
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Wolfgang Boedeker | + 1619 word(s) | 1619 | 2021-08-11 10:05:55 | | | |
| 2 | Camila Xu | + 409 word(s) | 2028 | 2021-08-17 04:04:21 | | | | |
| 3 | Camila Xu | + 409 word(s) | 2028 | 2021-08-17 04:05:02 | | |
Video Upload Options
Pesticides are considered highly hazardous when presenting high acute toxicity according to internationally accepted classification systems such as the WHO Recommended Classification of Pesticides by Hazard. In addition, pesticides that cause severe or irreversible harm to health “… under conditions of use in a country” may be considered as highly hazardous.
1. Introduction
It took more than 30 years for an updated estimation to be published, finding that worldwide annually 385 million cases of unintentional acute pesticide poisoning are expected to occur, including around 11,000 fatalities [1]. Additionally, 110,000–168,000 fatalities were lately estimated to occur from suicidal pesticide poisoning worldwide mostly in rural agricultural areas in low- and middle-income countries [2]. During the last decades, international bodies have taken up the issue of health hazards from pesticide exposure and adopted a great number of resolutions and programs to improve their safe use [3]. Realizing, however, that despite all efforts there might be no safe use of toxic pesticides especially under conditions of poverty, the International Code of Conduct on Pesticide Management of WHO and the Food and Agriculture Organization (FAO) endorses a new policy approach by considering the prohibition of highly hazardous pesticides [4].
Pesticides are considered highly hazardous when presenting high acute toxicity according to internationally accepted classification systems such as the WHO Recommended Classification of Pesticides by Hazard [5]. In addition, pesticides that cause severe or irreversible harm to health “… under conditions of use in a country” may be considered as highly hazardous [4].
Case fatality and severity scores might be a more realistic indicator for human toxicity of substances than hazard classes based on animal testing. If so, the indicators should primarily point to the substance-specific toxic properties and not on the characteristics of the incident and treatment e.g., cause, dose, and time lag between exposition and treatment. A low variability of the e.g., pesticide specific case-fatality-rate (CFR) would then indicate problematic chemicals from a public health perspective as the human toxicity of an agent in general was captured rather than the clinical course of a specific poisoning. Recently, it has been suggested that a case fatality after self-poisoning greater than 5% should be used as an indicator of a highly hazardous pesticide and that a complete ban of these pesticides be targeted [6].
In order to study whether and which indicators of the severity of poisonings can be used to prioritize pesticides of public health concern we systematically reviewed the scientific literature. We aimed at answering the following research questions: For which active ingredients in pesticides or for which group of pesticides have human case- fatality-ratios been published? What is the geographical distribution and the variability of the reported case-fatality ratios? What is the relationship between the human case-fatality and WHO hazard classes? Which factors influence the case-fatality? Which severity scores are used with respect to pesticide poisonings?
2. Methods
We conducted a systematic literature review without prior protocol by starting the search for publications in the database PUBMED. We used the terms “pesticides” AND (“case-fatality-ratio” OR “case-fatality-rate” OR “poisoning severity score”) and allowed for studies in English, German, Portuguese, and Spanish with a publication date between January 1990 and October 2014. The search procedure was repeated with the database SCOPUS which has a higher coverage outside medical sciences and includes the database EMBASE completely as of 1996. In a sensitivity analysis addressing our search strategy and a possibly too strict selection, we additionally searched for specific pesticides and checked these with the results in our automatic search as outlined below.
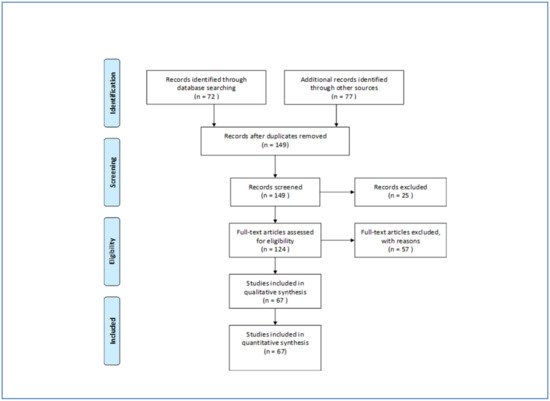
According to the PRISMA-Statement (prisma-statement.org) all records were screened and excluded in case abstracts clearly indicated non-eligibility, e.g., when only specific symptoms of poisonings or animals were studied. Full-text-analysis was carried out on all other records. Studies were considered eligible when addressing active ingredients in pesticides or groups of active ingredients (e.g., organophosphates). Case-studies and papers which do not report or not allow to calculate a case fatality were excluded. The search was supplemented by inspecting bibliographic reference lists in all identified papers. Articles initially not identified by the automatic search were then manually back searched. Finally, 149 papers were identified of which 67 could be included after assessment. We excluded 25 papers by abstract and 57 by full-text analysis mainly because no information on active ingredients or group of pesticides was presented ( Figure 1 ).
Case fatality was extracted from all included publications. In most papers, case fatality was referred to as case-fatality-ratio (CFR) or mortality-ratio and was given as number of fatal poisonings divided by the number of all poisonings with a specific agent or group of agents respectively. When the CFR was not stated in the studies that we calculated from given numbers of incidents. Case fatality and indicators used as descriptors of the poisoning severity as well as information on the number of patients, the country, year, cause of poisoning, and timespan of the study were retrieved study-wise for each poisoning agent in a data base.
