
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mario Gagliardi | + 1236 word(s) | 1236 | 2021-07-16 11:05:52 | | | |
| 2 | Peter Tang | Meta information modification | 1236 | 2021-07-28 05:12:52 | | |
Video Upload Options
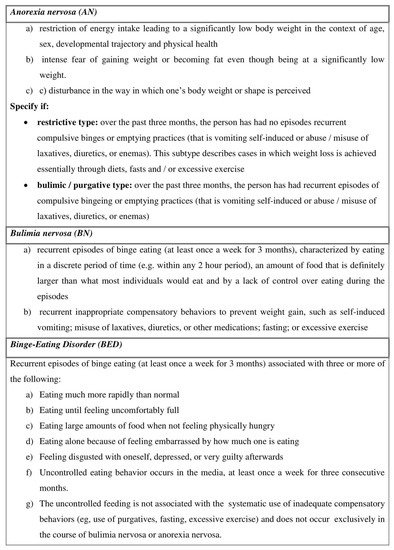
Eating disorders (ED) are frequently associated with a wide range of psychiatric or somatic comorbidities. The most relevant ED are anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorders (BED). Patients with ED exhibit both upper and lower gastrointestinal (GI) symptoms. Evidence of alterations throughout the GI tract in ED will be analyzed given the role of the GI tract in food intake and its regulation. It remains a matter of debate whether GI disorders are inherent manifestations of ED or the results of malnutrition occurring from ED. Moreover, recent clinical studies have highlighted the growing role of intestinal microbiota in the pathogenesis of ED, making it possible to hypothesize a modulation of intestinal microbiota as a co-adjuvant to standard therapy.
1. Eating Disorders
2. ED and GI Tract
3. Conclusions
References
- Lewinsohn, P.M.; Hops, H.; Roberts, R.E.; Seeley, J.R.; Andrews, J.A. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J. Abnorm. Psychol. 1993, 102, 133–144.
- Association, A.P. Diagnostic and statistical manual of mental disorders. In DSM—5; American Psychological Association: Washington, DC, USA, 2015.
- Hetterich, L.; Mack, I.; Giel, K.E.; Zipfel, S.; Stengel, A. An update on gastrointestinal disturbances in eating disorders. Mol. Cell. Endocrinol. 2018, 497, 110318.
- Udo, T.; Grilo, C.M. Prevalence and Correlates of DSM-5-Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biol. Psychiatry 2018, 84, 345–354.
- Smink, F.R.; van Hoeken, D.; Hoek, H.W. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Curr. Psychiatry Rep. 2012, 14, 406–414.
- Favaro, A.; Caregaro, L.; Tenconi, E.; Bosello, R.; Santonastaso, P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J. Clin. Psychiatry 2009, 70, 1715–1721.
- Keski-Rahkonen, A.; Hoek, H.W.; Linna, M.S.; Raevuori, A.; Sihvola, E.; Bulik, C.M.; Rissanen, A.; Kaprio, J. Incidence and outcomes of bulimia nervosa: A nationwide population-based study. Psychol. Med. 2009, 39, 823–831.
- Cossrow, N.; Pawaskar, M.; Witt, E.A.; Ming, E.E.; Victor, T.W.; Herman, B.K.; Wadden, T.A.; Erder, M.H. Estimating the Prevalence of Binge Eating Disorder in a Community Sample From the United States: Comparing DSM-IV-TR and DSM-5 Criteria. J. Clin. Psychiatry 2016, 77, e968–e974.
- Olguin, P.; Fuentes, M.; Gabler, G.; Guerdjikova, A.I.; Keck, P.E., Jr.; McElroy, S.L. Medical comorbidity of binge eating disorder. Eat. Weight Disord. EWD 2017, 22, 13–26.
- Stunkard, A.J. Eating disorders and obesity. Psychiatr. Clin. N. Am. 2011, 34, 765–771.
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000.
- Silverman, J.A. Louis-Victor Marce, 1828–1864: Anorexia nervosa’s forgotten man. Psychol. Med. 1989, 19, 833–835.
- Perkins, S.J.; Keville, S.; Schmidt, U.; Chalder, T. Eating disorders and irritable bowel syndrome: Is there a link? J. Psychosom. Res. 2005, 59, 57–64.
- Boyd, C.; Abraham, S.; Kellow, J. Psychological features are important predictors of functional gastrointestinal disorders in patients with eating disorders. Scand. J. Gastroenterol. 2005, 40, 929–935.
- Salvioli, B.; Pellicciari, A.; Iero, L.; Di Pietro, E.; Moscano, F.; Gualandi, S.; Stanghellini, V.; De Giorgio, R.; Ruggeri, E.; Franzoni, E. Audit of digestive complaints and psychopathological traits in patients with eating disorders: A prospective study. Dig. Liver Dis. 2013, 45, 639–644.
- Guerdjikova, A.I.; Mori, N.; Casuto, L.S.; McElroy, S.L. Binge Eating Disorder. Psychiatr. Clin. N. Am. 2017, 40, 255–266.
- Ulfvebrand, S.; Birgegard, A.; Norring, C.; Hogdahl, L.; von Hausswolff-Juhlin, Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015, 230, 294–299.
- Bohn, K.; Doll, H.A.; Cooper, Z.; O’Connor, M.; Palmer, R.L.; Fairburn, C.G. The measurement of impairment due to eating disorder psychopathology. Behav. Res. Ther. 2008, 46, 1105–1110.
- Abraham, S.; Kellow, J.E. Do the digestive tract symptoms in eating disorder patients represent functional gastrointestinal disorders? BMC Gastroenterol. 2013, 13, 38.
