/AKT and the MAPK pathways [82]. Interestingly, the IGF axis represents a major target for the anti-PCa action of silibinin, a flavonoid endowed with antioxidant properties commonly found in the milk thistle (Silybum marianum) [83][84]. Indeed, it decreased IGF1 expression and increased IGFBP-3 levels in transgenic adenocarcinoma of the mouse prostate (TRAMP) models, thus inhibiting tumor growth and progression [85][86][87]. Similar results were also obtained after treatment of PCa-bearing mice with luteolin [88].
Emerging evidence has highlighted the key role played by the PI3K/AKT pathway in the development of castration resistant PCa. This cascade, which is activated in most of advanced PCas, acts as a fundamental driver for tumor cell proliferation, thereby allowing cancer cells to survive to the androgen deprivation-related cytotoxicity. Moreover, preclinical studies have highlighted a strict correlation between the PI3K/AKT and AR axes, evidencing a dynamic cross-talk between these cascades in the acquisition of androgen-deprivation therapy resistance. Therefore, there is an evident rationale for the development of novel PI3K inhibitors, which may be able to block castration-resistant PCa growth and survival [89]. In this setting, the interest in natural products has recently increased, due to their ability to specifically target the PI3K/AKT cascade. In particular, quercetin, apigenin, curcumin, genistein, sulforaphane, and EGCG have been demonstrated to attenuate PCa cell growth by downregulating this signaling pathway [90][91][92][93][94][95][96][97][98].
During PCa progression, both tumor invasion and chemoresistance are promoted by NF-κB. Indeed, constitutive activation of this protein has been commonly found in primary PCas and it is associated with AR loss and castration-resistant features. Thus, NF-κB is an important target for PCa management, owing to its role in tumorigenesis and therapy resistance [99]. Notably, downregulation of this protein and of its target genes has been highlighted after resveratrol, genistein, sulforaphane, ursolic acid, tocotrienol, and celastrol treatment [100][101][102][103][104][105].
Hh pathway activation is implicated in the development of different types of tumors, including PCa. In particular, many studies have pointed out that this signaling plays a crucial role in the progression of PCa to more aggressive and chemoresistant states [106]. Slusarz et al. demonstrated that seven common nutraceuticals, (i.e., genistein, curcumin, EGCG, resveratrol, apigenin, baicalein, and quercetin) can suppress the Hh pathway both in vitro and in vivo, with four of them (i.e., genistein, curcumin, resveratrol, and EGCG) decreasing not only Hh effector Gli1 expression but also Gli1 reporter activity [107].
Genome sequencing and gene expression analyses have evidenced the importance of the Wnt pathway in the development of castration resistant PCa [108]. Wnt signaling is also implicated in the cross-talk with the PCa microenvironment, where this protein is secreted by the tumor stroma and promotes therapy resistance, as well as in PCa stem cell self-renewal or expansion [109]. Preclinical studies have illustrated the potential of Wnt inhibitors in preventing PCa progression. Some of them have already been tested in phase I trials, although they have not been administered to PCa patients yet [108][109]. Interestingly, treatment of PCa cells with quercetin, curcumin, genistein, and silibinin resulted in growth suppression through Wnt cascade modulation [110][111][112][113].
MicroRNAs (miRNAs) are endogenous, ≈22 nucleotides, non-coding RNAs able to induce both transcriptional and translational arrest, thus functioning as either oncogenes or oncosuppressors, depending on the specific tumor type [114]. Concerning PCa, genistein has shown promise in modulating the levels of different oncogenic (i.e., miR221, miR222, miR151, and miR1260b) and oncosuppressor (i.e., miR-574-3p and miR34a) miRNAs, thus affecting cancer cell proliferation [115][116][117][118][119][120]. Similar encouraging data were also obtained from in vitro studies with luteolin, curcumin, resveratrol, ginsenoside Rh2, and celastrol [121][122][123][124][125][126].
2.3. Natural Compounds Inducing Canonical and Non-Canonical Cell Deaths
Apoptosis is commonly induced in PCa cells and xenografts treated with phytochemicals. In particular, many natural products have been found to trigger both the extrinsic and intrinsic apoptotic pathways, by activating cell surface death receptors, altering Bax/Bcl-2 ratio, increasing p21 levels and triggering caspase-8, -9, -3, and poly (ADP-ribose) polymerase (PARP) cleavage [127][128][129][130][131][132][133][134][135][136][137][138][139][140][141][142][143][144][145][146][147][148][149][150][151][152][153]. In this setting, proteostasis disruption appears to play a key role in the modulation of the nutraceutical-related apoptotic cell death. Indeed, while apigenin, luteolin, genistein, and celastrol inhibited the proteasomal activity and caused ubiquitinated protein accumulation in different PCa cell lines [154][155][156], quercetin, curcumin, silibinin, and tannic acid induced endoplasmic reticulum (ER) stress [157][158][159][160], a condition where unfolded/misfolded proteins accumulate in the ER lumen and promote the activation of distinct pro-death cascades, including the double-stranded RNA-dependent protein kinase PKR-like ER kinase (PERK)/eukaryotic initiation factor 2α (eIF2α)/activating transcription factor 4 (ATF4)/C/EBP homologous protein (CHOP) pathway and the inositol-requiring enzyme 1α (IRE1)/c-Jun N-terminal kinase (JNK)/p38 MAPK cascade [161]. Notably, curcumin- and silibinin-mediated ER stress was associated with generation of reactive oxygen species (ROS) and redox homeostasis alteration [159][162], which were also observed in resveratrol- and sulforaphane-treated PCa cells [163][164][165][166].
Interestingly, apoptotic cell death is not the only death mode triggered by natural compounds.
Berberine is a benzylisoquinoline alkaloid commonly found in the plants of the genus Berberis [167][168]. In a recent study by Zhang et al., it was shown to induce programmed necrosis in LNCaP and PC-82 PCa cell lines. In particular, mitochondrial protein cyclophilin-D (Cyp-D) was observed to be crucially involved in the modulation of berberine-related necrotic cell death. Indeed, berberine treatment resulted in ROS production, which promoted p53 translocation to mitochondria and its interaction with Cyp-D to open the mitochondrial permeability transition pore (mPTP), ultimately leading to necrosis induction [169]. Pro-necrotic effects were also exerted by curcumin in DU145 cells [170].
Paraptosis is a programmed cell death mode characterized by cytoplasmic vacuolation, particularly by ER dilatation and mitochondrial swelling [171][172]. Recently, we have demonstrated that δ-tocotrienol, a vitamin E derivative particularly abundant in annatto seeds, rice bran, and palm oil [173][174], can trigger both apoptosis and paraptosis in PC3 and DU145 cell lines. The mechanisms underlying its pro-paraptotic effects were found to correlate with activation of JNK and p38, as well as with proteotoxicity, since not only the protein synthesis inhibitor cycloheximide but also the ER stress inhibitor salubrinal successfully prevented the cytoplasmic vacuolation evoked by the treatment with this natural compound [175]. Similarly, paraptosis-like cytoplasmic vacuolation was also observed in celastrol-treated PC3 cells [176].
Autophagy is an evolutionarily conserved catabolic process generally used by the cell to eliminate cytoplasmic material, including misfolded proteins and damaged organelles, via lysosomal degradation: it involves the formation of double-membrane vesicles, the autophagosomes, that promote cytoplasmic cargo recycling after fusion with lysosomes, and it is regulated by different proteins, particularly by microtubule-associated proteins 1A/1B light chain 3B, commonly called LC3 [177]. It is now well known that autophagy can act as both tumor promoter and suppressor. The dual role of this mechanism in cancer cells apparently depends on tumor type, stage, and genetic context. Indeed, while on one hand the autophagic flux clearly suppresses tumorigenesis, on the other hand it acts as a key survival mechanism in response to stress, thus promoting cancer cell proliferation. In the context of PCa, curcumin, sulforaphane, silibinin, ursolic acid, honokiol, and oridonin triggered cytoprotective autophagy [178][179][180][181][182][183][184]; on the contrary, fisetin, resveratrol, and celastrol treatment resulted in autophagic cell death [185][186][187]. In particular, the fisetin- and resveratrol-mediated autophagic flux was associated with Akt/mTOR signaling pathway downregulation and AMP-activated protein kinase (AMPK) activation [185][186]. The autophagy induced by celastrol, a pentacyclic triterpenoid extracted from Tripterygium Wilfordi roots [188], was instead correlated to suppression of AR/miR-101 cascade [187].
