Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Simon Rauch | + 2204 word(s) | 2204 | 2021-10-09 04:13:13 | | | |
| 2 | Rita Xu | -16 word(s) | 2188 | 2021-10-13 05:58:55 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Rauch, S. On-Site Medical Management of Avalanche Victims. Encyclopedia. Available online: https://encyclopedia.pub/entry/14977 (accessed on 07 February 2026).
Rauch S. On-Site Medical Management of Avalanche Victims. Encyclopedia. Available at: https://encyclopedia.pub/entry/14977. Accessed February 07, 2026.
Rauch, Simon. "On-Site Medical Management of Avalanche Victims" Encyclopedia, https://encyclopedia.pub/entry/14977 (accessed February 07, 2026).
Rauch, S. (2021, October 12). On-Site Medical Management of Avalanche Victims. In Encyclopedia. https://encyclopedia.pub/entry/14977
Rauch, Simon. "On-Site Medical Management of Avalanche Victims." Encyclopedia. Web. 12 October, 2021.
Copy Citation
Avalanche accidents are common in mountain regions and approximately 100 fatalities are counted in Europe each year. The average mortality rate is about 25% and survival chances are mainly determined by the degree and duration of avalanche burial, the patency of the airway, the presence of an air pocket, snow characteristics, and the severity of traumatic injuries. The most common cause of death in completely buried avalanche victims is asphyxia followed by trauma. Hypothermia accounts for a minority of deaths; however, hypothermic cardiac arrest has a favorable prognosis and prolonged resuscitation and extracorporeal rewarming are indicated.
avalanche
avalanche burial
cardiac arrest
emergency medicine
hypothermia
1. Introduction and Epidemiology
Snow avalanches are common events in mountainous regions worldwide. About 100 avalanche fatalities are counted per year in Europe [1], while avalanches inflict even higher death tolls in developing countries (e.g., 284 fatalities in South East Anatolia, Turkey in 1992; 135 in Kashmir, Pakistan in 2012) [2], but comprehensive data are missing. Most avalanche accidents occur during recreational activities in the mountains in uncontrolled terrain, while occupational-related avalanche accidents are much less frequent [1][3]. The number of avalanche accidents involving winter recreationists has increased in recent decades due to the increasing popularity of winter outdoor activities [4]. However, in contrast to this development, the number of fatalities has remained relatively stable since the 1980s [1]. In Tyrol, Austria, two-thirds of avalanche accidents occurred on days with hazard grades 2 (triggering of an avalanche is possible with high additional loads) and 3 (triggering is possible even with low additional loads) on slope angles of 35–40 [5]. Most avalanches were triggered in open areas without trees above 2500 m, although >15% occurred below timberline. The highest incidence of avalanche accidents was between 10 a.m. and 3 p.m. [5].
The ongoing climate change may influence the frequency and change the types of snow avalanches, affecting the grade of avalanche burial, pattern of injuries, and survival rates [6]. A wetter and warmer snow climate might lead to higher snow densities and this will likely interfere with the respiration of completely buried victims and increase the rate of asphyxia [7]. Moreover, blunt trauma and secondary injuries will likely become more frequent as terrain roughness is expected to rise and snow cover to become thinner [6].
2. Pathophysiology
Avalanche accidents have an average mortality rate of 25% [8]. Survival chances are largely determined by the degree and duration of avalanche burial, the patency of the airway, the presence of an air pocket, snow characteristics, and the severity of traumatic injuries.
The chance of survival after complete burial (head and chest below the snow) for an uninjured victim is about 50%. If only partially buried (head and chest out of the snow), chance of survival is >95% [8][9][10].