Overall, case numbers and CFR were studied by minimum, mean, median, and maximum values. The cross-study variability of the CFR was assessed by the coefficient of variation (CV) as the ratio of the standard deviation to the mean and its normalized form which limits the CV to the interval 0–1 and adjusts for the number of observations [7]. Mathematically, a CV lower or equal 100% indicates low variability taking the exponential distribution as a reference. Calculation of CV was restricted to those pesticides which were addressed in more than three papers. All calculations were done with SAS statistical software, Version 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
Sixty-seven publications [8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41][42][43][44][45][46][47][48][49][50][51][52][53][54][55][56][57][58][59][60][61][62][63][64][65][66][67][68][69][70][71][72][73][74] reporting case fatality rates on 66 active ingredients and additionally on 13 groups of active ingredients were identified ( Table 1 ). Moreover, 58% of the active ingredients are covered by just one publication. The most mentioned active ingredient is glyphosate which is addressed in 16 papers followed by paraquat in 14 papers. With respect to groups of pesticides organophosphates are most frequently studied. Thirty-one papers report on studies from 14 different countries. In total, 20 countries are covered by the included studies with Taiwan and Sri Lanka most often addressed ( Table 2 ).
Of the active ingredients considered, 17% show case-fatality above 20. Table 3 shows how the CFR is captured by the WHO Recommended Classification of Pesticides by Hazard.
Thirty-two pesticide groups or active ingredients were studied by more than one paper and nine by more than three papers. Table 4 gives the coefficients of variation (CV) along with case-fatalities and WHO-classification on all pesticides addressed in more than three publications. All CFR show a coefficient of variation lower or equal 100%. Four out of the seven active ingredients are seen with a CV even well below 100% whereas only malathion and glyphosate reach 93% and 100%, respectively. Glyphosate serves as an example of how study characteristics impact on the variability of CFR. The highest value of 29% was seen in a study in Taiwan [35] recruiting in two hospitals which serve as referral hospitals and include a poisoning control center. The lowest value of 0.06% follows from two deaths in 3464 human exposure cases (98% unintentional) collected in the US National Poison Data System by telephone calls received in 57 regional poison centers [45]. If only those cases treated in health care facilities were taken as the denominator (see Mowry et al. p 1165) , the CFR would be 3.6% and further decrease the variability across countries. With respect to the normalized coefficient of variation, which adjusts for the number of publications, malathion is the active ingredient with the highest variability but also well below the possible 100%.
Clinical indicators for the severity of poisonings were mentioned in many papers. Although the Poisoning Severity Score (PSS) was part of the search terms we found more papers reporting on the Glasgow Coma Score (GCS). Additionally, the Acute Physiology and Chronic Health Evaluation Score (APACHE), the Sequential Organ Failure Assessment (SOFA), and the Simplified Acute Physiology Score (SAPS) were used along with scores built specifically by the study authors ( Table 5 ). Studies often aim at a comparison of different indicators with respect to their performance for predicting study specific clinical outcomes. More information on the used indicators is available in some studies, e.g., mean and grading of scores. However, the number of papers in this entry is too limited to study the variability of indicators with respect to specific group of pesticides or active ingredients.