References
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; Dandona, L.; et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015. JAMA Oncol. 2017, 3, 524.
- Stephenson, A.J.; Scardino, P.T.; Eastham, J.A.; Bianco, F.J., Jr.; Dotan, Z.A.; Fearn, P.A.; Kattan, M.W. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J. Natl. Cancer Inst. 2006, 98, 715–717.
- Perlmutter, M.A.; Lepor, H. Androgen deprivation therapy in the treatment of advanced prostate cancer. Rev. Urol. 2007, 9, S3–S8.
- Thomas, T.S.; Pachynski, R.K. Treatment of advanced prostate cancer. Mo. Med. 2018, 115, 156–161.
- Sweeney, C.J.; Chen, Y.H.; Carducci, M.; Liu, G.; Jarrard, D.F.; Eisenberger, M.; Wong, Y.N.; Hahn, N.; Kohli, M.; Cooney, M.M.; et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl. J. Med. 2015, 373, 737–746.
- James, N.D.; Sydes, M.R.; Clarke, N.W.; Mason, M.D.; Dearnaley, D.P.; Spears, M.R.; Ritchie, A.W.; Parker, C.C.; Russell, J.M.; Attard, G.; et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): Survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 2016, 387, 1163–1177.
- Limonta, P.; Moretti, R.M.; Marzagalli, M.; Montagnani Marelli, M. Castration Resistant Prostate Cancer: From emerging molecular pathways to targeted therapeutic approaches. Clin. Cancer Drugs. 2014, 1, 11–27.
- Nelson, A.W.; Shah, N. Prostate cancer. Surg. (United Kingdom) 2019, 37, 500–507.
- Teo, M.Y.; Rathkopf, D.E.; Kantoff, P. Treatment of advanced prostate cancer. Annu. Rev. Med. 2019, 70, 479–499.
- Cathomas, R.; Bajory, Z.; Bouzid, M.; El Ghoneimy, A.; Gillessen, S.; Goncalves, F.; Kacso, G.; Kramer, G.; Milecki, P.; Pacik, D.; et al. Management of bone metastases in patients with castration-resistant prostate cancer. Urol. Int. 2014, 92, 377–386.
- Salehi, B.; Fokou, P.V.T.; Yamthe, L.R.T.; Tali, B.T.; Adetunji, C.O.; Rahavian, A.; Mudau, F.N.; Martorell, M.; Setzer, W.N.; Rodrigues, C.F.; et al. Phytochemicals in Prostate Cancer: From Bioactive Molecules to Upcoming Therapeutic Agents. Nutrients. 2019, 11, 1483.
- Kallifatidis, G.; Hoy, J.J.; Lokeshwar, B.L. Bioactive natural products for chemoprevention and treatment of castration-resistant prostate cancer. Semin. Cancer Biol. 2016, 40–41, 160–169.
- Taylor, W.F.; Jabbarzadeh, E. The use of natural products to target cancer stem cells. Am. J. Cancer Res. 2017, 7, 1588–1605.
- Dai, C.; Heemers, H.; Sharifi, N. Androgen signaling in prostate cancer. Cold Spring Harb. Perspect. Med. 2017, 7, a030452.
- Nadal, M.; Prekovic, S.; Gallastegui, N.; Helsen, C.; Abella, M.; Zielinska, K.; Gay, M.; Vilaseca, M.; Taulès, M.; Houtsmuller, A.B.; et al. Structure of the homodimeric androgen receptor ligand-binding domain. Nat. Commun. 2017, 8, 14388.
- van Royen, M.E.; van Cappellen, W.A.; de Vos, C.; Houtsmuller, A.B.; Trapman, J. Stepwise androgen receptor dimerization. J. Cell Sci. 2012, 125, 1970–1979.
- Koivisto, P.; Kononen, J.; Palmberg, C.; Tammela, T.; Hyytinen, E.; Isola, J.; Trapman, J.; Cleutjens, K.; Noordzij, A.; Visakorpi, T.; et al. Androgen receptor gene amplification: A possible molecular mechanism for androgen deprivation therapy failure in prostate cancer. Cancer Res. 1997, 57, 314–319.
- Buchanan, G.; Greenberg, N.M.; Scher, H.I.; Harris, J.M.; Marshall, V.R.; Tilley, W.D. Collocation of androgen receptor gene mutations in prostate cancer. Clin. Cancer Res. 2001, 7, 1273–1281.
- Jenster, G. Ligand-independent activation of the androgen receptor in prostate cancer by growth factors and cytokines. J. Pathol. 2000, 191, 227–228.
- Green, S.M.; Mostaghel, E.A.; Nelson, P.S. Androgen action and metabolism in prostate cancer. Mol. Cell. Endocrinol. 2012, 360, 3–13.
- Mellinghoff, I.K.; Vivanco, I.; Kwon, A.; Tran, C.; Wongvipat, J.; Sawyers, C.L. HER2/neu kinase-dependent modulation of androgen receptor function through effects on DNA binding and stability. Cancer Cell 2004, 6, 517–527.
- Mahajan, N.P.; Liu, Y.; Majumder, S.; Warren, M.R.; Parker, C.E.; Mohler, J.L.; Earp, H.S.; Whang, Y.E. Activated Cdc42-associated kinase Ack1 promotes prostate cancer progression via androgen receptor tyrosine phosphorylation. Proc. Natl. Acad. Sci. U. S. A. 2007, 104, 8438–8443.
- Liu, Y.; Karaca, M.; Zhang, Z.; Gioeli, D.; Earp, H.S.; Whang, Y.E. Dasatinib inhibits site-specific tyrosine phosphorylation of androgen receptor by Ack1 and Src kinases. Oncogene 2010, 29, 3208–3216.
- Kraus, S.; Gioeli, D.; Vomastek, T.; Gordon, V.; Weber, M.J. Receptor for activated C kinase 1 (RACK1) and Src regulate the tyrosine phosphorylation and function of the androgen receptor. Cancer Res. 2006, 66, 11047–11054.
- Sharifi, N. Mechanisms of androgen receptor activation in castration-resistant prostate cancer. Endocrinology 2013, 154, 4010–4017.
- Guo, Z.; Yang, X.; Sun, F.; Jiang, R.; Linn, D.E.; Chen, H.; Chen, H.; Kong, X.; Melamed, J.; Tepper, C.G.; et al. A novel androgen receptor splice variant is up-regulated during prostate cancer progression and promotes androgen depletion-resistant growth. Cancer Res. 2009, 69, 2305–2313.
- Rauf, A.; Imran, M.; Khan, I.A.; Ur-Rehman, M.-; Gilani, S.A.; Mehmood, Z.; Mubarak, M.S. Anticancer potential of quercetin: A comprehensive review. Phyther. Res. 2018, 32, 2109–2130.
- Xing, N. Quercetin inhibits the expression and function of the androgen receptor in LNCaP prostate cancer cells. Carcinogenesis 2001, 22, 409–414.
- Yuan, H.; Pan, Y.; Young, C.Y.F. Overexpression of c-Jun induced by quercetin and resverol inhibits the expression and function of the androgen receptor in human prostate cancer cells. Cancer Lett. 2004, 213, 155–163.
- Yuan, H.; Gong, A.; Young, C.Y.F. Involvement of transcription factor Sp1 in quercetin-mediated inhibitory effect on the androgen receptor in human prostate cancer cells. Carcinogenesis 2005, 26, 793–801.