In case of complete burial, the chance of survival is highly time-dependent (Figure 1) [11][12]. The survival rate is around 90% if the victim is rescued within the first 15–20 min (‘survival phase’). Thereafter, survival probability drops sharply to about 30% (~35 min after burial). The main cause of death in this second phase is asphyxia (‘asphyxia phase’); asphyxia causes about 75% of overall avalanche deaths. Asphyxiation during avalanche burial mainly occurs due to airway obstruction with snow, ice mask formation, impaired chest expansion and ventilation because of the weight and compaction of snow, and oxygen deprivation due to rebreathing of expired air. The onset of asphyxia depends also on snow characteristics [7]. From 35 to 90 min, the avalanche survival curve flattens (‘latent phase’). In this phase, survival is possible only if the airway is patent, and it is favored by the presence of an air pocket or mid-low snow density [12][13]. The combination of severe hypothermia, hypoxia, and hypercapnia (triple H syndrome) [14] is the usual cause of death in uninjured victims during the latent and the long-term survival phase (>90 min) [14][15][16]. Rebreathing expired air during avalanche burial results in a progressive decrease in the fraction of inspired oxygen and an increase in the fraction of inspired carbon dioxide, leading to hypoxia and hypercapnia, respectively [17][18]. Accidental hypothermia is the main cause of death in only about 1% of completely buried avalanche victims, but it should be suspected in survivors who do not die of asphyxia within 35 min, especially in victims buried for >60 min [19][20][21]. With cooling, there is a decrease in oxygen consumption of ~6% for every 1 °C reduction in core temperature [22]. A mean core cooling rate of 3 °C/h has been calculated for the entire time between avalanche burial and hospital admission [23], yet, the individual cooling rates during snow burial vary widely, from 0.1 °C/h to 9 °C/h [24][25]. It generally takes at least 60 min after avalanche burial to reach a core temperature <30 °C [20].
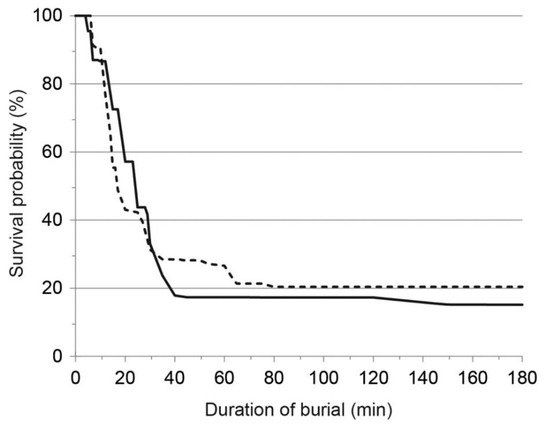
Figure 1. Survival curve for Austria (solid line) and Switzerland (dashed line) for completely buried victims between 2005 and 2013. Reprinted with permission from [12].
Trauma accounts for less than 25% of avalanche deaths in North America and Europe [10]. Traumatic deaths are associated with a wide range of injuries that depend on topographic differences in terrain and snow characteristics [6]. Avalanche victims can sustain virtually any type of injury during the often turbulent descent in an avalanche; severe injuries are frequently caused by collisions with trees or rocks [26].
3. On-Site Management
3.1. Guidelines for On-Site Management
The first algorithm for on-site triage of avalanche victims with asystole was published in 1996 [27]. Recommendations for on-site care of avalanche victims were adopted by the International Commission for Mountain Emergency Medicine (ICAR MedCom) in 2002 [28] and updated in 2013 [2]. In 2010, guidelines were approved by the International Liaison Committee for Resuscitation (ILCOR) and incorporated into the European Resuscitation Council (ERC) and American Heart Association (AHA) guidelines [29][30]. In 2015, the ERC dedicated a section of the resuscitation guidelines in special circumstances to mountain emergency medicine and avalanche rescue [31]. The Wilderness Medical Society (WMS) published Practice Guidelines for Prevention and Management of Avalanche and Nonavalanche Snow Burial Accidents in 2017 [10]. Finally, in 2021, the ERC updated their guidelines [20].
3.2. Companion and Organized Rescue
The highly time dependent survival from complete avalanche burial highlights the importance of immediate rescue by uninjured companions [32]. The likelihood of survival can be four times higher if the victim is rescued by uninjured companions compared to organized rescue [32]. Once at the scene, it takes at least 3–5 min to locate a completely buried person. Once located, in a simulation study with manikins buried at a depth of 1 m, it took an average of 7 min to free the airway, plus a further 3 min to initiate cardiopulmonary resuscitation (CPR). The number of rescuers (one compared to two) and the body position of the buried manikin had no significant influence on extrication times [33]. Since asphyxia is the most frequent cause of death in the early phase of burial, basic life support by first responders must include ventilations and chest compressions (compression-only CPR is not recommended [2].
Organized rescue differs from companion rescue because the response time is typically longer, resources are more available, and group size is larger. For avalanche rescue, if conditions allow, helicopters should be given priority over ground rescue teams, as they are faster, safer, and more efficient. Helicopters can also be used to search from the air with avalanche transceivers and RECCO® (see below) [34]. However, air rescue operations may be restricted by adverse weather conditions with low visibility and wind.