| Group of Pesticide | Publications | Countries | Case-Fatality-Ratio (%) | Cases (n) | Severity Indicator 1 | Country | Reference | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | Median | Min | Max | Median | Min | Max | ||||
| carbamates | 9 | 6 | 5.1 | 0.0 | 14.2 | 60 | 6 | 1433 | CFR | Brazil, India, Israel, Serbia, Sri Lanka, Taiwan | [8][9][15][25][40][42][66][68][73] |
| carbamates/OP 2 | 1 | 1 | 5.0 | 280 | PSS, CFR | Brazil | [14] | ||||
| chloracetanilide | 1 | 1 | 3.6 | 28 | CFR, PSS | Korea | [55] | ||||
| coumarin | 1 | 1 | 0.0 | 82 | PSS, CFR | Brazil | [14] | ||||
| cyanide | 1 | 1 | 24.1 | CFR | Taiwan | [73] | |||||
| diethyl-OP | 1 | 1 | 38.0 | 8 | CFR, PSS, APACHE, SOFA, GCS | Germany | [30] | ||||
| dimethyl-OP | 1 | 1 | 11.0 | 19 | CFR, PSS, APACHE, SOFA, GCS | Germany | [30] | ||||
| fungicides | 1 | 1 | 6.1 | 49 | CFR | Sri Lanka | [9] | ||||
| herbicides | 1 | 1 | 12.4 | 2783 | CFR | Sri Lanka | [9] | ||||
| organochlorines | 2 | 2 | 18.4 | 16.7 | 20.0 | 112 | 12 | 212 | CFR | India, Sri Lanka | [8][9] |
| organophosphate | 31 | 14 | 11.1 | 2.9 | 73.0 | 94 | 16 | 5226 | CFR, APACHE, PSS, SOFA, GCSCFR, SAPS, CFRCFR, SAPSII | Australia, China, Germany, India, Iran, Israel, Japan, Jordan, Slovenia, SouthAfrica, Sri Lanka, Taiwan, Turkey, Zimbabwe | [8][9][11][12][13][15][16][19][20][22][27][28][29][30][33][39][41][50][53][54][57][61][62][63][66][67][69][71][72][73][74] |
| pyrethrins | 1 | 1 | 0.0 | 5522 | CFR | USA | [45] | ||||
| pyrethroids | 3 | 3 | 0.7 | 0.0 | 1.0 | 203 | 140 | 23,853 | PSS, CFR | Brazil, Sri Lanka, USA | [9][14][45] |
| Active Ingredients | |||||||||||
| 2,4-D | 1 | 1 | 5.5 | 20 | CFR | Brazil | [51] | ||||
| abamectin | 1 | 1 | 11.1 | 18 | CFR | Sri Lanka | [9] | ||||
| acephate | 1 | 1 | 29.0 | 14 | CFR | India | [8] | ||||
| acetamiprid | 1 | 1 | 0.0 | 11 | CFR | Sri Lanka | [9] | ||||
| alachlor | 2 | 2 | 8.0 | 4.8 | 11.1 | 36 | 9 | 63 | CFR | Sri Lanka, Taiwan | [9][43] |
| aldicarb | 2 | 2 | 2.6 | 0.0 | 5.2 | 37 | 35 | 39 | CFR, PSS | France, USA | [48][49] |
| aldrin | 1 | 1 | 13.3 | 49 | CFR | Brazil | [51] | ||||
| aluminium phosphide | 2 | 1 | 48.9 | 31.0 | 66.7 | 255 | 39 | 471 | CFR, APACHE, SAPS, GCS | Iran | [58][59] |
| bispyribac-sodium | 1 | 1 | 2.9 | 103 | CFR | Sri Lanka | [9] | ||||
| butachlor | 1 | 1 | 0.0 | 70 | CFR | Taiwan | [43] | ||||
| carbaryl | 1 | 1 | 5.6 | 18 | CFR | Sri Lanka | [9] | ||||
| carbofuran | 3 | 2 | 2.9 | 1.0 | 4.1 | 209 | 100 | 479 | CFR | Brazil, Sri Lanka | [9][10][51] |
| carbosulfan | 2 | 1 | 17.1 | 10.7 | 23.5 | 198 | 51 | 345 | CFR | Sri Lanka | [9][10] |
| chlorfluazuron | 1 | 1 | 2.2 | 45 | CFR | Sri Lanka | [9] | ||||
| chlorpyrifos | 7 | 3 | 6.2 | 5.2 | 8.0 | 208 | 34 | 1376 | CFR, GCS, PSS | Brazil, India, Sri Lanka | [8][9][10][20][23][26][51] |
| cypermethrin | 2 | 2 | 6.1 | 5.1 | 7.0 | 50 | 41 | 58 | CFR | Brazil, India | [8][51] |
| deltamethrin | 1 | 1 | 0.0 | 11 | CFR | Sri Lanka | [9] | ||||
| diazinon | 1 | 1 | 4.8 | 84 | CFR | Sri Lanka | [9] | ||||
| dichlorvos | 2 | 1 | 32.3 | 31.3 | 33.3 | 13 | 9 | 16 | CFR | Japan | [47][72] |
| dimethoate | 6 | 2 | 23.6 | 5.5 | 30.8 | 268 | 17 | 833 | CFR, GCS, PSS | Brazil, Sri Lanka | [9][10][20][23][26][51] |
| diquat | 1 | 1 | 0.0 | 312 | CFR | USA | [45] | ||||
| edifenphos | 1 | 1 | 11.8 | 17 | CFR | Sri Lanka | [9] | ||||
| endosulfan | 6 | 3 | 22.9 | 20.2 | 29.3 | 86 | 9 | 400 | CFR | Brazil, India, Sri Lanka | [8][9][10][33][46][51] |
| endrin | 1 | 1 | 5.0 | 74 | CFR | India | [8] | ||||
| esfenvalerate | 1 | 1 | 8.3 | 12 | CFR | Sri Lanka | [9] | ||||
| etofenprox | 1 | 1 | 0.8 | 121 | CFR | Sri Lanka | [9] | ||||
| fenitrothion | 2 | 1 | 15.4 | 9.4 | 21.3 | 40 | 32 | 47 | CFR | Japan | [47][72] |
| fenobucarb | 2 | 1 | 5.6 | 5.3 | 5.8 | 71 | 38 | 104 | CFR | Sri Lanka | [9][10] |
| fenoxaprop-p-ethyl | 1 | 1 | 0.0 | 74 | CFR | Sri Lanka | [9] | ||||
| fenthion | 4 | 1 | 13.9 | 4.3 | 16.2 | 111 | 23 | 237 | CFR, GCS, PSS | Sri Lanka | [9][10][20][23] |