- Yuan, H.; Young, C.Y.F.; Tian, Y.; Liu, Z.; Zhang, M.; Lou, H. Suppression of the androgen receptor function by quercetin through protein-protein interactions of Sp1, c-Jun, and the androgen receptor in human prostate cancer cells. Mol. Cell. Biochem. 2010, 339, 253–262.
- Kita, K.; Shiota, M.; Tanaka, M.; Otsuka, A.; Matsumoto, M.; Kato, M.; Tamada, S.; Iwao, H.; Miura, K.; Nakatani, T.; et al. Heat shock protein 70 inhibitors suppress androgen receptor expression in LNCaP95 prostate cancer cells. Cancer Sci. 2017, 108, 1820–1827.
- Pal, H.C.; Pearlman, R.L.; Afaq, F. Fisetin and its role in chronic diseases. Adv. Exp. Med. Biol. 2016, 928, 213–244.
- Lall, R.K.; Adhami, V.M.; Mukhtar, H. Dietary flavonoid fisetin for cancer prevention and treatment. Mol. Nutr. Food Res. 2016, 60, 1396–1405.
- Khan, N.; Asim, M.; Afaq, F.; Zaid, M.A.; Mukhtar, H. A novel dietary flavonoid fisetin inhibits androgen receptor signaling and tumor growth in athymic nude mice. Cancer Res. 2008, 68, 8555–8563.
- Nabavi, S.F.; Braidy, N.; Gortzi, O.; Sobarzo-Sanchez, E.; Daglia, M.; Skalicka-Woźniak, K.; Nabavi, S.M. Luteolin as an anti-inflammatory and neuroprotective agent: A brief review. Brain Res. Bull. 2015, 119, 1–11.
- Imran, M.; Rauf, A.; Abu-Izneid, T.; Nadeem, M.; Shariati, M.A.; Khan, I.A.; Imran, A.; Orhan, I.E.; Rizwan, M.; Atif, M.; et al. Luteolin, a flavonoid, as an anticancer agent: A review. Biomed. Pharmacother. 2019, 112, 108612.
- Chiu, F.L.; Lin, J.K. Downregulation of androgen receptor expression by luteolin causes inhibition of cell proliferation and induction of apoptosis in human prostate cancer cells and xenografts. Prostate 2008, 68, 61–71.
- Pulido-Moran, M.; Moreno-Fernandez, J.; Ramirez-Tortosa, C.; Ramirez-Tortosa, M.C. Curcumin and health. Molecules 2016, 21, 264.
- Kunnumakkara, A.B.; Bordoloi, D.; Padmavathi, G.; Monisha, J.; Roy, N.K.; Prasad, S.; Aggarwal, B.B. Curcumin, the golden nutraceutical: Multitargeting for multiple chronic diseases. Br. J. Pharmacol. 2017, 174, 1325–1348.
- Tomeh, M.A.; Hadianamrei, R.; Zhao, X. A review of curcumin and its derivatives as anticancer agents. Int. J. Mol. Sci. 2019, 20, 1033.
- Nakamura, K.; Yasunaga, Y.; Segawa, T.; Ko, D.; Moul, J.; Srivastava, S.; Rhim, J. Curcumin down-regulates AR gene expression and activation in prostate cancer cell lines. Int. J. Oncol. 2002, 21, 825–830.
- Zhang, H.N.; Yu, C.X.; Zhang, P.J.; Chen, W.W.; Jiang, A.L.; Kong, F.; Deng, J.T.; Zhang, J.Y.; Young, C.Y.F. Curcumin downregulates homeobox gene NKX3.1 in prostate cancer cell LNCaP. Acta Pharmacol. Sin. 2007, 28, 423–430.
- Guo, H.; Xu, Y.-M.; Ye, Z.-Q.; Yu, J.-H.; Hu, X.-Y. Curcumin induces cell cycle arrest and apoptosis of prostate cancer cells by regulating the expression of IkappaBalpha, c-Jun and androgen receptor. Pharmazie 2013, 68, 431–434.
- Ide, H.; Lu, Y.; Noguchi, T.; Muto, S.; Okada, H.; Kawato, S.; Horie, S. Modulation of AKR1C2 by curcumin decreases testosterone production in prostate cancer. Cancer Sci. 2018, 109, 1230–1238.
- Rauf, A.; Imran, M.; Butt, M.S.; Nadeem, M.; Peters, D.G.; Mubarak, M.S. Resveratrol as an anti-cancer agent: A review. Crit. Rev. Food Sci. Nutr. 2018, 58, 1428–1447.
- Gao, S.; Liu, G.-Z.; Wang, Z. Modulation of androgen receptor-dependent transcription by resveratrol and genistein in prostate cancer cells. Prostate 2004, 59, 214–225.
- Jones, S.B.; DePrimo, S.E.; Whitfield, M.L.; Brooks, J.D. Resveratrol-induced gene expression profiles in human prostate cancer cells. Cancer Epidemiol. Biomarkers Prev. 2005, 14, 596–604.
- Benitez, D.A.; Pozo-Guisado, E.; Clementi, M.; Castellón, E.; Fernandez-Salguero, P.M. Non-genomic action of resveratrol on androgen and oestrogen receptors in prostate cancer: Modulation of the phosphoinositide 3-kinase pathway. Br. J. Cancer 2007, 96, 1595–1604.
- Harada, N.; Murata, Y.; Yamaji, R.; Miura, T.; Inui, H.; Nakano, Y. Resveratrol down-regulates the androgen receptor at the post-translational level in prostate cancer cells. J. Nutr. Sci. Vitaminol. (Tokyo) 2007, 53, 556–560.
- Wang, T.T.Y.; Hudson, T.S.; Wang, T.C.; Remsberg, C.M.; Davies, N.M.; Takahashi, Y.; Kim, Y.S.; Seifried, H.; Vinyard, B.T.; Perkins, S.N.; et al. Differential effects of resveratrol on androgen-responsive LNCaP human prostate cancer cells in vitro and in vivo. Carcinogenesis 2008, 29, 2001–2010.
- Mitani, T.; Harada, N.; Tanimori, S.; Nakano, Y.; Inui, H.; Yamaji, R. Resveratrol inhibits hypoxia-inducible factor-1α-mediated androgen receptor signaling and represses tumor progression in castration-resistant prostate cancer. J. Nutr. Sci. Vitaminol. 2014, 60, 276–282.
- Lee, M.H.; Kundu, J.K.; Keum, Y.S.; Cho, Y.Y.; Surh, Y.J.; Choi, B.Y. Resveratrol inhibits IL-6-induced transcriptional activity of AR and STAT3 in human prostate cancer LNCaP-FGC cells. Biomol. Ther. 2014, 22, 426–430.
- Wilson, S.; Cavero, L.; Tong, D.; Liu, Q.; Geary, K.; Talamonti, N.; Xu, J.; Fu, J.; Jiang, J.; Zhang, D. Resveratrol enhances polyubiquitination-mediated ARV7 degradation in prostate cancer cells. Oncotarget 2017, 8, 54683–54693.
- Tuli, H.S.; Tuorkey, M.J.; Thakral, F.; Sak, K.; Kumar, M.; Sharma, A.K.; Sharma, U.; Jain, A.; Aggarwal, V.; Bishayee, A. Molecular mechanisms of action of genistein in cancer: Recent advances. Front. Pharmacol. 2019, 10, 1336.
- Bektic, J.; Berger, A.P.; Pfeil, K.; Dobler, G.; Bartsch, G.; Klocker, H. Androgen Receptor Regulation by Physiological Concentrations of the Isoflavonoid Genistein in Androgen-Dependent LNCaP Cells Is Mediated by Estrogen Receptor β. Eur. Urol. 2004, 45, 245–251.
- Takahashi, Y.; Hursting, S.D.; Perkins, S.N.; Wang, T.C.; Wang, T.T.Y. Genistein affects androgen-responsive genes through both androgen- and estrogen-induced signaling pathways. Mol. Carcinog. 2006, 45, 18–25.
