Risk of COVID-19 exposure and more severe illness are serious concerns for older adults. Social distancing has worsened existing social isolation, with severe impacts on connectedness among seniors. The pandemic is threatening to cause an extended health crisis, with impacts including serious health consequences. The pandemic has worsened social isolation among older adults. Social isolation has become urgent, as seniors have lost their usual connections due to social distancing. While safety measures are critical to prevent virus exposure, this approach must be balanced with maintaining social connectedness. The pandemic highlights the importance of social connections, with significant impacts on both community-living older adults and those in nursing facilities.
1. Background
The need for social connectedness among older adults has been studied extensively; experts state that being socially connected is critical to health and survival
[1][2][3]. Social connectedness plays a prominent role in preventing both loneliness and social isolation, with social isolation specifically defined as an objective measure of one’s social interactions, relationships, networks, and support
[2][3]. Social isolation is estimated to impact up to 40% of adults aged 60 and older in the US
[2]. According to the National Health and Aging Trends Study report, released in early 2020 just before the novel coronavirus (COVID-19) outbreak, 28% of older adults aged 65+ in the US (9 million) were already socially isolated at that time
[4][5][6].
The negative impacts of social isolation later in life have been widely reported, ranging from declining mental and physical health to reduced quality of life, increased mortality, and higher Medicare costs
[7][8][9][10]. Older adults who live alone, with limited resources and cognition/memory issues, are at even greater risk of social isolation, worsened significantly by the COVID-19 pandemic
[11].
Worldwide spread of the pandemic triggered an urgent, ongoing public health crisis in the US and worldwide, beginning in early 2020
[12]. Significant effects include millions of infections along with widespread, serious illness and death; devastating strain and shortages within the healthcare system; severe economic ramifications; growing mental health concerns; and strict social distancing efforts leading to greater social isolation among the most vulnerable individuals
[12].
Older adults have been disproportionately impacted by COVID-19, with higher susceptibility to severe illness, hospitalization, and death
[13]. In the US, those who are age 65+ comprised about 80% of all COVID-19 deaths as of late 2020; worldwide, estimates suggest that 95% of pandemic related deaths have been among those age 60 and older
[13][14]. While the physical illness and death impact has been emphasized, the pandemic has taken a toll on mental health and quality of life, as well
[3][12][15].
Social distancing has significantly impacted social connectedness especially among seniors who are already isolated
[3][15]. Although recommendations have varied by state and by urban versus rural areas, social distancing has been especially important for vulnerable older adults due to their high risk of severe illness resulting from COVID-19 infection. Thus, from early in the pandemic, older adults in most areas have been urged to stay home as much as possible until recent availability has improved access to approved COVID-19 vaccines. Consequently, increased social isolation has added to family and caregiver burden, reduced access to healthcare services, strained support networks, and hampered coping strategies for many
[16]. Older individuals who previously left their homes regularly for social activities, volunteering, doctors’ appointments, family visits, and errands have generally suspended these activities due to strong recommendations and strict guidelines urging older Americans to stay home. Thus, their social connectedness, one of several factors recently identified to be key personal determinants of health
[17], has been severely impacted. Notably, a collection of personal factors has been defined as personal determinants of health, or PDOH—an emerging concept built on the individual resources that help buffer challenges in life and support optimal health outcomes
[17]. In addition to social connectedness, other important PDOH including resilience and purpose in life may potentially decrease over the long term for many individuals as a result of the pandemic, with the abrupt absence of normal support systems, roles, and activities
[3][15][17]. Furthermore, older adults who are hospitalized for COVID-19 infections with a poor prognosis may not be able to perform life completion and end-of-life tasks due to current hospital restrictions such as prohibited family visits, creating a reality that may reduce quality of life for the patient and cause distress for family members
[16].
The pandemic has made these realities increasingly challenging, as every area of life has changed in efforts to slow the spread of the virus
[3]. Downstream consequences include not only an economic recession, but also the potential for a social recession, recently defined as a lasting collapse in social contact resulting from compounded social isolation, especially among the most vulnerable
[3][12][18]. A long social recession could worsen the well-known negative impacts of social isolation, encompassing both physical and mental health outcomes as well as longevity and overall quality of life
[3][12][18].
2. The Shift in Social Connectedness during COVID-19
Emerging literature identified in this review confirms our previous hypotheses that: (1) the COVID-19 pandemic has compounded and worsened social isolation among older adults; and (2) the impacts of intensifying social isolation within this population have the potential to be long-lasting, with subsequent consequences for both mental and physical health outcomes. Research conducted during the early months of the pandemic and its accompanying stay-at-home orders and lockdown conditions demonstrate these impacts, with growing consensus on the key concerns escalating during this unprecedented era.
