Pancreatic cancer is one of the most aggressive malignant neoplastic diseases. The incidence and mortality rates of this disease vary depending on geographical area, which might be explained by the different exposure to risk factors. Currently, the risk factors for pancreatic cancer fall into two broad categories, namely extrinsic and intrinsic factors. Extrinsic factors include alcohol consumption, smoking, a diet rich in saturated fats, and viral infections such as chronic infection with hepatitis B and C viruses. The pathophysiological mechanisms explaining how these hepatotropic viruses contribute to the development of pancreatic cancer are not fully elucidated. The common origin of hepatocytes and pancreatic cells in the multipotent endodermal cells, the common origin of the blood vessels and biliary ducts of the pancreas and the liver, or chronic inflammatory changes may be involved in this interaction.
1. Introduction
Pancreatic cancer is one of the most aggressive malignant neoplasms, with a 5-year survival rate of about 10% in the United States of America (USA)
[1]. The negative prognosis is due to the insidious growth and non-specific symptoms up to its advanced stages, and also to the absence of sensitive and specific methods for an early diagnosis. Approximately 80–85% of pancreatic cancer cases are diagnosed in stage IV, when the patients can no longer benefit from curative surgery
[1]. In a small proportion of individuals, pancreatic cancer is diagnosed in a localized stage, when surgical treatment is possible and recommended. In this situation, the 5-year survival rate can reach up to 20%
[1].
Huang et al. reported higher incidence and mortality rates of pancreatic cancer in high-income countries
[2]. This suggests the possible correlation between pancreatic cancer and lifestyle factors
[3]. This malignancy is associated with several risk factors that fall into two broad categories, namely intrinsic and extrinsic factors (
Table 1). Extrinsic risk factors are modifiable. The higher incidence of this malignancy in developed regions can also be explained by the increasing prevalence in such areas of modifiable risk factors, such as cigarette smoking, alcohol intake, and obesity
[4].
Table 1. Risk factors for pancreatic cancer
[1][5].
| Intrinsic Risk Factors |
Extrinsic Risk Factors |
| Hereditary |
Diet |
| AB0 blood group |
Obesity |
| Chronic pancreatitis |
Tobacco |
| Cystic fibrosis |
Coffee and alcohol consumption |
| Pancreatic cysts |
Helicobacter pylori infection |
| Diabetes mellitus and insulin resistance |
Infection with hepatitis B virus (HBV) and hepatitis C virus (HCV) |
About 10% of pancreatic cancer patients have a genetic susceptibility
[6]. To date, scientists have identified several genes related to the development of this malignancy, namely:
Regarding the hereditary risk of developing pancreatic cancer, two main categories were defined:
-
Patients with genetic syndromes at risk of developing malignancies, including pancreatic cancer (e.g., Li-Fraumeni syndrome, ataxia-telangiectasia syndrome, Peutz-Jeghers syndrome, Lynch II syndrome, etc.);
-
Patients at risk of familial pancreatic cancer, without a specific molecular basis
[9].
In addition, the existing data in the literature suggest the possible presence of germline mutations in the genes involved in the onset of this malignancy, even in the absence of a family history of pancreatic cancer
[10].
Some studies identified an association between pancreatic cancer and AB0 blood type. The blood group is determined by the presence or absence of some antigens on the surface of erythrocytes. These antigens are glycoproteins that can also be expressed on the surface of other cell types, including pancreatic cells.
Chronic pancreatitis is characterized by a chronic inflammation of the pancreas, which can progress to pancreatic cancer
[11][12]. Thus, among patients with chronic pancreatitis, a cumulative risk of progression to pancreatic cancer of 1.8% at 10 years and 4% at 20 years was reported, regardless of the type of pancreatitis
[13]. There are also reports of the involvement of the cationic trypsinogen gene (PRSS1) in the etiopathogenesis of chronic pancreatitis and pancreatic cancer
[14]. Somatic mutations of PRSS1 have been shown to play important roles in carcinogenesis
[14].
The association of cystic fibrosis with some digestive cancers, including pancreatic cancer, has been demonstrated
[15]. Cystic fibrosis is the most common autosomal recessive disease in Europe. It appears as a consequence of biallelic inactivating germline mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene.
Other conditions strongly correlated with the risk of developing pancreatic cancer are pancreatic cysts, the most common types being intraductal papillary mucinous neoplasms (IPMN). Therapeutic management usually consists of carefully monitoring these patients for the early identification of possible malignant degeneration. In a surveillance strategy for IPMN, the appearance of pancreatic ductal adenocarcinoma was reported in 2–9% of patients, independent of the evolution of IPMN. These results suggest the existence of genetic defects in the pancreatic tissue
[16].