- Li, Y.; Wang, Z.; Kong, D.; Li, R.; Sarkar, S.H.; Sarkar, F.H. Regulation of Akt/FOXO3a/GSK-3beta/AR signaling network by isoflavone in prostate cancer cells. J. Biol. Chem. 2008, 283, 27707–27716.
- Basak, S.; Pookot, D.; Noonan, E.J.; Dahiya, R. Genistein down-regulates androgen receptor by modulating HDAC6-Hsp90 chaperone function. Mol. Cancer Ther. 2008, 7, 3195–3202.
- Mahmoud, A.M.; Zhu, T.; Parray, A.; Siddique, H.R.; Yang, W.; Saleem, M.; Bosland, M.C. Differential effects of genistein on prostate cancer cells depend on mutational status of the androgen receptor. PLoS ONE 2013, 8, e78479.
- Yu, L.; Blackburn, G.L.; Zhou, J.-R. Genistein and Daidzein Downregulate Prostate Androgen-Regulated Transcript-1 (PART-1) Gene expression induced by dihydrotestosterone in human prostate LNCaP cancer cells. J. Nutr. 2003, 133, 389–392.
- Kim, S.-H.; Singh, S.V. D,L-Sulforaphane causes transcriptional repression of androgen receptor in human prostate cancer cells. Mol. Cancer Ther. 2009, 8, 1946–1954.
- Gibbs, A.; Schwartzman, J.; Deng, V.; Alumkal, J. Sulforaphane destabilizes the androgen receptor in prostate cancer cells by inactivating histone deacetylase 6. Proc. Natl. Acad. Sci. USA 2009, 106, 16663–16668.
- Khurana, N.; Talwar, S.; Chandra, P.K.; Sharma, P.; Abdel-Mageed, A.B.; Mondal, D.; Sikka, S.C. Sulforaphane increases the efficacy of anti-androgens by rapidly decreasing androgen receptor levels in prostate cancer cells. Int. J. Oncol. 2016, 49, 1609–1619.
- Khurana, N.; Kim, H.; Chandra, P.K.; Talwar, S.; Sharma, P.; Abdel-Mageed, A.B.; Sikka, S.C.; Mondal, D. Multimodal actions of the phytochemical sulforaphane suppress both AR and AR-V7 in 22Rv1 cells: Advocating a potent pharmaceutical combination against castration-resistant prostate cancer. Oncol. Rep. 2017, 38, 2774–2786.
- Ren, F.; Zhang, S.; Mitchell, S.H.; Butler, R.; Young, C.Y. Tea polyphenols down-regulate the expression of the androgen receptor in LNCaP prostate cancer cells. Oncogene 2000, 19, 1924–1932.
- Chuu, C.-P.; Chen, R.-Y.; Kokontis, J.M.; Hiipakka, R.A.; Liao, S. Suppression of androgen receptor signaling and prostate specific antigen expression by (-)-epigallocatechin-3-gallate in different progression stages of LNCaP prostate cancer cells. Cancer Lett. 2009, 275, 86–92.
- Bae, J.-S.; Park, H.-S.; Park, J.-W.; Li, S.-H.; Chun, Y.-S. Red ginseng and 20(S)-Rg3 control testosterone-induced prostate hyperplasia by deregulating androgen receptor signaling. J. Nat. Med. 2012, 66, 476–485.
- Nanao-Hamai, M.; Son, B.K.; Komuro, A.; Asari, Y.; Hashizume, T.; Takayama, K.; Ogawa, S.; Akishita, M. Ginsenoside Rb1 inhibits vascular calcification as a selective androgen receptor modulator. Eur. J. Pharmacol. 2019, 859, 172546.
- Cao, B.; Liu, X.; Li, J.; Liu, S.; Qi, Y.; Xiong, Z.; Zhang, A.; Wiese, T.; Fu, X.; Gu, J.; et al. 20(S)-protopanaxadiol-aglycone downregulation of the full-length and splice variants of androgen receptor. Int. J. Cancer 2013, 132, 1277–1287.
- Cao, B.; Qi, Y.; Yang, Y.; Liu, X.; Xu, D.; Guo, W.; Zhan, Y.; Xiong, Z.; Zhang, A.; Wang, A.R.; et al. 20(S)-protopanaxadiol inhibition of progression and growth of castration-resistant prostate cancer. PLoS ONE 2014, 9, e111201.
- Zhu, W. Silymarin inhibits function of the androgen receptor by reducing nuclear localization of the receptor in the human prostate cancer cell line LNCaP. Carcinogenesis 2001, 22, 1399–1403.
- Li, J.; Cao, B.; Liu, X.; Fu, X.; Xiong, Z.; Chen, L.; Sartor, O.; Dong, Y.; Zhang, H. Berberine suppresses androgen receptor signaling in prostate cancer. Mol. Cancer Ther. 2011, 10, 1346–1356.
- Hahm, E.-R.; Karlsson, A.I.; Bonner, M.Y.; Arbiser, J.L.; Singh, S. V Honokiol inhibits androgen receptor activity in prostate cancer cells. Prostate 2014, 74, 408–420.
- Shao, L.; Zhou, Z.; Cai, Y.; Castro, P.; Dakhov, O.; Shi, P.; Bai, Y.; Ji, H.; Shen, W.; Wang, J. Celastrol suppresses tumor cell growth through targeting an AR-ERG-NF-κB pathway in TMPRSS2/ERG fusion gene expressing prostate cancer. PLoS ONE 2013, 8, e58391.
- Normanno, N.; De Luca, A.; Bianco, C.; Strizzi, L.; Mancino, M.; Maiello, M.R.; Carotenuto, A.; De Feo, G.; Caponigro, F.; Salomon, D.S. Epidermal growth factor receptor (EGFR) signaling in cancer. Gene 2006, 366, 2–16.
- Huynh, H.; Nguyen, T.T.T.; Chan, E.; Tran, E. Inhibition of ErbB-2 and ErbB-3 expression by quercetin prevents transforming growth factor alpha (TGF-alpha)- and epidermal growth factor (EGF)-induced human PC-3 prostate cancer cell proliferation. Int. J. Oncol. 2003, 23, 821–829.
- Firdous, A.B.; Sharmila, G.; Balakrishnan, S.; Rajasingh, P.; Suganya, S.; Srinivasan, N.; Arunakaran, J. Quercetin, a natural dietary flavonoid, acts as a chemopreventive agent against prostate cancer in an in vivo model by inhibiting the EGFR signaling pathway. Food Funct. 2014, 5, 2632–2645.
- Markaverich, B.M.; Vijjeswarapu, M.; Shoulars, K.; Rodriguez, M. Luteolin and gefitinib regulation of EGF signaling pathway and cell cycle pathway genes in PC-3 human prostate cancer cells. J. Steroid Biochem. Mol. Biol. 2010, 122, 219–231.
- Stewart, J.R.; O’Brian, C.A. Resveratrol antagonizes EGFR-dependent Erk1/2 activation in human androgen-independent prostate cancer cells with associated isozyme-selective PKC alpha inhibition. Invest. New Drugs 2004, 22, 107–117.
- Oh, H.Y.; Leem, J.; Yoon, S.J.; Yoon, S.; Hong, S.J. Lipid raft cholesterol and genistein inhibit the cell viability of prostate cancer cells via the partial contribution of EGFR-Akt/p70S6k pathway and down-regulation of androgen receptor. Biochem. Biophys. Res. Commun. 2010, 393, 319–324.
- Heidegger, I.; Kern, J.; Ofer, P.; Klocker, H.; Massoner, P. Oncogenic functions of IGF1R and INSR in prostate cancer include enhanced tumor growth, cell migration and angiogenesis. Oncotarget 2014, 5, 2723–2735.
- Wing Ying Cheung, C.; Gibbons, N.; Wayne Johnson, D.; Lawrence Nicol, D. Silibinin – A promising new treatment for cancer. Anticancer. Agents Med. Chem. 2010, 10, 186–195.