An organized search for a completely buried avalanche victim can rely on visual and acoustic methods, avalanche transceivers, avalanche dogs, the RECCO® rescue system, and probing. Companions and rescuers should immediately search for clues on the surface and acoustic signs (calling out and listening for victims’ cries for help). Rescue dogs are trained to detect buried victims by scent. The initial dog search should be with the handler before the terrain is contaminated by helicopter fumes. The search continues with avalanche transceivers and the RECCO® system, if available [34]. The RECCO® technology system is a two-part system, featuring an active detector, carried by the rescuer, and a passive reflector diode, embedded into the victim’s clothing. It is used by more than 600 rescue organizations worldwide, especially in ski areas [34]. If attempts with avalanche transceivers and RECCO® fail, rescuers should begin a probe-line search. The initial probing depth should be limited to 1.5 m and the ‘Three Holes per Step’ or the ‘Slalom’ probing techniques should be used [10]. A probe line leader is necessary to ensure accuracy and effectiveness. Professional healthcare personnel should be at the scene to treat victims during and after extrication.
Every ground or air rescuer who enters avalanche terrain must be properly equipped with an avalanche transceiver and, ideally, an avalanche airbag. Medical equipment should be protected from the cold. Electronic instruments should have full batteries. Rescue equipment should include rescue bags, which are similar to sleeping bags but modified for rescue use, or other insulating layers, aluminum blankets, chemical heat packs, a thermometer suitable for measuring core temperature, and a cardiac monitor/defibrillator [2].
3.3. Extrication, Initial Assessment and Monitoring
In an organized avalanche search and rescue (SAR) operation, the duration of victim burial usually exceeds 35 min. Victims can be expected to be mildly or moderately hypothermic. For this reason, extrication and the initial assessment should be carried out as carefully, rather than as rapidly, as possible. Rescuers should first assess the position of a victim, then dig a channel towards their head. The rescuer who uncovers the face should check whether there is an air pocket in front of the mouth and nose, noting whether the airway is open or is blocked by snow or debris. Ideally, these observations should be made by a rescuer trained in advanced life support (ALS) or an emergency physician. Knowing whether the airway was patent or obstructed and if there was an air pocket is crucial for decisions concerning resuscitation and transport. If the position of the victim allows, the first assessment of the airway and vital signs should be made before complete extrication. An ECG should be obtained as soon as possible, before removal and transport of the victim, as it allows for the detection of arrhythmias provoked by movement of the patient [35]. Core temperature should be measured using an esophageal probe or a low reading thermistor-based epitympanic thermometer [36]. Esophageal temperature measurement correlates well with cardiac temperature. An esophageal probe placed with the distal end in the lower third of the esophagus is considered the gold standard for patients in cardiac arrest or in whom advanced airway management is necessary [37]. Epitympanic measurement using a thermistor is a reliable alternative in patients not in cardiac arrest but may register a much lower temperature than actual core temperature if the environment is very cold [38]. The probe must be well insulated and the external auditory canal must be free of snow or water. Epitympanic probes not manufactured for outdoor use should not be used at the scene [36]. Pulse oximetry is not mandatory, as it may be inaccurate with cold exposure due to peripheral vasoconstriction.
As soon as a victim is extricated, a first assessment should be made to look for vital signs and evident injuries. Cardiac activity and core temperature should be continuously monitored throughout the rescue for early detection of after-drop or circum-rescue collapse. If a defibrillator is available, defibrillator pads should be put in position. The victim should be protected from cold and wind [2][20].
3.4. Trauma Management
Chest and head trauma are the most frequent injuries in avalanches, while spinal, abdominal, and limb injuries are less frequent [26]. General concepts of trauma management also apply to avalanche victims: Current resuscitation guidelines emphasize early hemorrhage control, damage-control resuscitation, advanced airway management if indicated, stabilization of injuries, and prompt evacuation to definitive care [39][40]. Spinal motion restriction, splinting limb fractures, and administration of effective analgesia should be performed during on-site management and transport. In severe head trauma, early intubation and normocapnic ventilation is recommended. Tourniquets can be life-saving in exsanguinating limb injuries. Immediate chest decompression is mandatory for tension pneumothorax. For pneumo- or hemothorax, a thoracostomy tube should be considered, particularly before evacuation by helicopter if a climb in altitude is expected and the victim is intubated.
In victims of traumatic cardiac arrest, survival is low; prolonged CPR is associated with poor neurological outcomes.
