
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Hidetaka Hamasaki | + 1574 word(s) | 1574 | 2021-11-01 04:08:48 | | | |
| 2 | Beatrix Zheng | + 396 word(s) | 1970 | 2021-11-05 11:58:50 | | |
Video Upload Options
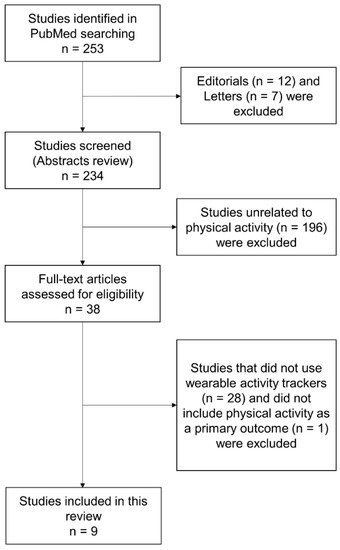
Wearable activity trackers are devices that are comfortably worn on the body and are designed to be effective in monitoring daily physical activity and improving physical fitness of the wearer. This review aimed to investigate the impact of the coronavirus disease 2019 (COVID-19) pandemic on physical activity measured using wearable activity trackers and discuss future perspectives on wearable activity trackers during pandemics. Daily physical activity was significantly decreased during the COVID-19 pandemic.
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has emerged and become prolonged, significantly affecting the lives of people worldwide. To date (September 2021), over 220,000,000 coronavirus cases and 4,500,000 deaths due to COVID-19 have been confirmed across the globe [1]. New coronavirus variants have been appearing one after another, and some mutated strains, such as the Delta variant, may be more contagious, virulent, and vaccine-resistant, which will make it difficult for humans to manage the pandemic effectively [2]. Several countries took non-pharmaceutical public health measures such as lockdown [3] and social distancing [4] in addition to conventional infection control measures (e.g., handwashing and wearing of face masks); however, the spread of COVID-19 is not currently controlled. People are required to make behavioral and lifestyle changes in this pandemic era. The development of technologies and systems that enable disease prevention, effective healthcare without a risk of infection, and protection of human life is critical [5].
Wearable devices that can comfortably be worn on the body and perform several tasks in conjunction with handheld devices, such as smartphones, play a pivotal role in healthcare [6]. Recent systematic reviews have shown that wearable devices are useful for monitoring heart rate and sleep in hospital settings [7], increasing physical activity in children and adolescents [8], improving health-related outcomes in patients with cancer [9], and reducing body weight in individuals with obesity [10]. In addition, during the COVID-19 pandemic, sleep pattern and duration were accurately and effectively monitored by wearable devices [11][12][13][14][15]. On the other hand, social distancing or self-isolation can decrease daily physical activity [16], and such physical inactivity may increase cardiovascular risks [17]; further, physical inactivity itself was associated with an increased risk of hospitalization due to COVID-19 (relative risk = 1.32; 95% confidence interval [CI], 1.10–1.58) [18]. Physical inactivity is a global health problem responsible for the increasing risk of noncommunicable diseases, such as diabetes, coronary heart disease, and breast and colon cancers, and Lee et al. [19] reported that the life expectancy of humans would increase by 0.68 years by increasing physical activity. Promoting and increasing physical activity are the cornerstone of the management of diabetes and obesity, which are now the risks of severe COVID-19 as well as public health epidemics.
2. Physical Activity during the COVID-19 Pandemic
| Authors, Year | Subjects Countries |
Study Design Study Period |
Wearable Activity Trackers | Results |
|---|---|---|---|---|
| Sun et al., 2020 [20] | 1062 patients with major depressive disorder or multiple sclerosis in Italy, Spain, Denmark, the United Kingdom, and Netherlands Age: No description BMI: No description |
Prospective cohort study a part of the RADAR-CNS studies Between 1 February 2019 and 5 July 2020 |
Smartphone Fitbit |
Daily step count↓ in young subjects Heart rate↓ Time spent on social media↑ Sleep duration↑ |
| Kańtoch E and Kańtoch A, 2021 [22] | 5 adult volunteers (2 men and 3 women, 2 subjects with history of cardiovascular diseases) Poland Age: 57 ± 22.38 years BMI: 27.80 ± 2.95 kg/m2 |
Retrospective observational study Between 22 January 2019 and 30 April 2020 |
Fitbit Versa smartwatch | Daily step count↓ Resting heart rate↓ Sleep duration→ |
| Mishra et al., 2021 [24] | 10 community-dwelling older adults (6 men and 4 women) United States Age: 77.3 ± 1.9 years BMI: 27.5 ± 1.6 kg/m2 |
Prospective observational study Between January-March 2020 and March–September 2020 |
ActivePERS/PAMSys pendant | Daily step count↓ Standing%↓ Walking%↓ Sitting%↑ Sleep quality→ |