- Zhu, X.X.; Ding, Y.H.; Wu, Y.; Qian, L.Y.; Zou, H.; He, Q. Silibinin: A potential old drug for cancer therapy. Expert Rev. Clin. Pharmacol. 2016, 9, 1323–1330.
- Zi, X.; Zhang, J.; Agarwal, R.; Pollak, M. Silibinin up-regulates insulin-like growth factor-binding protein 3 expression and inhibits proliferation of androgen-independent prostate cancer cells. Cancer Res. 2000, 60, 5617–5620.
- Singh, R.P.; Dhanalakshmi, S.; Tyagi, A.K.; Chan, D.C.F.; Agarwal, C.; Agarwal, R. Dietary feeding of silibinin inhibits advance human prostate carcinoma growth in athymic nude mice and increases plasma insulin-like growth factor-binding protein-3 levels. Cancer Res. 2002, 62, 3063–3069.
- Raina, K.; Blouin, M.-J.; Singh, R.P.; Majeed, N.; Deep, G.; Varghese, L.; Glodé, L.M.; Greenberg, N.M.; Hwang, D.; Cohen, P.; et al. Dietary feeding of silibinin inhibits prostate tumor growth and progression in transgenic adenocarcinoma of the mouse prostate model. Cancer Res. 2007, 67, 11083–11091.
- Fang, J.; Zhou, Q.; Shi, X.L.; Jiang, B.H. Luteolin inhibits insulin-like growth factor 1 receptor signaling in prostate cancer cells. Carcinogenesis 2007, 28, 713–723.
- Hsieh, A.; Edlind, M. PI3K-AKT-mTOR signaling in prostate cancer progression and androgen deprivation therapy resistance. Asian J. Androl. 2014, 16, 378.
- Ward, A.B.; Mir, H.; Kapur, N.; Gales, D.N.; Carriere, P.P.; Singh, S. Quercetin inhibits prostate cancer by attenuating cell survival and inhibiting anti-apoptotic pathways. World J. Surg. Oncol. 2018, 16, 108.
- Shukla, S.; Gupta, S. Apigenin-induced cell cycle arrest is mediated by modulation of MAPK, PI3K-Akt, and loss of cyclin D1 associated retinoblastoma dephosphorylation in human prostate cancer cells. Cell Cycle 2007, 6, 1102–1114.
- Shukla, S.; Bhaskaran, N.; Babcook, M.A.; Fu, P.; MacLennan, G.T.; Gupta, S. Apigenin inhibits prostate cancer progression in TRAMP mice via targeting PI3K/Akt/FoxO pathway. Carcinogenesis 2014, 35, 452–460.
- Chaudhary, L.R.; Hruska, K.A. Inhibition of cell survival signal protein kinase B/Akt by curcumin in human prostate cancer cells. J. Cell. Biochem. 2003, 89, 1–5.
- Yu, S.; Shen, G.; Khor, T.O.; Kim, J.-H.; Kong, A.-N.T. Curcumin inhibits Akt/mammalian target of rapamycin signaling through protein phosphatase-dependent mechanism. Mol. Cancer Ther. 2008, 7, 2609–2620.
- Cao, F.; Jin, T.-Y.; Zhou, Y.-F. Inhibitory effect of isoflavones on prostate cancer cells and PTEN gene. Biomed. Environ. Sci. 2006, 19, 35–41.
- El Touny, L.H.; Banerjee, P.P. Akt–GSK-3 pathway as a target in genistein-induced inhibition of TRAMP prostate cancer progression toward a poorly differentiated phenotype. Carcinogenesis 2007, 28, 1710–1717.
- Keum, Y.S.; Oo Khor, T.; Lin, W.; Shen, G.; Han Kwon, K.; Barve, A.; Li, W.; Kong, A.N. Pharmacokinetics and pharmacodynamics of broccoli sprouts on the suppression of prostate cancer in transgenic adenocarcinoma of mouse prostate (TRAMP) Mice: Implication of induction of Nrf2, HO-1 and apoptosis and the suppression of Akt-dependent kinase p. Pharm. Res. 2009, 26, 2324–2331.
- Siddiqui, I.A.; Adhami, V.M.; Afaq, F.; Ahmad, N.; Mukhtar, H. Modulation of phosphatidylinositol-3-kinase/protein kinase B- and mitogen-activated protein kinase-pathways by tea polyphenols in human prostate cancer cells. J. Cell. Biochem. 2004, 91, 232–242.
- Verzella, D.; Fischietti, M.; Capece, D.; Vecchiotti, D.; Del Vecchio, F.; Cicciarelli, G.; Mastroiaco, V.; Tessitore, A.; Alesse, E.; Zazzeroni, F. Targeting the NF-κB pathway in prostate cancer: A promising therapeutic approach? Curr. Drug Targets 2016, 17, 311–320.
- Benitez, D.A.; Hermoso, M.A.; Pozo-Guisado, E.; Fernández-Salguero, P.M.; Castellón, E.A. Regulation of cell survival by resveratrol involves inhibition of NFκB-regulated gene expression in prostate cancer cells. Prostate 2009, 69, 1045–1054.
- Davis, J.N.; Kucuk, O.; Sarkar, F.H. Genistein inhibits NF-kappa B activation in prostate cancer cells. Nutr. Cancer 1999, 35, 167–174.
- Li, Y.; Sarkar, F.H. Inhibition of nuclear factor kappaB activation in PC3 cells by genistein is mediated via Akt signaling pathway. Clin. Cancer Res. 2002, 8, 2369–2377.
- Xu, C.; Shen, G.; Chen, C.; Gélinas, C.; Kong, A.N.T. Suppression of NF-κB and NF-κB-regulated gene expression by sulforaphane and PEITC through IκBα, IKK pathway in human prostate cancer PC-3 cells. Oncogene 2005, 24, 4486–4495.
- Shanmugam, M.K.; Rajendran, P.; Li, F.; Nema, T.; Vali, S.; Abbasi, T.; Kapoor, S.; Sharma, A.; Kumar, A.P.; Ho, P.C.; et al. Ursolic acid inhibits multiple cell survival pathways leading to suppression of growth of prostate cancer xenograft in nude mice. J. Mol. Med. 2011, 89, 713–727.
- Yap, W.N.; Chang, P.N.; Han, H.Y.; Lee, D.T.W.; Ling, M.T.; Wong, Y.C.; Yap, Y.L. γ-Tocotrienol suppresses prostate cancer cell proliferation and invasion through multiple-signalling pathways. Br. J. Cancer 2008, 99, 1832–1841.
- Gonnissen, A.; Isebaert, S.; Haustermans, K. Hedgehog signaling in prostate cancer and its therapeutic implication. Int. J. Mol. Sci. 2013, 14, 13979–14007.
- Slusarz, A.; Shenouda, N.S.; Sakla, M.S.; Drenkhahn, S.K.; Narula, A.S.; MacDonald, R.S.; Besch-Williford, C.L.; Lubahn, D.B. Common botanical compounds inhibit the Hedgehog signaling pathway in prostate cancer. Cancer Res. 2010, 70, 3382–3390.
- Yardy, G.W.; Brewster, S.F. Wnt signalling and prostate cancer. Prostate Cancer Prostatic Dis. 2005, 8, 119–126.
- Murillo-Garzón, V.; Kypta, R. WNT signalling in prostate cancer. Nat. Rev. Urol. 2017, 14, 683–696.
- Baruah, M.M.; Khandwekar, A.P.; Sharma, N. Quercetin modulates Wnt signaling components in prostate cancer cell line by inhibiting cell viability, migration, and metastases. Tumor Biol. 2016, 37, 14025–14034.
- Teiten, M.H.; Gaascht, F.; Cronauer, M.; Henry, E.; Dicato, M.; Diederich, M. Anti-proliferative potential of curcumin in androgen-dependent prostate cancer cells occurs through modulation of the Wingless signaling pathway. Int. J. Oncol. 2011, 38, 603–611.