3.5. Airway Management and Ventilation
For unconscious avalanche victims, advanced airway management provides effective oxygenation, reducing the likelihood of aspiration. Endotracheal intubation can, rarely, provoke ventricular fibrillation in victims with moderate or severe hypothermia, usually at a core temperature < 30 °C [41][42]. As the evidence for this is mainly animal-based; the small risk is far outweighed by the advantages of airway control [43][44].
Whether ventilation in unconscious avalanche victims should target normocapnia (endtidal CO2 35–45 mmHg) is controversial. Hypocapnia, (endtidal CO2 <35 mmHg) due to excessive ventilation or decreased metabolic production of CO2, decreases cerebral blood flow due to vasoconstriction, which can induce arrhythmias as frequently as hypercapnia, especially in victims with hypothermia. Normoxia may protect against malignant arrhythmias, as it improves myocardial stability in asphyxiated as well as in severely hypothermic victims. It seems likely that adequate oxygenation might help to reduce the risk of circum-rescue collapse.
Endotracheal intubation requires training and practice; therefore, it should be done only by qualified rescuers with a high tracheal intubation success rate [45]. Placement of supraglottic devices is easier and safer than endotracheal intubation [46]. For rescuers who are not experienced in advanced airway management, ventilation is most effective with mouth-to-mask or bag–valve–mask techniques. For a survivor with an unsecured airway, hospital transport should be expedited for advanced airway management [22].
References
- Techel, F.; Jarry, F.; Kronthaler, G.; Mitterer, S.; Nairz, P.; Pavšek, M.; Valt, M.; Darms, G. Avalanche fatalities in the European Alps: Long-term trends and statistics. Geogr. Helvetica 2016, 71, 147–159.
- Brugger, H.; Durrer, B.; Elsensohn, F.; Paal, P.; Strapazzon, G.; Winterberger, E.; Zafren, K.; Boyd, J. Resuscitation of avalanche victims: Evi-dence-based guidelines of the international commission for mountain emergency medicine (ICAR MEDCOM): Intended for physi-cians and other advanced life support personnel. Resuscitation 2013, 84, 539–546.
- Atkins, D. 10 years of avalanche rescues in the United States, 2003/04 to 2012/13. Avalanche Rev. 2015, 33, 22–24.
- Schweizer, J.; Lütschg, M. Characteristics of human-triggered avalanches. Cold Reg. Sci. Technol. 2001, 33, 147–162.
- Rainer, B.; Frimmel, C.; Sumann, G.; Brugger, H.; Kinzl, J.F.; Lederer, W. Correlation between avalanche emergencies and avalanche danger forecast in the alpine region of Tyrol. Eur. J. Emerg. Med. 2008, 15, 43–47.
- Strapazzon, G.; Schweizer, J.; Chiambretti, I.; Brodmann Maeder, M.; Brugger, H.; Zafren, K. Effects of Climate Change on Ava-lanche Accidents and Survival. Front Physiol. 2021, 12, 639433.
- Strapazzon, G.; Paal, P.; Schweizer, J.; Falk, M.; Reuter, B.; Schenk, K.; Gatterer, H.; Grasegger, K.; Cappello, T.D.; Malacrida, S.; et al. Effects of snow properties on humans breathing into an artificial air pocket–An experimental field study. Sci. Rep. 2017, 7, 17675.
- Brugger, H.; Durrer, B.; Adler-Kastner, L.; Falk, M.; Tschirky, F. Field management of avalanche victims. Resuscitation 2001, 51, 7–15.
- Haegeli, P.; Falk, M.; Brugger, H.; Etter, H.-J.; Boyd, J. Comparison of avalanche survival patterns in Canada and Switzerland. Can. Med. Assoc. J. 2011, 183, 789–795.
- Van Tilburg, C.; Grissom, C.K.; Zafren, K.; McIntosh, S.; Radwin, M.I.; Paal, P.; Haegeli, P.; Smith, W.W.R.; Wheeler, A.R.; Weber, D.; et al. Wilderness Medical Society Practice Guidelines for Prevention and Management of Avalanche and Nonavalanche Snow Burial Accidents. Wilderness Environ. Med. 2017, 28, 23–42.
- Falk, M.; Brugger, H.; Adler-Kastner, L. Avalanche survival chances. Nature 1994, 368, 21.
- Procter, E.; Strapazzon, G.; Cappello, T.D.; Zweifel, B.; Würtele, A.; Renner, A.; Falk, M.; Brugger, H. Burial duration, depth and air pocket explain avalanche survival patterns in Austria and Switzerland. Resuscitation 2016, 105, 173–176.