| fipronil | 1 | 1 | 0.0 | 26 | CFR | Sri Lanka | [9] | ||||
| glufosinate | 1 | 1 | 7.1 | 14 | CFR | Japan | [47] | ||||
| glyphosate | 16 | 6 | 6.1 | 0.1 | 29.3 | 102 | 15 | 3464 | CFR, PSS | Brazil, Japan, Korea, Sri Lanka, Taiwan, USA | [9][10][15][17][18][35][36][45][47][51][52][56][60][64][65][73] |
| hydrogen phosphide | 1 | 1 | 2.6 | 152 | CFR, PSS | Germany | [34] | ||||
| imidacloprid | 2 | 2 | 0.0 | 0.0 | 0.0 | 39 | 8 | 70 | CFR | India, Sri Lanka | [8][9] |
| indoxacarb | 1 | 1 | 14.0 | 7 | CFR | India | [8] | ||||
| lindane | 1 | 1 | 0.0 | 3 | CFR | Sri Lanka | [9] | ||||
| malathion | 7 | 5 | 6.5 | 0.0 | 25.0 | 23 | 5 | 209 | CFR, APACHE | Brazil, India, Japan, Singapore, Sri Lanka | [8][9][10][37][47][51][72] |
| MCPA | 2 | 1 | 5.1 | 4.8 | 5.4 | 387 | 93 | 681 | CFR | Sri Lanka | [9][10] |
| metam sodium | 1 | 1 | 0.0 | 102 | CFR | France | [21] | ||||
| methamidophos | 3 | 2 | 12.5 | 11.5 | 15.4 | 26 | 8 | 191 | CFR | Brazil, Sri Lanka | [9][10][51] |
| methomyl | 2 | 1 | 7.2 | 0.0 | 14.3 | 31 | 7 | 54 | CFR | Sri Lanka | [9][10] |
| monocrotophos | 3 | 3 | 22.2 | 20.4 | 35.0 | 99 | 54 | 257 | CFR | Brazil, India, Sri Lanka | [8][10][51] |
| oxydemeton-methyl | 2 | 2 | 13.4 | 12.5 | 14.3 | 11 | 8 | 14 | CFR, PSS, APACHE, SOFA, GCSCFR | Germany, Sri Lanka | [9][30] |
| oxyfluorfen | 1 | 1 | 0.0 | 15 | CFR | Sri Lanka | [9] | ||||
| paraquat | 14 | 6 | 54.2 | 1.4 | 83.6 | 115 | 7 | 1046 | CFR | Brazil, Japan, Korea, Sri Lanka, Taiwan, USA | [9][10][15][17][25][31][32][38][44][45][47][51][70][73] |
| parathion ethyl | 1 | 1 | 42.9 | 7 | CFR, PSS, APACHE, SOFA, GCS | Germany | [30] | ||||
| parathion methyl | 1 | 1 | 60.0 | 5 | CFR | India | [8] | ||||
| permethrin | 1 | 1 | 0.0 | 13 | CFR | Sri Lanka | [9] | ||||
| petrilachlor | 1 | 1 | 0.0 | 11 | CFR | Sri Lanka | [9] | ||||
| phenthoate | 2 | 1 | 7.4 | 6.5 | 8.3 | 96 | 24 | 168 | CFR | Sri Lanka | [9][10] |
| phorate | 1 | 1 | 19.0 | 21 | CFR | India | [8] | ||||
| picloram | 1 | 1 | 25.0 | 5 | CFR | Brazil | [51] | ||||
| pirimiphos-methyl | 1 | 1 | 0.0 | 12 | CFR | Sri Lanka | [9] | ||||
| profenofos | 2 | 1 | 5.5 | 0.0 | 11.0 | 84 | 22 | 146 | CFR | Sri Lanka | [9][10] |
| propamocarb | 1 | 1 | 100.0 | 1 | CFR | Sri Lanka | [9] | ||||
| propanil | 3 | 1 | 5.0 | 1.6 | 10.9 | 150 | 64 | 412 | CFR | Sri Lanka | [9][10][24] |
| propoxur | 1 | 1 | 0.0 | 16 | CFR | Sri Lanka | [9] | ||||
| prothiofos | 1 | 1 | 7.7 | 13 | CFR | Sri Lanka | [9] | ||||
| quinalphos | 2 | 2 | 12.1 | 12.0 | 12.1 | 101 | 78 | 124 | CFR | India, Sri Lanka | [8][9] |
| rotenone | 1 | 1 | 0.0 | 54 | CFR | USA | [45] | ||||
| spinosad | 1 | 1 | 0.0 | 4 | CFR | India | [8] | ||||
| triazophos | 1 | 1 | 17.0 | 6 | CFR | India | [8] | ||||
| trichlorfon | 2 | 1 | 18.8 | 0.0 | 37.5 | 8 | 7 | 8 | CFR | Japan | [47][72] |
| trifuralin | 1 | 1 | 0.0 | 17 | CFR | Brazil | [51] | ||||
| zink phosphide | 2 | 1 | 7.6 | 4.2 | 11.0 | 30 | 24 | 35 | CFR | India | [46][74] |
| Country | No. of Paper | No. of Papers Providing Case-Fatality on | |
|---|---|---|---|
| Group Level | Active Ingredient Level | ||
| Australia | 1 | 1 | - |
| Brazil | 3 | 2 | 1 |
| China | 1 | 1 | - |
| France | 2 | - | 2 |
| Germany | 2 | 1 | 2 |
| India | 8 | 7 | 4 |
| Iran | 3 | 1 | 2 |
| Israel | 4 | 4 | - |
| Japan | 3 | 1 | 3 |
| Jordan | 1 | 1 | - |
| Korea | 5 | 1 | 4 |
| Serbia | 1 | 1 | - |
| Singapore | 1 | - | 1 |
| Slovenia | 1 | 1 | - |
| South Africa | 2 | 2 | - |
| Sri Lanka | 10 | 5 | 9 |
| Taiwan | 12 | 3 | 10 |
| Turkey | 4 | 4 | - |
| USA | 2 | 1 | 2 |
| Zimbabwe | 1 | 1 | - |
| All | 67 | 38 | 40 |
| WHO Class * | Median Case-Fatality-Ratio | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <1 | 1 – <10 | 10 – <20 | ≥20% | All | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Ia | 1 | 4 | 1 | 8 | 2 | 18 | 4 | 6 | ||
| Ib | 3 | 13 | 5 | 38 | 2 | 18 | 10 | 15 | ||
| II | 11 | 61 | 14 | 58 | 6 | 46 | 4 | 36 | 35 | 53 |