- Liss, M.A.; Schlicht, M.; Kahler, A.; Fitzgerald, R.; Thomassi, T.; Degueme, A.; Hessner, M.; Datta, M.W. Characterization of soy-based changes in Wnt-frizzled signaling in prostate cancer. Cancer Genomics Proteomics 2010, 7, 245–252.
- Lu, W.; Lin, C.; King, T.D.; Chen, H.; Reynolds, R.C.; Li, Y. Silibinin inhibits Wnt/β-catenin signaling by suppressing Wnt co-receptor LRP6 expression in human prostate and breast cancer cells. Cell. Signal. 2012, 24, 2291–2296.
- Peng, Y.; Croce, C.M. The role of MicroRNAs in human cancer. Signal. Transduct. Target. Ther. 2016, 1, 15004.
- Chen, Y.; Zaman, M.S.; Deng, G.; Majid, S.; Saini, S.; Liu, J.; Tanaka, Y.; Dahiya, R. MicroRNAs 221/222 and genistein-mediated regulation of ARHI tumor suppressor gene in prostate cancer. Cancer Prev. Res. (Phila). 2011, 4, 76–86.
- Rabiau, N.; Trraf, H.-K.; Adjakly, M.; Bosviel, R.; Guy, L.; Fontana, L.; Bignon, Y.-J.; Bernard-Gallon, D.J. miRNAs differentially expressed in prostate cancer cell lines after soy treatment. In Vivo 2011, 25, 917–921.
- Chiyomaru, T.; Yamamura, S.; Zaman, M.S.; Majid, S.; Deng, G.; Shahryari, V.; Saini, S.; Hirata, H.; Ueno, K.; Chang, I.; et al. Genistein suppresses prostate cancer growth through inhibition of oncogenic MicroRNA-151. PLoS ONE 2012, 7, e43812.
- Chiyomaru, T.; Yamamura, S.; Fukuhara, S.; Hidaka, H.; Majid, S.; Saini, S.; Arora, S.; Deng, G.; Shahryari, V.; Chang, I.; et al. Genistein up-regulates tumor suppressor microRNA-574-3p in prostate cancer. PLoS ONE 2013, 8, e58929.
- Chiyomaru, T.; Yamamura, S.; Fukuhara, S.; Yoshino, H.; Kinoshita, T.; Majid, S.; Saini, S.; Chang, I.; Tanaka, Y.; Enokida, H.; et al. Genistein inhibits prostate cancer cell growth by targeting miR-34a and oncogenic HOTAIR. PLoS ONE 2013, 8, e70372.
- Hirata, H.; Hinoda, Y.; Shahryari, V.; Deng, G.; Tanaka, Y.; Tabatabai, Z.L.; Dahiya, R. Genistein downregulates onco-miR-1260b and upregulates sFRP1 and Smad4 via demethylation and histone modification in prostate cancer cells. Br. J. Cancer 2014, 110, 1645–1654.
- Han, K.; Meng, W.; Zhang, J.-J.; Zhou, Y.; Wang, Y.; Su, Y.; Lin, S.; Gan, Z.; Sun, Y.; Min, D.-L. Luteolin inhibited proliferation and induced apoptosis of prostate cancer cells through miR-301. Onco. Targets. Ther. 2016, 26, 3085–3094.
- Zhu, M.; Zheng, Z.; Huang, J.; Ma, X.; Huang, C.; Wu, R.; Li, X.; Liang, Z.; Deng, F.; Wu, J.; et al. Modulation of miR-34a in curcumin-induced antiproliferation of prostate cancer cells. J. Cell. Biochem. 2019, 120, 15616–15624.
- Sheth, S.; Jajoo, S.; Kaur, T.; Mukherjea, D.; Sheehan, K.; Rybak, L.P.; Ramkumar, V. Resveratrol reduces prostate cancer growth and metastasis by inhibiting the Akt/MicroRNA-21 pathway. PLoS ONE 2012, 7, e51655.
- Dhar, S.; Kumar, A.; Rimando, A.M.; Zhang, X.; Levenson, A.S. Resveratrol and pterostilbene epigenetically restore PTEN expression by targeting oncomiRs of the miR-17 family in prostate cancer. Oncotarget 2015, 6, 27214–27226.
- Gao, Q.; Zheng, J. Ginsenoside Rh2 inhibits prostate cancer cell growth through suppression of microRNA-4295 that activates CDKN1A. Cell Prolif. 2018, 51, e12438.
- Cao, L.; Zhang, X.; Cao, F.; Wang, Y.; Shen, Y.; Yang, C.; Uzan, G.; Peng, B.; Zhang, D. Inhibiting inducible miR-223 further reduces viable cells in human cancer cell lines MCF-7 and PC3 treated by celastrol. BMC Cancer 2015, 15, 873.
- Vijayababu, M.R.; Kanagaraj, P.; Arunkumar, A.; Ilangovan, R.; Dharmarajan, A.; Arunakaran, J. Quercetin induces p53-independent apoptosis in human prostate cancer cells by modulating Bcl-2-related proteins: A possible mediation by IGFBP-3. Oncol. Res. 2006, 16, 67–74.
- Senthilkumar, K.; Elumalai, P.; Arunkumar, R.; Banudevi, S.; Gunadharini, N.D.; Sharmila, G.; Selvakumar, K.; Arunakaran, J. Quercetin regulates insulin like growth factor signaling and induces intrinsic and extrinsic pathway mediated apoptosis in androgen independent prostate cancer cells (PC-3). Mol. Cell. Biochem. 2010, 344, 173–184.
- Lee, D.H.; Szczepanski, M.; Lee, Y.J. Role of Bax in quercetin-induced apoptosis in human prostate cancer cells. Biochem. Pharmacol. 2008, 75, 2345–2355.
- Horinaka, M.; Yoshida, T.; Shiraishi, T.; Nakata, S.; Wakada, M.; Nakanishi, R.; Nishino, H.; Matsui, H.; Sakai, T. Luteolin induces apoptosis via death receptor 5 upregulation in human malignant tumor cells. Oncogene 2005, 24, 7180–7189.
- Pham, H.N.T.; Sakoff, J.A.; Van Vuong, Q.; Bowyer, M.C.; Scarlett, C.J. Comparative cytotoxic activity between kaempferol and gallic acid against various cancer cell lines. Data Br. 2018, 21, 1033–1036.
- Dorai, T.; Gehani, N.; Katz, A. Therapeutic potential of curcumin in human prostate cancer - I. Curcumin induces apoptosis in both androgen-dependent and androgen-independent prostate cancer cells. Prostate Cancer Prostatic Dis. 2000, 3, 84–93.
- Shankar, S.; Srivastava, R.K. Involvement of Bcl-2 family members, phosphatidylinositol 3′-kinase/AKT and mitochondrial p53 in curcumin (diferulolylmethane)-induced apoptosis in prostate cancer. Int. J. Oncol. 2007, 30, 905–918.
- Yang, J.; Ning, J.; Peng, L.; He, D. Effect of curcumin on Bcl-2 and Bax expression in nude mice prostate cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 9272–9278.
- Lin, H.Y.; Shih, A.; Davis, F.B.; Tang, H.Y.; Martino, L.J.; Bennett, J.A.; Davis, P.J. Resveratrol induced serine phosphorylation of p53 causes apoptosis in a mutant p53 prostate cancer cell line. J. Urol. 2002, 168, 748–755.
- Morris, G.Z.; Williams, R.L.; Elliott, M.S.; Beebe, S.J. Resveratrol induces apoptosis in LNCaP cells and requires hydroxyl groups to decrease viability in LNCaP and DU 145 cells. Prostate 2002, 52, 319–329.
- Aziz, M.H.; Nihal, M.; Fu, V.X.; Jarrard, D.F.; Ahmad, N. Resveratrol-caused apoptosis of human prostate carcinoma LNCaP cells is mediated via modulation of phosphatidylinositol 3′-kinase/Akt pathway and Bcl-2 family proteins. Mol. Cancer Ther. 2006, 5, 1335–1341.