- Strapazzon, G.; Brugger, H.; Paal, P.; Brown, D. Reconsidering the air pocket around mouth and nose as a positive outcome predictor in completely buried avalanche victims. Resuscitation 2020, 152, 208–209.
- Strapazzon, G.; Putzer, G.; Cappello, T.D.; Falla, M.; Braun, P.; Falk, M.; Glodny, B.; Pinggera, D.; Helbok, R.; Brugger, H. Effects of hypothermia, hypoxia, and hypercapnia on brain oxygenation and hemodynamic parameters during simulated avalanche burial: A porcine study. J. Appl. Physiol. 2021, 130, 237–244.
- Brugger, H.; Etter, H.J.; Boyd, J.; Falk, M. Causes of death from avalanche. Wilderness Environ. Med. 2009, 20, 93–96.
- Paal, P.; Strapazzon, G.; Braun, P.; Ellmauer, P.P.; Schroeder, D.C.; Sumann, G.; Werner, A.; Wenzel, V.; Falk, M.; Brugger, H. Factors affecting survival from avalanche burial—A randomised prospective porcine pilot study. Resuscitation 2013, 84, 239–243.
- Brugger, H.; Sumann, G.; Meister, R.; Adler-Kastner, L.; Mair, P.; Gunga, H.C.; Schobersberger, W.; Falk, M. Hypoxia and hypercapnia during respiration into an artificial air pocket in snow: Implications for avalanche survival. Resuscitation 2003, 58, 81–88.
- Strapazzon, G.; Gatterer, H.; Falla, M.; Cappello, T.D.; Malacrida, S.; Turner, R.; Schenk, K.; Paal, P.; Falk, M.; Schweizer, J.; et al. Hypoxia and hypercapnia effects on cerebral oxygen saturation in avalanche burial: A pilot human experimental study. Resuscitation 2020, 158, 175–182.
- Boyd, J.; Brugger, H.; Shuster, M. Prognostic factors in avalanche resuscitation: A systematic review. Resuscitation 2010, 81, 645–652.
- Lott, C.; Truhlář, A.; Alfonzo, A.; Barelli, A.; González-Salvado, V.; Hinkelbein, J.; Nolan, J.P.; Paal, P.; Perkins, G.D.; Thies, K.-C.; et al. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation 2021, 161, 152–219.
- Eidenbenz, D.; Techel, F.; Kottmann, A.; Rousson, V.; Carron, P.-N.; Albrecht, R.; Pasquier, M. Survival probability in avalanche victims with long burial (≥60 min): A retrospective study. Resuscitation 2021.
- Paal, P.; Gordon, L.; Strapazzon, G.; Brodmann Maeder, M.; Putzer, G.; Walpoth, B.; Wanscher, M.; Brown, D.; Holzer, M.; Broessner, G.; et al. Accidental hypothermia-an update: The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 111.
- Locher, T.; Walpoth, B.H. Differential diagnosis of circulatory failure in hypothermic avalanche victims: Retrospective analysis of 32 avalanche accidents. Praxis 1996, 85, 1275–1282.
- Oberhammer, R.; Beikircher, W.; Hörmann, C.; Lorenz, I.; Pycha, R.; Adler-Kastner, L.; Brugger, H. Full recovery of an avalanche victim with profound hypothermia and prolonged cardiac arrest treated by extracorporeal re-warming. Resuscitation 2008, 76, 474–480.
- Mittermair, C.; Foidl, E.; Wallner, B.; Brugger, H.; Paal, P. Extreme Cooling Rates in Avalanche Victims: Case Report and Narrative Review. High Alt. Med. Biol. 2021, 22, 235–240.
- Hohlrieder, M.; Brugger, H.; Schubert, H.M.; Pavlic, M.; Ellerton, J.; Mair, P. Pattern And Severity of Injury in Avalanche Victims. High Alt. Med. Biol. 2007, 8, 56–61.
- Brugger, H.; Durrer, B.; Adler-Kastner, L. On-site triage of avalanche victims with asystole by the emergency doctor. Resuscitation 1996, 31, 11–16.
- Brugger, H.; Durrer, B. On-Site Treatment of Avalanche Victims ICAR-MEDCOM-Recommendation. High Alt. Med. Biol. 2002, 3, 421–425.
- Soar, J.; Perkins, G.; Abbas, G.; Alfonzo, A.; Barelli, A.; Bierens, J.J.; Brugger, H.; Deakin, C.D.; Dunning, J.; Georgiou, M.; et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation 2010, 81, 1400–1433.