| III | 3 | 17 | 3 | 13 | 6 | 9 | ||||
| O | 1 | 4 | 1 | 8 | 2 | 3 | ||||
| U | 4 | 22 | 1 | 4 | 2 | 18 | 7 | 11 | ||
| VF | 1 | 4 | 1 | 9 | 2 | 3 | ||||
| All | 18 | 100 | 24 | 100 | 13 | 100 | 11 | 100 | 66 | 100 |
| Name | WHO Class ** | Publications | Cases | Case Fatality Ratio | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | Median | Min | Mean | Median | Max | CV | CV Norm | ||
| carbamates | 9 | 60 | 0 | 5 | 5 | 14 | 98 | 35 | |
| organophosphate | 31 | 94 | 3 | 15 | 11 | 73 | 92 | 17 | |
| chlorpyrifos | II | 7 | 208 | 5 | 7 | 6 | 8 | 19 | 8 |
| dimethoate | II | 6 | 268 | 6 | 22 | 24 | 31 | 40 | 18 |
| endosulfan | II | 6 | 86 | 20 | 24 | 23 | 29 | 16 | 7 |
| fenthion | II | 4 | 111 | 4 | 12 | 14 | 16 | 44 | 26 |
| glyphosate | III | 16 | 102 | 0 | 7 | 6 | 29 | 100 | 26 |
| malathion | III | 7 | 23 | 0 | 10 | 7 | 25 | 93 | 38 |
| paraquat | II | 14 | 115 | 1 | 49 | 54 | 84 | 56 | 16 |
References
- Boedeker, W.; Watts, M.; Clausing, P.; Marquez, E. The global distribution of acute unintentional pesticide poisoning: Estimations based on a systematic review. BMC Public Health 2020, 20, 1–19.
- Mew, E.J.; Padmanathan, P.; Konradsen, F.; Eddleston, M.; Chang, S.-S.; Phillips, M.R.; Gunnell, D. The global burden of fatal self-poisoning with pesticides 2006–2015: Systematic review. J. Affect. Disord. 2017, 219, 93–104.
- Dinham, B. Communities in Peril: Global Report on Health Impacts of Pesticide Use in Agriculture; Pesticide Action Network Asia Pacific: Penang, Malaysia, 2021; Available online: http://www.pan-germany.org/download/PAN-I_CBM-Global-Report_1006-final.pdf (accessed on 25 May 2021).
- WHO & FAO—World Health Organization and Food and Agriculture Organization. International Code of Conduct on Pesticide Management. Guidelines on Highly Hazardous Pesticides. Available online: http://apps.who.int/iris/bitstream/10665/205561/1/9789241510417_eng.pdf (accessed on 25 May 2021).
- WHO—World Health Organization. WHO Recommended Classification of Pesticides by Hazard and Guideline to Classification. Available online: http://www.who.int/ipcs/publications/pesticides_hazard/en/ (accessed on 25 May 2021).
- Buckley, N.A.; Fahim, M.; Raubenheimer, J.; Gawarammana, I.B.; Eddleston, M.; Roberts, M.S.; Dawson, A.H. Case fatality of agricultural pesticides after self-poisoning in Sri Lanka: A prospective cohort study. Lancet Glob. Health 2021, 9, e854–e862.
- Martin, J.; David, L.N. Gray Measurement of Relative Variation: Sociological Examples. Am. Sociol. Rev. 1971, 36, 496.
- Rao, C.S.; Venkateswarlu, V.; Surender, T.; Eddleston, M.; Buckley, N.A. Pesticide poisoning in south India: Opportunities for prevention and improved medical management. Trop. Med. Int. Health 2005, 10, 581–588.
- Dawson, A.H.; Eddleston, M.; Senarathna, L.; Mohamed, F.; Gawarammana, I.; Bowe, S.J.; Manuweera, G.; Buckley, N.A. Acute Human Lethal Toxicity of Agricultural Pesticides: A Prospective Cohort Study. PLoS Med. 2010, 7, e1000357.
- Van der Hoek, W.; Konradsen, F. Analysis of 8000 hospital admissions for acute poisoning in a rural area of Sri Lanka. Clin. Toxicol. 2006, 44, 225–231.
- Agarwal, S. A Clinical, Biochemical, Neurobehavioral, and Sociopsychological Study of 190 Patients Admitted to Hospital as a Result of Acute Organophosphorus Poisoning. Environ. Res. 1993, 62, 63–70.
- Akdur, O.; Durukan, P.; Özkan, S.; Avsarogullari, L.; Vardar, A.; Kavalci, C.; Ikizceli, I. Poisoning severity score, Glasgow coma scale, corrected QT interval in acute organophosphate poisoning. Hum. Exp. Toxicol. 2010, 29, 419–425.
- Bilgin, T.E.; Camdeviren, H.; Yapici, D.; Doruk, N.; Altunkan, A.A.; Altunkan, Z.; Oral, U. The comparison of the efficacy of scoring systems in organophosphate poisoning. Toxicol. Ind. Health 2005, 21, 141–146.
- Caldas, E.D.; Rebelo, F.M.; Heliodoro, V.O.; Magalhaes, A.F.A.; Rebelo, R.M. Poisonings with pesticides in the Federal District of Brazil. Clin. Toxicol. 2008, 46, 1058–1063.