- Benitez, D.A.; Pozo-Guisado, E.; Alvarez-Barrientos, A.; Fernandez-Salguero, P.M.; Castellon, E.A. Mechanisms involved in resveratrol-induced apoptosis and cell cycle arrest in prostate cancer-derived cell lines. J. Androl. 2006, 28, 282–293.
- Kai, L.; Samuel, S.K.; Levenson, A.S. Resveratrol enhances p53 acetylation and apoptosis in prostate cancer by inhibiting MTA1/NuRD complex. Int. J. cancer 2010, 126, 1538–1548.
- Kumi-Diaka, J.; Sanderson, N.A.; Hall, A. The mediating role of caspase-3 protease in the intracellular mechanism of genistein-induced apoptosis in human prostatic carcinoma cell lines, DU145 and LNCaP. Biol. Cell 2000, 92, 595–604.
- Chiao, J.; Chung, F.-L.; Kancherla, R.; Ahmed, T.; Mittelman, A.; Conaway, C. Sulforaphane and its metabolite mediate growth arrest and apoptosis in human prostate cancer cells. Int. J. Oncol. 2002, 20, 631–636.
- Singh, A.V.; Xiao, D.; Lew, K.L.; Dhir, R.; Singh, S.V. Sulforaphane induces caspase-mediated apoptosis in cultured PC-3 human prostate cancer cells and retards growth PC-3 xenografts in vivo. Carcinogenesis 2004, 25, 83–90.
- Choi, S.; Lew, K.L.; Xiao, H.; Herman-Antosiewicz, A.; Xiao, D.; Brown, C.K.; Singh, S.V. D,L-Sulforaphane-induced cell death in human prostate cancer cells is regulated by inhibitor of apoptosis family proteins and Apaf-1. Carcinogenesis 2007, 28, 151–162.
- Clarke, J.D.; Hsu, A.; Yu, Z.; Dashwood, R.H.; Ho, E. Differential effects of sulforaphane on histone deacetylases, cell cycle arrest and apoptosis in normal prostate cells versus hyperplastic and cancerous prostate cells. Mol. Nutr. Food Res. 2011, 55, 999–1009.
- Hagen, R.M.; Chedea, V.S.; Mintoff, C.P.; Bowler, E.; Morse, H.R.; Ladomery, M.R. Epigallocatechin-3-gallate promotes apoptosis and expression of the caspase 9a splice variant in PC3 prostate cancer cells. Int. J. Oncol. 2013, 43, 194–200.
- Ben-Eltriki, M.; Deb, S.; Adomat, H.; Tomlinson Guns, E.S. Calcitriol and 20(S)-protopanaxadiol synergistically inhibit growth and induce apoptosis in human prostate cancer cells. J. Steroid Biochem. Mol. Biol. 2016, 158, 207–219.
- Agarwal, C.; Tyagi, A.; Kaur, M.; Agarwal, R. Silibinin inhibits constitutive activation of Stat3, and causes caspase activation and apoptotic death of human prostate carcinoma DU145 cells. Carcinogenesis 2007, 28, 1463–1470.
- Mantena, S.K.; Sharma, S.D.; Katiyar, S.K. Berberine, a natural product, induces G1-phase cell cycle arrest and caspase-3-dependent apoptosis in human prostate carcinoma cells. Mol. Cancer Ther. 2006, 5, 296–308.
- Choi, M.S.; Oh, J.H.; Kim, S.M.; Jung, H.Y.; Yoo, H.S.; Lee, Y.M.; Moon, D.C.; Han, S.B.; Hong, J.T. Berberine inhibits p53-dependent cell growth through induction of apoptosis of prostate cancer cells. Int. J. Oncol. 2009, 34, 1221–1230.
- Zhang, Y.; Kong, C.; Wang, H.; Wang, L.; Xu, C.; Sun, Y. Phosphorylation of Bcl-2 and activation of caspase-3 via the c-Jun N-terminal kinase pathway in ursolic acid-induced DU145 cells apoptosis. Biochimie 2009, 91, 1173–1179.
- Zhang, Y.; Kong, C.; Wang, L.; Li, J.; Liu, X.; Xu, B.; Xu, C.; Sun, Y. Ursolic acid overcomes Bcl-2-mediated resistance to apoptosis in prostate cancer cells involving activation of JNK-induced Bcl-2 phosphorylation and degradation. J. Cell. Biochem. 2009, 109, 764–773.
- Zhang, Y.; Kong, C.; Zeng, Y.; Wang, L.; Li, Z.; Wang, H.; Xu, C.; Sun, Y. Ursolic acid induces PC-3 cell apoptosis via activation of JNK and inhibition of Akt pathways in vitro. Mol. Carcinog. 2010, 49, 374–385.
- Hahm, E.R.; Arlotti, J.A.; Marynowski, S.W.; Singh, S.V. Honokiol, a constituent of oriental medicinal herb Magnolia officinalis, inhibits growth of PC-3 xenografts in vivo in association with apoptosis induction. Clin. Cancer Res. 2008, 14, 1248–1257.
- Chen, D. Structure-proteasome-inhibitory activity relationships of dietary flavonoids in human cancer cells. Front. Biosci. 2007, 12, 1935.
- Kazi, A.; Daniel, K.G.; Smith, D.M.; Kumar, N.B.; Dou, Q.P. Inhibition of the proteasome activity, a novel mechanism associated with the tumor cell apoptosis-inducing ability of genistein. Biochem. Pharmacol. 2003, 66, 965–976.
- Dai, Y.; Desano, J.; Tang, W.; Meng, X.; Meng, Y.; Burstein, E.; Lawrence, T.S.; Xu, L. Natural proteasome inhibitor celastrol suppresses androgen-independent prostate cancer progression by modulating apoptotic proteins and NF-kappaB. PLoS ONE 2010, 5, e14153.
- Liu, K.-C.; Yen, C.-Y.; Wu, R.S.-C.; Yang, J.-S.; Lu, H.-F.; Lu, K.-W.; Lo, C.; Chen, H.-Y.; Tang, N.-Y.; Wu, C.-C.; et al. The roles of endoplasmic reticulum stress and mitochondrial apoptotic signaling pathway in quercetin-mediated cell death of human prostate cancer PC-3 cells. Environ. Toxicol. 2014, 29, 428–439.
- Rivera, M.; Ramos, Y.; Rodríguez-Valentín, M.; López-Acevedo, S.; Cubano, L.A.; Zou, J.; Zhang, Q.; Wang, G.; Boukli, N.M. Targeting multiple pro-apoptotic signaling pathways with curcumin in prostate cancer cells. PLoS ONE 2017, 12, e0179587.
- Kim, S.H.; Kim, K.Y.; Yu, S.N.; Seo, Y.K.; Chun, S.S.; Yu, H.S.; Ahn, S.C. Silibinin induces mitochondrial NOX4-mediated endoplasmic reticulum stress response and its subsequent apoptosis. BMC Cancer 2016, 16, 452.
- Nagesh, P.; Hatami, E.; Chowdhury, P.; Kashyap, V.; Khan, S.; Hafeez, B.; Chauhan, S.; Jaggi, M.; Yallapu, M. Tannic acid induces endoplasmic reticulum stress-mediated apoptosis in prostate cancer. Cancers 2018, 10, 68.
- Limonta, P.; Moretti, R.; Marzagalli, M.; Fontana, F.; Raimondi, M.; Montagnani Marelli, M. Role of endoplasmic reticulum stress in the anticancer activity of natural compounds. Int. J. Mol. Sci. 2019, 20, 961.
- Lee, W.-J.; Chien, M.-H.; Chow, J.-M.; Chang, J.-L.; Wen, Y.-C.; Lin, Y.-W.; Cheng, C.-W.; Lai, G.-M.; Hsiao, M.; Lee, L.-M. Nonautophagic cytoplasmic vacuolation death induction in human PC-3M prostate cancer by curcumin through reactive oxygen species -mediated endoplasmic reticulum stress. Sci. Rep. 2015, 5, 10420.