| Woodruff et al., 2021 [25] | 121 subjects (23 men, 96 women, 1 cisgender, and 1 unknown) Canada Age: 36.2 ± 13.12 years BMI: No description |
Prospective observational study Between March 2020 and April 2020 |
Various activity trackers, e.g., Apple Watch, Fitbit, Samsung, and Garmin | Daily step count↓ Sedentary time↑ |
| Ong et al., 2021 [26] | 1824 city-dwelling, working adults (883 men and 941 women) Singapore Age: 30.94 ± 4.62 years BMI: No description |
Prospective cohort study Between 2 January 2020 and 27 April 2020 |
Fitbit | Daily step count↓ Time spent on moderate-to-vigorous activity↓ Resting heart rate↓ Sleep duration↑ Sleep efficiency→ |
| Pépin et al., 2020 [27] | Approximately 742,000 individuals using wearable activity trackers (proportion of women: 37.8%) Australia, Canada, China, France, Germany, Ireland, Italy, Japan, Netherlands, Singapore, Switzerland, United Kingdom, and United States Age: 35–46 years BMI: No description |
Retrospective observational study Between 1 December 2019 and 13 April 2020 |
Withings | The number of steps↓ in countries with lockdown The number of steps↑ in Sweden without lockdown |
| Capodilupo and Miller, 2021 [28] | 5436 individuals using a wearable activity tracker (3900 men and 1536 women) United States Age: 40.25 ± 11.33 years BMI: No description |
Retrospective observational study Between 1 January 2020 and 15 May 2020 |
WHOOP strap | Exercise frequency↑ in all subjects Exercise frequency↓ in subjects aged 18–25 years Resting heart rate↓ Heart rate variability↑ Sleep duration↑ |
| Zinner et al., 2020 [29] | 14 highly trained athletes (6 men and 8 women) Germany Age: 17.1 ± 1.9 years BMI: 22.9 ± 1.4 kg/m2 |
Retrospective observational study During 4 weeks prior to and after the social distancing and lockdown on 23 March 2020 |
Polar M430 | Training time↓ Time spent on light- and moderate-intensity physical activity↓ Sitting time↓ Time spent lying down↑ |
| Taylor et al., 2021 [23] | 311 patients with heart failure (240 men and 71 women) United Kingdom Age: 68.8 years BMI: <18.5 kg/m2 (0.7%), 18.5–24.9 kg/m2 (22.3%), 25–29.9 kg/m2 (32.8%), >30 (44.3%) |
Prospective observational study During 4 weeks preceding and following the lockdown on 23 March 2020 |
Triage HF | Daily physical activity↓ |
3. Conclusions
In conclusion, daily physical activity was significantly decreased during the current COVID-19 pandemic. It depends on the types of non-pharmacological public health measure; however, the reduction in daily physical activity reaches approximately 10–50% of the amount of daily physical activity before the pandemic. After the current pandemic, the world may confront a significant increase in the number of individuals with metabolic disturbances, such as obesity and diabetes. It should be considered that healthcare professionals encourage people to increase (or at least maintain) daily physical activity via wearable technologies such as smartphone applications. If we construct an effective healthcare system involving wearable activity trackers, we will be able to prevent health problems due to physical inactivity and hospitals’ burden during pandemics in the future.
References
- Coronavirus Cases–Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 1 September 2021).
- Soh, S.M.; Kim, Y.; Kim, C.; Jang, U.S.; Lee, H.R. The rapid adaptation of SARS-CoV-2-rise of the variants: Transmission and resistance. J. Microbiol. 2021, 59, 807–818.
- Alfano, V.; Ercolano, S. The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Appl. Health Econ. Health Policy 2020, 18, 509–517.
- Thu, T.; Ngoc, P.; Hai, N.M.; Tuan, L.A. Effect of the social distancing measures on the spread of COVID-19 in 10 highly infected countries. Sci. Total Environ. 2020, 742, 140430.
- Ding, X.; Clifton, D.; Ji, N.; Lovell, N.H.; Bonato, P.; Chen, W.; Yu, X.; Xue, Z.; Xiang, T.; Long, X.; et al. Wearable Sensing and Telehealth Technology with Potential Applications in the Coronavirus Pandemic. IEEE Rev. Biomed. Eng. 2021, 14, 48–70.
- Hamasaki, H. Efficacy of wearable devices to measure and promote physical activity in the management of diabetes. Eur. Med. J. Diabetes 2018, 6, 62–69.
- Patel, V.; Orchanian-Cheff, A.; Wu, R. Evaluating the Validity and Utility of Wearable Technology for Continuously Monitoring Patients in a Hospital Setting: Systematic Review. JMIR Mhealth Uhealth 2021, 9, e17411.
- Creaser, A.V.; Clemes, S.A.; Costa, S.; Hall, J.; Ridgers, N.D.; Barber, S.E.; Bingham, D.D. The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6211.