- Carroll, R.; Metcalfe, C.; Gunnell, D.; Mohamed, F.; Eddleston, M. Diurnal variation in probability of death following self-poisoning in Sri Lanka-evidence for chronotoxicity in humans. Int. J. Epidemiol. 2012, 41, 1821–1828.
- Chaou, C.H.; Lin, C.C.; Chen, H.Y.; Lee, C.H.; Chen, T.H.H. Chlorpyrifos is associated with slower serum cholinesterase recovery in acute organophosphate-poisoned patients. Clin. Toxicol. 2013, 51, 402–408.
- Chen, H.-H.; Lin, J.-L.; Huang, W.-H.; Weng, C.-H.; Lee, S.-Y.; Hsu, C.-W.; Chen, K.-H.; Wang, I.-K.; Liang, C.-C.; Chang, C.-T. Spectrum of corrosive esophageal injury after intentional paraquat or glyphosate-surfactant herbicide ingestion. Int. J. Gen. Med. 2013, 6, 677–683.
- Chen, Y.J.; Wu, M.L.; Deng, J.F.; Yang, C.C. The epidemiology of glyphosate-surfactant herbicide poisoning in Taiwan, 1986–2007: A poison center study. Clin. Toxicol. 2009, 47, 670–677.
- Churi, S.; Bhakta, K.; Madhan, R. Organophosphate Poisoning: Prediction of Severity and Outcome by Glasgow Coma Scale, Poisoning Severity Score, Acute Physiology and Chronic Health Evaluation Ii Score, and Simplified Acute Physiology Score Ii. J. Emerg. Nurs. 2012, 38, 493–495.
- Davies, J.O.J.; Eddleston, M.; Buckley, N.A. Predicting outcome in acute organophosphorus poisoning with a poison severity score or the Glasgow coma scale. Qjm. Int. J. Med. 2008, 101, 371–379.
- Deguigne, M.B.; Lagarce, L.; Boels, D.; Harry, P. Metam sodium intoxication: The specific role of degradation products—Methyl isothiocyanate and carbon disulphide—As a function of exposure. Clin. Toxicol. 2011, 49, 416–422.
- Dippenaar, R.; Diedericks, R.J. Paediatric organophosphate poisoning—A rural hospital experience. Samj. S. Afr. Med. J. 2005, 95, 678–681.
- Eddleston, M.; Eyer, P.; Worek, F.; Mohamed, F.; Senarathna, L.; von Meyer, L.; Juszczak, E.; Hittarage, A.; Azhar, S.; Dissanayake, W.; et al. Differences between organophosphorus insecticides in human self-poisoning: A prospective cohort study. Lancet 2005, 366, 1452–1459.
- Eddleston, M.; Rajapakshe, M.; Roberts, D.; Reginald, K.; Sheriff, M.H.R.; Dissanayake, W.; Buckley, N. Severe Propanil [N-(3,4-Dichlorophenyl) Propanamide] Pesticide Self-Poisoning. J. Toxicol. Clin. Toxicol. 2002, 40, 847–854.
- Eddleston, M.; Sudarshan, K.; Senthilkumaran, M.; Reginald, K.; Karalliedde, L.; Senarathna, L.; de Silva, D.; Sheriff, M.H.R.; Buckley, N.A.; Gunnell, D. Patterns of hospital transfer for self-poisoned patients in rural Sri Lanka: Implications for estimating the incidence of self-poisoning in the developing world. Bull. World Health Organ. 2006, 84, 276–282.
- Eddleston, M.; Eyer, P.; Worek, F.; Sheriff, M.H.R.; Buckley, N.A. Predicting outcome using butyryl-cholinesterase activity in organophosphorus pesticide self-poisoning. Qjm. Int. J. Med. 2008, 101, 467–474.
- Emerson, G.M.; Gray, M.N.; Jelinek, G.A.; Mountain, D.; Mead, H.J. Organophosphate poisoning in Perth, Western Australia, 1987. J. Emerg. Med. 1999, 17, 273–277.
- Goel, A.; Joseph, S.; Dutta, T.K. Organophosphate poisoning: Predicting the need for ventilatory support. J. Assoc. Physicians India 1998, 46, 786–790.
- Grmec, S.; Mally, S.; Klemen, P. Glasgow coma scale score and QTc interval in the prognosis of organophosphate poisoning. Acad. Emerg. Med. 2004, 11, 925–930.
- Hrabetz, H.; Thiermann, H.; Felgenhauer, N.; Zilker, T.; Haller, B.; Nahrig, J.; Saugel, B.; Eyer, F. Organophosphate poisoning in the developed world—A single centre experience from here to the millennium. Chem. Biol. Interact. 2013, 206, 561–568.
- Huang, N.C.; Lin, S.L.; Hung, Y.M.; Hung, S.Y.; Chung, H.M. Severity assessment in acute paraquat poisoning by analysis of APACHE II score. J. Formos. Med. Assoc. 2003, 102, 782–787.
- Ikebuchi, J.; Proudfoot, A.T.; Matsubara, K.; Hampson, E.C.G.M.; Tomita, M.; Suzuki, K.; Fuke, C.; Ijiri, I.; Tsu-nerari, T.; Yuasa, I.; et al. Toxicological Index of Paraquat—A New Strategy for Assessment of Severity of Paraquat Poisoning in 128 Patients. Forensic Sci. Int. 1993, 59, 85–87.