Social isolation is a well-known concern within older populations, yet its impacts on physical, psychological, and social health gained greater awareness at the onset of the COVID-19 outbreak
[19]. Since early 2020, the pandemic has truly highlighted the importance of social connections for seniors. Social isolation quickly became even more urgent as older adults lost their usual connections due to quarantine orders and social distancing recommendations designed to keep them safe. As such, a new phenomenon has occurred across this age group, as the safety protocols executed to protect older adults have subsequently placed them at greater risk of social isolation. The new concept emerging to describe this cycle resulting from social distancing efforts has become known as the COVID-19 Social Connectivity Paradox
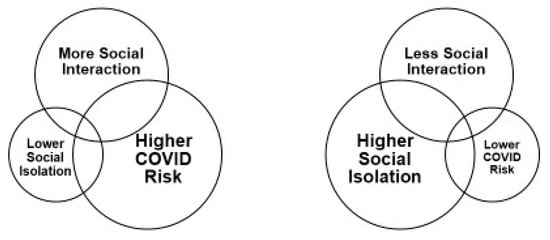
[20] ().
Figure 1. The COVID-19 Social Connectivity Paradox20.
Within this paradox, frequent interaction with others prevents social isolation, but also leads to higher risk of COVID-19 infection. Conversely, reduced interaction (due to social distancing and staying home) leads to greater isolation, yet lower risk of exposure
[20]. Compounding these factors, family members and friends of older adults often stay away and stop in-person visits to avoid exposing aging loved ones to the virus
[15][20]. The consequences of this paradox require urgent attention as it intensifies the existing problems of social isolation and disconnectedness among seniors; solutions adapted for safety are needed now and in the longer term
[20].
Another new phenomenon resulting from the pandemic has been described as “Lockdown Loneliness,” referring to loneliness specifically caused by worsening social isolation and disconnectedness due to lockdowns and stay-at-home orders
[21]. This trend is supported by June 2020 data from Great Britain suggesting that “Lockdown Loneliness” impacted 7.4 million residents at that time
[21]. Chronic loneliness remained at pre-lockdown levels (2.6 million), but among these lonely individuals, 80% were further impacted by pandemic lockdowns
[21].
At the same time, experts predict a long-term societal impact, compared to an economic low period and referred to as a “social recession,” or the long-term collapse in social contact and fraying of social bonds that could lead to worsening chronic isolation as the loss of interaction continues over time
[3][12][18]. A social recession could have lasting impacts on both physical and mental health, with serious consequences expected among the oldest and those in poor health. Unfortunately, the effects of a social recession are likely to be harder to assess and reverse than those of an economic recession.
Meanwhile, new research emphasizes the unique challenge of social isolation in long-term care settings, compounded by safety guidelines since the start of the COVID-19 outbreak. During the pandemic, infection rates and deaths among long-term care residents were initially overwhelming, with early “hot spots” of the virus in many of these facilities
[22][23][24]. Estimates from the Centers for Disease Control and Prevention (CDC) indicate that long-term care residents comprised over 25% of all COVID-19 related deaths in the US as of late 2020
[25], while in Europe and Quebec, Canada, rates appear even higher: 50% and 88%, respectively, of COVID-19 deaths have occurred in these facilities
[26][27]. Consequently, restrictions to prevent additional spread of the virus typically prohibit visits from family members and friends
[22]. At the same time, residents are often confined to their rooms inside facilities, with a sudden halt in group activities and gatherings for meals to reduce infection rates
[22]. Researchers predict that these factors will lead to significant consequences for older adults, worsening not only social isolation but also levels of loneliness, stress, anxiety, and depression, potentially further compounding physical health conditions
[22][28][29].
3. Assessing Social Isolation and the Impacts of COVID-19
As the pandemic worsened throughout 2020, fast-track research aimed to quickly examine the widespread impacts of COVID-19. Most research published prior to the end of 2020 primarily describes small survey studies and commentaries yet provides a foundation for growing knowledge
[30][31][32]. As one focus area, researchers emphasized the need to quickly assess social isolation among vulnerable seniors amid quarantines and social distancing recommendations
[30][31][32]. Experts stress that both during the pandemic and as normalcy returns, providers must regularly screen for social isolation and take proactive steps to alleviate it
[19]. In this effort, several surveys tailored with COVID-related questions have been developed in small studies. One such measure is the Questionnaire for Assessing the Impact of the COVID-19 Pandemic on Older Adults (QAICPOA), a 17-item survey
[30]. The QAICPOA was designed for use on the telephone with older participants to assess the impact of social isolation during COVID-19 and is currently freely available to use in subsequent studies. The 17 items focus on changes in social support during the pandemic, encompassing both emotional (who provides it) and instrumental (such as how food and medication is obtained while quarantined)
[30]. The QAICPOA is currently being applied in part to assess needs and barriers to connectedness, as well as to ensure referrals to resources.