The relationship between pancreatic cancer and diabetes mellitus is bidirectional. Thus, approximately 1% of patients over the age of 50 years, newly diagnosed with metabolic disorder, associate pancreatic cancer as a trigger for their diabetes
[17].
2. Viral Hepatitis: Virology and Epidemiology
Viral hepatitis is a worldwide public health problem because of the large number of affected individuals and the morbidity and mortality rates associated with these infectious disorders. Among viruses responsible for hepatitis, the most important are the hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis D (delta) virus (HDV), and hepatitis E virus (HEV)
[18]. Of these, the only one that does not lead to chronic hepatitis is HAV, while HBV, HCV, HDV, and occasionally HEV may be responsible for long-term forms of viral liver infection
[18].
HBV is a DNA virus, belonging to the
Orthohepadnavirus genus, and is classified into 10 genotypes, A–J
[19]. This virus can be transmitted sexually, by blood, and vertically, from the mother to the fetus
[19]. HBV genotypes have several peculiarities in terms of geographical distribution, route of transmission, and organ damage
[20].
3. Hepatotropic Viruses and Pancreatic Cancer-Pathophysiological Links
HBV and HCV are hepatotropic viruses with oncogenic properties. These viruses can induce persistent liver injury, with subsequent progression to cirrhosis and hepatocellular carcinoma
[21][22]. There are also data suggesting the involvement of these viruses in the development of other neoplasms, such as pancreatic cancer, intrahepatic and extrahepatic duct bile carcinoma, gastric cancer, oesophageal cancer, certain forms of non-Hodgkin’s lymphoma, and leukemia
[23][24][25][26].
Anatomically, the pancreas is situated in the proximity of the liver. The common origin of the blood vessels and bile ducts of these organs makes possible the microorganisms’ migration
[27]. Antigens and replicative sequences of these two viruses have also been identified in extrahepatic tissues (e.g., the pancreas, the kidneys, and the skin)
[28][29].
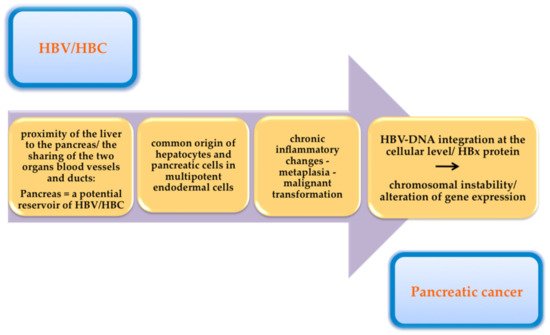
Figure 1 summarizes the pathophysiological mechanisms by which hepatotropic viruses may contribute to the development of pancreatic cancer.
Figure 1. The pathophysiological mechanisms by which hepatotropic viruses may contribute to the development of pancreatic cancer.
4. Conclusions
Pancreatic cancer is a disorder with a poor prognosis mainly because of its late diagnosis. The symptomatology remains nonspecific until its advanced stages, and the retroperitoneal location of the pancreas makes imaging diagnosis more difficult. To improve the prognosis of patients with pancreatic cancer, different approaches are needed for an earlier diagnosis. Viral infections with HBV and HCV are listed among the risk factors involved in the development of pancreatic cancer. The pathophysiological mechanisms by which these hepatotropic viruses contribute to the development of pancreatic cancer are not fully elucidated. Among the possible mechanisms are the anatomical proximity of the two organs, the common origin of the blood vessels and bile ducts of these organs, and the possibility of microorganism migration, the common origin of hepatocytes, and pancreatic cells in multipotent endodermal cells, with the risk of transformation when cultured under specific conditions (the pancreas can be a reservoir for HBV/HCV), and chronic inflammatory changes, with a possible progression to metaplasia and subsequently to malignant transformation, HBV-DNA integration at the cellular level with chromosomal instability, and alteration of gene expression. Future studies are needed to evaluate this relationship and to clarify the pathophysiological mechanisms. Also, there is a need for prospective studies to evaluate the most appropriate surveillance strategy for patients with chronic viral hepatitis regarding the risk of pancreatic cancer, in terms of performance and cost-efficiency. The virus clearance by antiviral treatment may have a role in decreasing the risk of pancreatic cancer.