- Kumar, S.; Stokes, J.; Singh, U.P.; Scissum-Gunn, K.; Singh, R.; Manne, U.; Mishra, M.K. Prolonged exposure of resveratrol induces reactive superoxide species–independent apoptosis in murine prostate cells. Tumor Biol. 2017, 39, 101042831771503.
- Wang, D.; Gao, Z.; Zhang, X. Resveratrol induces apoptosis in murine prostate cancer cells via hypoxia-inducible factor 1-alpha (HIF-1α)/reactive oxygen species (ROS)/P53 signaling. Med. Sci. Monit. 2018, 24, 8970–8976.
- Singh, S.V.; Srivastava, S.K.; Choi, S.; Lew, K.L.; Antosiewicz, J.; Xiao, D.; Zeng, Y.; Watkins, S.C.; Johnson, C.S.; Trump, D.L.; et al. Sulforaphane-induced cell death in human prostate cancer cells is initiated by reactive oxygen species. J. Biol. Chem. 2005, 280, 19911–19924.
- Xiao, D.; Powolny, A.A.; Antosiewicz, J.; Hahm, E.R.; Bommareddy, A.; Zeng, Y.; Desai, D.; Amin, S.; Herman-Antosiewicz, A.; Singh, S.V. Cellular responses to cancer chemopreventive agent D,L-sulforaphane in human prostate cancer cells are initiated by mitochondrial reactive oxygen species. Pharm. Res. 2009, 26, 1729–1738.
- Imenshahidi, M.; Hosseinzadeh, H. Berberis vulgaris and berberine: An update review. Phytother. Res. 2016, 30, 1745–1764.
- Zhang, C.; Sheng, J.; Li, G.; Zhao, L.; Wang, Y.; Yang, W.; Yao, X.; Sun, L.; Zhang, Z.; Cui, R. Effects of berberine and its derivatives on cancer: A systems pharmacology review. Front. Pharmacol. 2019, 10, 1461.
- Zhang, L.Y.; Wu, Y.L.; Gao, X.H.; Guo, F. Mitochondrial protein cyclophilin-D-mediated programmed necrosis attributes to berberine-induced cytotoxicity in cultured prostate cancer cells. Biochem. Biophys. Res. Commun. 2014, 450, 697–703.
- Kang, D.; Park, W.; Lee, S.; Kim, J.H.; Song, J.J. Crosstalk from survival to necrotic death coexists in DU-145 cells by curcumin treatment. Cell. Signal. 2013, 25, 1288–1300.
- Lee, D.; Kim, I.Y.; Saha, S.; Choi, K.S. Paraptosis in the anti-cancer arsenal of natural products. Pharmacol. Ther. 2016, 162, 120–133.
- Fontana, F.; Raimondi, M.; Marzagalli, M.; Di Domizio, A.; Limonta, P. The emerging role of paraptosis in tumor cell biology: Perspectives for cancer prevention and therapy with natural compounds. Biochim. Biophys. Acta Rev. Cancer. 2020, 1873, 188338.
- Montagnani Marelli, M.; Marzagalli, M.; Fontana, F.; Raimondi, M.; Moretti, R.M.; Limonta, P. Anticancer properties of tocotrienols: A review of cellular mechanisms and molecular targets. J. Cell. Physiol. 2019, 234, 1147–1164.
- Fontana, F.; Raimondi, M.; Marzagalli, M.; Moretti, R.M.; Marelli, M.M.; Limonta, P. Tocotrienols and cancer: From the state of the art to promising novel patents. Recent Pat. Anticancer. Drug Discov. 2019, 14, 5–18.
- Fontana, F.; Moretti, R.M.; Raimondi, M.; Marzagalli, M.; Beretta, G.; Procacci, P.; Sartori, P.; Montagnani Marelli, M.; Limonta, P. δ-Tocotrienol induces apoptosis, involving endoplasmic reticulum stress and autophagy, and paraptosis in prostate cancer cells. Cell Prolif. 2019, 52, e12576.
- Wang, W.B.; Feng, L.X.; Yue, Q.X.; Wu, W.Y.; Guan, S.H.; Jiang, B.H.; Yang, M.; Liu, X.; Guo, D.A. Paraptosis accompanied by autophagy and apoptosis was induced by celastrol, a natural compound with influence on proteasome, ER stress and Hsp90. J. Cell. Physiol. 2012, 227, 2196–2206.
- Glick, D.; Barth, S.; Macleod, K.F. Autophagy: Cellular and molecular mechanisms. J. Pathol. 2010, 221, 3–12.
- Yang, C.; Ma, X.; Wang, Z.; Zeng, X.; Hu, Z.; Ye, Z.; Shen, G. Curcumin induces apoptosis and protective autophagy in castration-resistant prostate cancer cells through iron chelation. Drug Des. Devel. Ther. 2017, 11, 431–439.
- Herman-Antosiewicz, A.; Johnson, D.E.; Singh, S.V. Sulforaphane causes autophagy to inhibit release of cytochrome c and apoptosis in human prostate cancer cells. Cancer Res. 2006, 66, 5828–5835.
- Watson, G.W.; Wickramasekara, S.; Fang, Y.; Palomera-Sanchez, Z.; Maier, C.S.; Williams, D.E.; Dashwood, R.H.; Perez, V.I.; Ho, E. Analysis of autophagic flux in response to sulforaphane in metastatic prostate cancer cells. Mol. Nutr. Food Res. 2015, 59, 1954–1961.
- Kim, S.-H.; Kim, K.-Y.; Yu, S.-N.; Park, S.-K.; Choi, H.-D.; Ji, J.-H.; Ahn, S.-C. Autophagy inhibition enhances silibinin-induced apoptosis by regulating reactive oxygen species production in human prostate cancer PC-3 cells. Biochem. Biophys. Res. Commun. 2015, 468, 151–156.
- Shin, S.W.; Kim, S.Y.; Park, J.-W. Autophagy inhibition enhances ursolic acid-induced apoptosis in PC3 cells. Biochim. Biophys. Acta Mol. Cell Res. 2012, 1823, 451–457.
- Delmulle, L.; Vanden Berghe, T.; De Keukeleire, D.; Vandenabeele, P. Treatment of PC-3 and DU145 prostate cancer cells by prenylflavonoids from hop (Humulus lupulus L.) induces a caspase-independent form of cell death. Phyther. Res. 2008, 22, 197–203.
- Hahm, E.R.; Sakao, K.; Singh, S.V. Honokiol activates reactive oxygen species-mediated cytoprotective autophagy in human prostate cancer cells. Prostate 2014, 74, 1209–1221.
- Suh, Y.; Afaq, F.; Khan, N.; Johnson, J.J.; Khusro, F.H.; Mukhtar, H. Fisetin induces autophagic cell death through suppression of mTOR signaling pathway in prostate cancer cells. Carcinogenesis 2010, 31, 1424–1433.
- Selvaraj, S.; Sun, Y.; Sukumaran, P.; Singh, B.B. Resveratrol activates autophagic cell death in prostate cancer cells via downregulation of STIM1 and the mTOR pathway. Mol. Carcinog. 2016, 55, 818–831.
- Guo, J.; Huang, X.; Wang, H.; Yang, H. Celastrol induces autophagy by targeting AR/miR-101 in prostate cancer cells. PLoS ONE 2015, 10, e0140745.
- Kashyap, D.; Sharma, A.; Tuli, H.S.; Sak, K.; Mukherjee, T.; Bishayee, A. Molecular targets of celastrol in cancer: Recent trends and advancements. Crit. Rev. Oncol. Hematol. 2018, 128, 70–81.
More
Information
Subjects:
Medicine, General & Internal
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.2K
Revisions:
2 times
(View History)
Update Date:
04 Jun 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




