
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ayodeji Iyanda | + 6886 word(s) | 6886 | 2021-08-05 04:26:40 | | | |
| 2 | Dean Liu | -15 word(s) | 6871 | 2021-08-09 10:44:54 | | | | |
| 3 | Dean Liu | -6199 word(s) | 672 | 2022-04-13 11:24:20 | | |
Video Upload Options
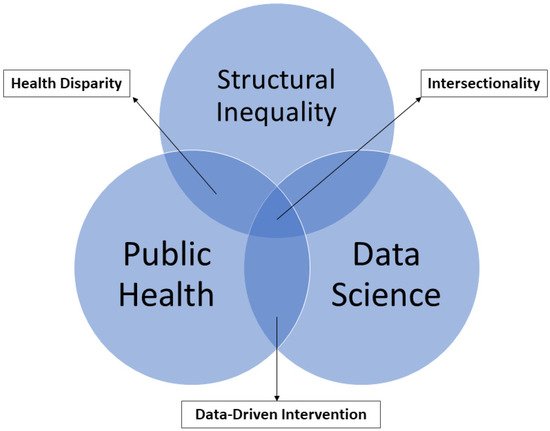
Health disparity is an unacceptable, unjust, or inequitable difference in health outcomes among different groups of people that affects access to optimal health care, as well as deterring it. Health disparity adversely affects disadvantaged subpopulations due to a higher incidence and prevalence of a particular disease or ill health. Existing health disparity determines whether a disease outbreak such as coronavirus disease 2019, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), will significantly impact a group or a region. Hence, health disparity assessment has become one of the focuses of many agencies, public health practitioners, and other social scientists. Successful elimination of health disparity at all levels requires pragmatic approaches through an intersectionality framework and robust data science.
References
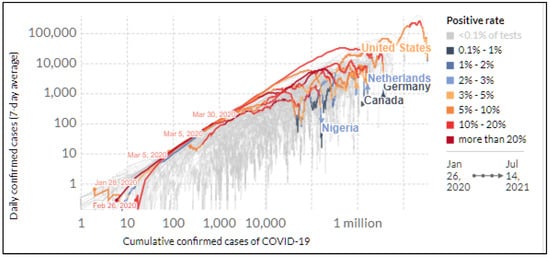
- Iyanda, A.E.; Adeleke, R.; Lu, Y.; Osayomi, T.; Adaralegbe, A.; Lasode, M.; Chima-Adaralegbe, N.J.; Osundina, A.M. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: A multiscale geographically weighted regression analysis (January 11–June 28, 2020). J. Infect. Public Health 2020, 13, 1438–1445.
- John Hopkins Coronavirus Research Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 23 June 2021).
- Kandi, V.; Thungaturthi, S.; Vadakedath, S.; Gundu, R.; Mohapatra, R.K. Mortality Rates of Coronavirus Disease 2019 (COVID-19) Caused by the Novel Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). Cureus 2021, 13, e14081.
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776.
- Chaudhry, R.; Dranitsaris, G.; Mubashir, T.; Bartoszko, J.; Riazi, S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine 2020, 25, 100464.
- Christie, A. Decreases in COVID-19 Cases, Emergency Department Visits, Hospital Admissions, and Deaths Among Older Adults Following the Introduction of COVID-19 Vaccine—United States, September 6, 2020–May 1, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 858–864. Available online: https://www.cdc.gov/mmwr/volumes/70/wr/mm7023e2.htm (accessed on 16 July 2021).
- Moghadas, S.M.; Vilches, T.N.; Zhang, K.; Wells, C.R.; Shoukat, A.; Singer, B.H.; Meyers, L.A.; Neuzil, K.M.; Langley, J.M.; Fitzpatrick, M.C.; et al. The impact of vaccination on COVID-19 outbreaks in the United States. Clin. Infect. Dis. 2021, ciab079.
- Reuters. UK Coronavirus Vaccines Have Weakened Link between Infections and Death, Says Scientist. 2021. Available online: https://www.reuters.com/world/uk/uk-coronavirus-vaccines-have-weakened-link-between-infections-death-says-2021-06-27/ (accessed on 16 July 2021).
- World Health Organization. Vaccine Efficacy, Effectiveness and Protection. 2021. Available online: https://www.who.int/news-room/feature-stories/detail/vaccine-efficacy-effectiveness-and-protection (accessed on 16 July 2021).
- Roser, M.; Ritchie, H.; Ortiz-Ospina, E.; Hasell, J. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 10 August 2020).