- Vanden Hoek, T.L.; Morrison, L.J.; Shuster, M.; Donnino, M.; Sinz, E.; Lavonas, E.J.; Jeejeebhoy, F.M.; Gabrielli, A. Part 12: Cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010, 122, S829–S861.
- Soar, J.; Bossaert, L.L.; Monsieurs, K.; Nikolaou, N.I.; Truhlář, A.; Zideman, D.A.; Maconochie, I.K.; Nolan, J.P.; Greif, R.; Perkins, G.D.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015, 95, 1–80.
- Mair, P.; Frimmel, C.; Vergeiner, G.; Hohlrieder, M.; Moroder, L.; Hoesl, P.; Voelckel, W. Emergency medical helicopter operations for ava-lanche accidents. Resuscitation 2013, 84, 492–495.
- Wallner, B.; Moroder, L.; Brandt, A.; Mair, P.; Erhart, S.; Bachler, M.; Putzer, G.; Turner, R.; Strapazzon, G.; Falk, M.; et al. Extrication Times During Avalanche Companion Rescue: A Randomized Single-Blinded Manikin Study. High Alt. Med. Biol. 2019, 20, 245–250.
- Grasegger, K.; Strapazzon, G.; Procter, E.; Brugger, H.; Soteras, I. Avalanche Survival After Rescue With the RECCO Rescue System: A Case Report. Wilderness Environ. Med. 2016, 27, 282–286.
- Strapazzon, G.; Beikircher, W.; Procter, E.; Brugger, H. Msc Electrical Heart Activity Recorded During Prolonged Avalanche Burial. Circulation 2012, 125, 646–647.
- Strapazzon, G.; Procter, E.; Paal, P.; Brugger, H. Pre-hospital core temperature measurement in accidental and therapeutic hy-pothermia. High Alt. Med. Biol. 2014, 15, 104–111.
- Pasquier, M.; Paal, P.; Kosinski, S.; Brown, D.; Podsiadlo, P.; DaRocha, T. Esophageal Temperature Measurement. N. Engl. J. Med. 2020, 383, e93.
- Strapazzon, G.; Procter, E.; Putzer, G.; Avancini, G.; Cappello, T.D.; Überbacher, N.; Hofer, G.; Rainer, B.; Rammlmair, G.; Brugger, H. Influence of low ambient temperature on epitympanic temperature measurement: A prospective randomized clinical study. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 90.
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J.; Komadina, R.; Maegele, M.; Nardi, G.; Riddez, L.; et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit. Care 2019, 23, 98.
- Sumann, G.; Moens, D.; Brink, B.; Brodmann Maeder, M.; Greene, M.; Jacob, M.; Koirala, P.; Zafren, K.; Ayala, M.; Musi, M.; et al. Multiple trauma management in mountain environments—A scoping review: Evidence based guidelines of the International Commission for Mountain Emergency Medicine (ICAR MedCom). Intended for physicians and other advanced life support personnel. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 1–22.
- Papenhausen, M.; Burke, L.; Antony, A.; Phillips, J. Severe hypothermia with cardiac arrest: Complete neurologic recovery in a 4-year-old child. J. Pediatr. Surg. 2001, 36, 1590–1592.
- Osborne, L.; El-Din, A.S.K.; Smith, J.E. Survival after prolonged cardiac arrest and accidental hypothermia. BMJ 1984, 289, 881–882.
- Gillen, J.P.; Vogel, M.F.; Holterman, R.K.; Skiendzielewski, J.J. Ventricular fibrillation during orotracheal intubation of hypothermic dogs. Ann. Emerg. Med. 1986, 15, 412–416.
- Danzl, D.F.; Pozos, R.S.; Auerbach, P.S.; Glazer, S.; Goetz, W.; Johnson, E.; Jui, J.; Lilja, P.; Marx, J.A.; Miller, J.; et al. Multicenter hypothermia survey. Ann. Emerg. Med. 1987, 16, 1042–1055.
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation 2021, 161, 115–151.
- Gruber, E.; Oberhammer, R.; Balkenhol, K.; Strapazzon, G.; Procter, E.; Brugger, H.; Falk, M.; Paal, P. Basic life support trained nurses ventilate more efficiently with laryngeal mask supreme than with facemask or laryngeal tube suction-disposable--a prospective, randomized clinical trial. Resuscitation 2014, 85, 499–502.
More
Information
Subjects:
Emergency Medicine
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.5K
Revisions:
2 times
(View History)
Update Date:
13 Oct 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