- Zipfel, S.; Sammet, I.; Rapps, N.; Herzog, W.; Herpertz, S.; Martens, U. Gastrointestinal disturbances in eating disorders: Clinical and neurobiological aspects. Auton. Neurosci. Basic Clin. 2006, 129, 99–106.
- Norris, M.L.; Harrison, M.E.; Isserlin, L.; Robinson, A.; Feder, S.; Sampson, M. Gastrointestinal complications associated with anorexia nervosa: A systematic review. Int. J. Eat. Disord. 2016, 49, 216–237.
- McCallum, R.W.; Grill, B.B.; Lange, R.; Planky, M.; Glass, E.E.; Greenfeld, D.G. Definition of a gastric emptying abnormality in patients with anorexia nervosa. Dig. Dis. Sci. 1985, 30, 713–722.
- Kamal, N.; Chami, T.; Andersen, A.; Rosell, F.A.; Schuster, M.M.; Whitehead, W.E. Delayed gastrointestinal transit times in anorexia nervosa and bulimia nervosa. Gastroenterology 1991, 101, 1320–1324.
- Hutson, W.R.; Wald, A. Gastric emptying in patients with bulimia nervosa and anorexia nervosa. Am. J. Gastroenterol. 1990, 85, 41–46.
- Rigaud, D.; Bedig, G.; Merrouche, M.; Vulpillat, M.; Bonfils, S.; Apfelbaum, M. Delayed gastric emptying in anorexia nervosa is improved by completion of a renutrition program. Dig. Dis. Sci. 1988, 33, 919–925.
- Hill, L.D.; Kozarek, R.A.; Kraemer, S.J.; Aye, R.W.; Mercer, C.D.; Low, D.E.; Pope, C.E., 2nd. The gastroesophageal flap valve: In vitro and in vivo observations. Gastrointest. Endosc. 1996, 44, 541–547.
- Abell, T.L.; Malagelada, J.R.; Lucas, A.R.; Brown, M.L.; Camilleri, M.; Go, V.L.; Azpiroz, F.; Callaway, C.W.; Kao, P.C.; Zinsmeister, A.R.; et al. Gastric electromechanical and neurohormonal function in anorexia nervosa. Gastroenterology 1987, 93, 958–965.
- Passananti, V.; Siniscalchi, M.; Zingone, F.; Bucci, C.; Tortora, R.; Iovino, P.; Ciacci, C. Prevalence of eating disorders in adults with celiac disease. Gastroenterol. Res. Pract. 2013, 2013, 491657.
- Vella, A.; Camilleri, M. The Gastrointestinal Tract as an Integrator of Mechanical and Hormonal Response to Nutrient Ingestion. Diabetes 2017, 66, 2729–2737.
- Latorre, R.; Sternini, C.; De Giorgio, R.; Greenwood-Van Meerveld, B. Enteroendocrine cells: A review of their role in brain-gut communication. Neurogastroenterol. Motil. 2016, 28, 620–630.
- Depoortere, I. Taste receptors of the gut: Emerging roles in health and disease. Gut 2014, 63, 179–190.
- Furness, J.B.; Rivera, L.R.; Cho, H.J.; Bravo, D.M.; Callaghan, B. The gut as a sensory organ. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 729–740.
- Iovino, P.; Azpiroz, F.; Domingo, E.; Malagelada, J.R. The sympathetic nervous system modulates perception and reflex responses to gut distention in humans. Gastroenterology 1995, 108, 680–686.
- Brookes, S.J.; Spencer, N.J.; Costa, M.; Zagorodnyuk, V.P. Extrinsic primary afferent signalling in the gut. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 286–296.
- Wang, G.J.; Tomasi, D.; Backus, W.; Wang, R.; Telang, F.; Geliebter, A.; Korner, J.; Bauman, A.; Fowler, J.S.; Thanos, P.K.; et al. Gastric distention activates satiety circuitry in the human brain. NeuroImage 2008, 39, 1824–1831.
- Jones, K.L.; Doran, S.M.; Hveem, K.; Bartholomeusz, F.D.; Morley, J.E.; Sun, W.M.; Chatterton, B.E.; Horowitz, M. Relation between postprandial satiation and antral area in normal subjects. Am. J. Clin. Nutr. 1997, 66, 127–132.
- Camilleri, M. Integrated upper gastrointestinal response to food intake. Gastroenterology 2006, 131, 640–658.
- Enck, P.; Azpiroz, F.; Boeckxstaens, G.; Elsenbruch, S.; Feinle-Bisset, C.; Holtmann, G.; Lackner, J.M.; Ronkainen, J.; Schemann, M.; Stengel, A.; et al. Functional dyspepsia. Nat. Rev. Dis. Primers 2017, 3, 17081.
- Iovino, P.; Angrisani, L.; Galloro, G.; Consalvo, D.; Tremolaterra, F.; Pascariello, A.; Ciacci, C. Proximal stomach function in obesity with normal or abnormal oesophageal acid exposure. Neurogastroenterol. Motil. 2006, 18, 425–432.
- Citrome, L. Binge-Eating Disorder and Comorbid Conditions: Differential Diagnosis and Implications for Treatment. J. Clin. Psychiatry 2017, 78 (Suppl. S1), 9–13.
- Guarda, A.S.; Schreyer, C.C.; Boersma, G.J.; Tamashiro, K.L.; Moran, T.H. Anorexia nervosa as a motivated behavior: Relevance of anxiety, stress, fear and learning. Physiol. Behav. 2015, 152, 466–472.
- Drossman, D.A. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 2016.