- Kumar, S.V.; Venkateswarlu, V.; Sasikala, M.; Kumar, G.V. A study on poisoning cases in a tertiary care hospital. J. Nat. Sci. Biol. Med. 2010, 1, 35–39.
- Lauterbach, M.; Solak, E.; Kaes, J.; Wiechelt, J.; Von Mach, M.A.; Weilemann, L.S. Epidemiology of hydrogen phosphide exposures in humans reported to the poison center in Mainz, Germany, 1983. Clin. Toxicol. 2005, 43, 575–581.
- Lee, C.H.; Shih, C.P.; Hsu, K.H.; Hung, D.Z.; Lin, C.C. The early prognostic factors of glypho-sate-surfactant intoxication. Am. J. Emerg. Med. 2008, 26, 275–281.
- Lee, H.L.; Chen, K.W.; Chi, C.H.; Huang, J.J.; Tsai, L.M. Clinical presentations and prognostic factors of a glyphosate-surfactant herbicide intoxication: A review of 131 cases. Acad. Emerg. Med. 2000, 7, 906–910.
- Lee, P.; Tai, D.Y.H. Clinical features of patients with acute organophosphate poisoning requiring intensive care. Intensive Care Med. 2001, 27, 694–699.
- Lee, Y.; Lee, J.H.; Seong, A.J.; Hong, C.K.; Lee, H.J.; Shin, D.H.; Hwang, S.Y. Arterial lactate as a predictor of mortality in emergency department patients with paraquat intoxication. Clin. Toxicol. 2012, 50, 52–56.
- Levy-Khademi, F.; Tenenbaum, A.N.; Wexler, I.D.; Amitai, Y. Unintentional organophosphate in-toxication in children. Pediatric Emerg. Care 2007, 23, 716–718.
- Lifshitz, M.; Shahak, E.; Bolotin, A.; Sofer, S. Carbamate poisoning in early childhood and in adults. J. Toxicol. Clin. Toxicol. 1997, 35, 25–27.
- Lifshitz, M.; Shahak, E.; Sofer, S. Carbamate and organophosphate poisoning in young children. Pediatr. Emerg. Care 1999, 15, 102–103.
- Lima, J.S.; Reis, C.A.G. Poisoning Due to Illegal Use of Carbamates as a Rodenticide in Rio-De-Janeiro. J. Toxicol. Clin. Toxicol. 1995, 33, 687–690.
- Lo, Y.C.; Yang, C.C.; Deng, J.F. Acute alachlor and butachlor herbicide poisoning. Clin. Toxicol. 2008, 46, 716–721.
- Min, Y.G.; Ahn, J.H.; Chan, Y.C.; Ng, S.H.; Tse, M.L.; Lau, F.L.; Chan, C.K. Prediction of prognosis in acute paraquat poisoning using severity scoring system in emergency department. Clin. Toxicol. 2011, 49, 840–845.
- Mowry, J.B.; Spyker, D.A.; Cantilena, L.R.; Bailey, J.E.; Ford, M. ABSTRACTS 2012 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report Abstracts. Clin. Toxicol. 2013, 51, 949–1229.
- Murali, R.; Bhalla, A.; Singh, D.; Singh, S. Acute pesticide poisoning: 15 years experience of a large North-West Indian hospital. Clin. Toxicol. 2009, 47, 35–38.
- Nagami, H.; Nishigaki, Y.; Matsushima, S.; Matsushita, T.; Asanuma, S.; Yajima, N.; Usuda, M.; Hirosawa, M. Hospital-based survey of pesticide poisoning in Japan, 1998. Int. J. Occup. Environ. Health 2005, 11, 180–184.
- Nelson, L.S.; Perrone, J.; DeRoos, F.; Stork, C.; Hoffman, R.S. Aldicarb poisoning bay an illicit rodenticide imported into the United States: Tres Pasitos. J. Toxicol. Clin. Toxicol. 2001, 39, 447–452.
- Nisse, P.; Deveaux, M.; Tellart, A.S.; Dherbecourt, V.; Peucelle, D.; Mathieu-Nolf, M. Aldicarb poisoning: Review of the intoxication cases in north of France 1998. Acta Clin. Belg. Supp. 2002, 1, 12–15.
- Peter, J.V.; Thomas, L.; Graham, P.L.; Moran, J.L.; Abhilash, K.P.P.; Jasmine, S.; Iyyadurai, R. Performance of clinical scoring systems in acute organophosphate poisoning. Clin. Toxicol. 2013, 51, 850–854.
- Recena, M.C.P.; Pires, D.X.; Caldas, E.D. Acute poisoning with pesticides in the state of Mato Grosso do Sul, Brazil. Sci. Total Environ. 2006, 357, 88–95.
- Roberts, D.M.; Buckley, N.A.; Mohamed, F.; Eddleston, M.; Goldstein, D.A.; Mehrsheikh, A.; Bleeke, M.S.; Dawson, A.H. A prospective observational study of the clinical toxicology of glyphosate-containing herbicides in adults with acute self-poisoning. Clin. Toxicol. 2010, 48, 129–136.
- Saadeh, A.M.; Alali, M.K.; Farsakh, N.A.; Ghani, M.A. Clinical and sociodemographic features of acute carbamate and organophosphate poisoning: A study of 70 adult patients in North Jordan. J. Toxicol. Clin. Toxicol. 1996, 34, 45–51.
- Senanayake, N.; Desilva, H.J.; Karalliedde, L. A Scale to Assess Severity in Organophosphorus Intoxication—Pop Scale. Hum. Exp. Toxicol. 1993, 12, 297–299.