- Singh, B.; Zopf, E.M.; Howden, E.J. Effect and feasibility of wearable physical activity trackers and pedometers for increasing physical activity and improving health outcomes in cancer survivors: A systematic review and meta-analysis. J. Sport Health Sci. 2021.
- McDonough, D.J.; Su, X.; Gao, Z. Health wearable devices for weight and BMI reduction in individuals with overweight/obesity and chronic comorbidities: Systematic review and network meta-analysis. Br. J. Sports Med. 2021, 55, 917–925.
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074.
- Blume, C.; Schmidt, M.H.; Cajochen, C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020, 30, R795–R797.
- Wright, K.P., Jr.; Linton, S.K.; Withrow, D.; Casiraghi, L.; Lanza, S.M.; Iglesia, H.; Vetter, C.; Depner, C.M. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr. Biol. 2020, 30, R797–R798.
- Gao, C.; Scullin, M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020, 73, 1–10.
- Lee, P.H.; Marek, J.; Nálevka, P. Crowdsourced smartphone data reveal altered sleep/wake pattern in quarantined Chinese during the COVID-19 outbreak. Chronobiol. Int. 2020, 37, 1181–1190.
- Caputo, E.L.; Reichert, F.F. Studies of Physical Activity and COVID-19 during the Pandemic: A Scoping Review. J. Phys. Act. Health 2020, 17, 1275–1284.
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2020, 318, H1441–H1446.
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 2020, 87, 184–187.
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229.
- Sun, S.; Folarin, A.A.; Ranjan, Y.; Rashid, Z.; Conde, P.; Stewart, C.; Cummins, N.; Matcham, F.; Dalla Costa, G.; Simblett, S.; et al. RADAR-CNS Consortium. Using Smartphones and Wearable Devices to Monitor Behavioral Changes During COVID-19. J. Med. Internet Res. 2020, 22, e19992.
- Raeisi, T.; Mozaffari, H.; Sepehri, N.; Darand, M.; Razi, B.; Garousi, N.; Alizadeh, M.; Alizadeh, S. The negative impact of obesity on the occurrence and prognosis of the 2019 novel coronavirus (COVID-19) disease: A systematic review and meta-analysis. Eat Weight Disord. 2021, 1–19.
- Kańtoch, E.; Kańtoch, A. Cardiovascular and Pre-Frailty Risk Assessment during Shelter-In-Place Measures Based on Multimodal Biomarkers Collected from Smart Telemedical Wearables. J. Clin. Med. 2021, 10, 1997.
- Taylor, J.K.; Ndiaye, H.; Daniels, M.; Ahmed, F.; Triage-HF Plus investigators. Lockdown, slow down: Impact of the COVID-19 pandemic on physical activity-an observational study. Open Heart 2021, 8, e001600.
- Mishra, R.; Park, C.; York, M.K.; Kunik, M.E.; Wung, S.F.; Naik, A.D.; Najafi, B. Decrease in Mobility during the COVID-19 Pandemic and Its Association with Increase in Depression among Older Adults: A Longitudinal Remote Mobility Monitoring Using a Wearable Sensor. Sensors 2021, 21, 3090.
- Woodruff, S.J.; Coyne, P.; St-Pierre, E. Stress, physical activity, and screen-related sedentary behaviour within the first month of the COVID-19 pandemic. Appl. Psychol. Health Well Being 2021, 13, 454–468.
- Ong, J.L.; Lau, T.; Massar, S.; Chong, Z.T.; Ng, B.; Koek, D.; Zhao, W.; Yeo, B.; Cheong, K.; Chee, M. COVID-19-related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep 2021, 44, zsaa179.
- Pépin, J.L.; Bruno, R.M.; Yang, R.Y.; Vercamer, V.; Jouhaud, P.; Escourrou, P.; Boutouyrie, P. Wearable Activity Trackers for Monitoring Adherence to Home Confinement During the COVID-19 Pandemic Worldwide: Data Aggregation and Analysis. J. Med. Internet Res. 2020, 22, e19787.
- Capodilupo, E.R.; Miller, D.J. Changes in health promoting behavior during COVID-19 physical distancing: Utilizing wearable technology to examine trends in sleep, activity, and cardiovascular indicators of health. PLoS ONE 2021, 16, e0256063.
- Zinner, C.; Matzka, M.; Leppich, R.; Kounev, S.; Holmberg, H.C.; Sperlich, B. The Impact of the German Strategy for Containment of Coronavirus SARS-CoV-2 on Training Characteristics, Physical Activity and Sleep of Highly Trained Kayakers and Canoeists: A Retrospective Observational Study. Front. Sports Act. Living 2020, 2, 579830.
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159.
- Henriksen, A.; Johannessen, E.; Hartvigsen, G.; Grimsgaard, S.; Hopstock, L.A. Consumer-Based Activity Trackers as a Tool for Physical Activity Monitoring in Epidemiological Studies During the COVID-19 Pandemic: Development and Usability Study. JMIR Public Health Surveill. 2021, 7, e23806.