- Seok, S.J.; Park, J.S.; Hong, J.R.; Gil, H.W.; Yang, J.O.; Lee, E.Y.; Song, H.Y.; Hong, S.Y. Surfactant volume is an essential element in human toxicity in acute glyphosate herbicide intoxication. Clin. Toxicol. 2011, 49, 892–899.
- Seok, S.J.; Choi, S.C.; Gil, H.W.; Yang, J.O.; Lee, E.Y.; Song, H.Y.; Hong, S.Y. Acute Oral Poisoning Due to Chloracetanilide Herbicides. J. Korean Med. Sci. 2012, 27, 111–114.
- Shadnia, S.; Darabi, D.; Pajoumand, A.; Salimi, A.; Abdollahi, M. A simplified acute physiology score in the prediction of acute organophosphate poisoning outcome in an intensive care unit. Hum. Exp. Imental Toxicol. 2007, 26, 623–627.
- Shadnia, S.; Mehrpour, O.; Soltaninejad, K. A simplified acute physiology score in the prediction of acute aluminum phosphide poisoning. Indian J. Med. Sci 2010, 64, 532–539.
- Shadnia, S.; Sasanian, G.; Allami, P.; Hosseini, A.; Ranjbar, A.; Amini-Shirazi, N.; Abdollahi, M. A retrospective 7-years study of aluminum phosphide poisoning in Tehran: Opportunities for prevention. Hum. Exp. Toxicol. 2009, 28, 209–213.
- Suh, J.H.; Oh, B.J.; Roh, H.K. Clinical outcomes after suicidal ingestion of glyphosate surfactant herbicide: Severity of intoxication according to amount ingested. Clininal Toxicol. 2007, 45, 641.
- Sungur, M.; Guven, M. Intensive care management of organophosphate insecticide poisoning. Crit. Care 2001, 5, 211–215.
- Sungurtekin, H.; Gurses, E.; Balci, C. Evaluation of several clinical scoring tools in organophos-phate poisoned patients. Clin. Toxicol. 2006, 44, 121–126.
- Tagwireyi, D.; Ball, D.E.; Nhachi, C.F.B. Toxicoepidemiology in Zimbabwe: Pesticide poisoning admissions to major hospitals. Clin. Toxicol. 2006, 44, 59–66.
- Talbot, A.R.; Shiaw, M.H.; Huang, J.S.; Yang, S.F.; Goo, T.S.; Wang, S.H.; Chen, C.L.; Sanford, T.R. Acute-Poisoning with A Glyphosate-Surfactant Herbicide (Round-Up)—A Review of 93 Cases. Hum. Exp. Toxicol. 1991, 10, 1–8.
- Tominack, R.L.; Yang, G.Y.; Tsai, W.J.; Chung, H.M.; Deng, J.F. Taiwan-National-Poison-Center Survey of Glyphosate Surfactant Herbicide Ingestions. J. Toxicol. Clin. Toxicol. 1991, 29, 91–109.
- Tsao, T.C.Y.; Juang, Y.C.; Lan, R.S.; Shieh, W.B.; Lee, C.H. Respiratory-Failure of Acute Organophos-phate and Carbamate Poisoning. Chest 1990, 98, 631–636.
- Verhulst, L.; Waggie, Z.; Hatherill, M.; Reynolds, L.; Argent, A. Presentation and outcome of severe anticholinesterase insecticide poisoning. Arch. Dis. Child. 2002, 86, 352–355.
- Vucinic, S.; Jovanovic, D.; Antonijevic, B.; Vucinic, Z.; Djordjevic, D.; Potrebic, O.; Rezic, T. Acute carbamate poisoning treated in the National Poison Control Centre during ten years period. Clin. Toxicol. 2009, 47, 506–507.
- Weissmann-Brenner, A.; David, A.; Vidan, A.; Hourvitz, A. Organophosphate poisoning: A multi-hospital survey. Isr. Med. Assoc. J. 2002, 4, 573–576.
- Weng, C.H.; Hu, C.C.; Lin, J.L.; Lin-Tan, D.T.; Huang, W.H.; Hsu, C.W.; Yen, T.H. Sequential Organ Failure Assessment Score Can Predict Mortality in Patients with Paraquat Intoxication. PLoS ONE 2012, 7, e51743.
- Xia, C.Y.; Wang, M.; Liang, Q.; Yun, L.A.; Kang, H.S.; Fan, L.; Wang, D.S.; Zhang, G.Y. Changes in monoclonal HLA-DR antigen expression in acute organophosphorus pesticide-poisoned patients. Exp. Ther. Med. 2014, 7, 137–140.
- Yamashita, M.; Yamashita, M.; Tanaka, J.; Ando, Y. Human mortality in organophosphate poisonings. Vet. Hum. Toxicol. 1997, 39, 84–85.
- Yang, C.C.; Wu, J.F.; Ong, H.C.; Hung, S.C.; Kuo, Y.P.; Sa, C.H.; Chen, S.S.; Deng, J.F. Taiwan National Poison Center: Epidemiologic data 1985. J. Toxicol. Clin. Toxicol. 1996, 34, 651–663.
- Zaheer, M.S.; Aslam, M.; Gupta, V.; Sharma, V.; Khan, S.A. Profile of poisoning cases at A North Indian tertiary care hospital. Health Popul. Perspect. Issues 2009, 32, 176–183.