Another new measure, the Fear of COVID-19 Scale (FCV-19S), is a seven-item survey designed to assess emotional, cognitive, and behavioral impacts of the pandemic. Developed for the general population, the FCV-19S uses a five-point scale with responses from strongly agree to strongly disagree, with higher scores indicating greater fear about the virus
[33]. Questions include: “I am most afraid of coronavirus-19;” “It makes me uncomfortable to think about coronavirus-19;” “My hands become clammy when I think about coronavirus-19;” and others.
Finally, the Understanding America Study (UAS) COVID-19 Survey was conducted in April–May 2020 among US adults age 50+ (
n = 3283)
[34]. This survey, funded by the National Institutes of Health (NIH), evaluated the impacts of social distancing measures primarily on loneliness. One single item asked, “In the past 7 days, how often have you felt lonely?” with responses of at least one day coded as lonely. Those who stated they were implementing social distancing measures, including cancellation of social activities and avoiding contact with others, reported up to 41% greater loneliness.
4. Growing Impacts of the Pandemic on Older Adults
Meanwhile, several small research studies have attempted to determine how the pandemic is affecting older adults’ lives, including levels of social isolation. In one study, researchers conducted an analysis of online focus group discussion data from older adults with pre-frailty or frailty while under stay-at-home orders in March 2020 (
n = 10; total posts = 60). Topics in the online posts included impacts of the pandemic on daily life, preparedness, and technology use
[11]. Participants reported increased stress, anxiety, and lack of preparedness for the crisis, along with greater feelings of social isolation due to ongoing restrictions. However, many were increasingly using technology for social connections and to find current information
[11]. Another study evaluated the impact of early COVID-19 restrictions on older adults with pre-existing depression. Telephone interviews (
n = 73) were conducted with individuals who had previously taken a survey before the pandemic related to their depression. In this follow-up survey, most participants described increasing depression, stress, anxiety, and lower quality of life (QOL), despite feeling somewhat resilient or positive at first, which authors suggested could indicate a “honeymoon” phase of resilience
[35]. Nevertheless, most also reported concerns and anxiety about the future of the pandemic and ongoing spread of COVID-19, along with continued restrictions to their routines
[35].
Similarly, an early 2020 study evaluated the short-term effects of sheltering in place
[36]. Older adults (
n = 93) had previously completed surveys on loneliness and social networks prior to the start of the pandemic as part of a mental well-being study. Then, in April and May 2020, study participants completed the same items by phone, as well as new items related to COVID-19. Most participants reported increased depression and greater loneliness following the onset of the pandemic, as compared to 6–9 months prior. In addition, loneliness positively predicted increased depression during stay-at-home orders
[36].
Another online survey evaluated perceptions of threats related to the pandemic among over 1700 adults in the US, of all ages (18–89 years)
[37]. Overall, perceptions of COVID-19 as a threat to health were high across all age groups. Notably, the greatest perceived negative impacts of the pandemic were among the oldest and associated with stress, loneliness, and poor sleep. Meanwhile, a survey conducted in July examined other potential effects of the pandemic, specifically disruptions in healthcare services among those age 65 + due to concerns about COVID-19 exposure
[38]. Participants reported disruptions to care including mental health care (69%), dental care (67%), primary care (63%), and rehabilitation (63%). Of those reporting disruptions to care during the pandemic, 35% reported the reason as fear of contracting the virus and becoming seriously ill. Over half of survey respondents were using telehealth options; of those, 95% reported satisfaction with the technology used
[38], suggesting that telehealth expansion could increase access to routine care now and in the future.
Meanwhile, perspectives are also emerging on the potential for long-term effects of the pandemic on both mental and physical health, resulting from daily lifestyle changes
[39]. For instance, reduced exercise while sheltering in place could lead to increased weakness, reduced mobility/balance, and thus higher falls risk
[39]. Shifting availability of healthy, fresh food options with older adults staying home instead of shopping frequently could have a potential impact on heart health, diabetes, and weight. In addition, the reduction in support services, caregiving, and opportunities for socialization will likely worsen loneliness, social isolation, and depression over time; fear of virus exposure has already amounted to missed preventive care appointments and procedures
[39]. Finally, authors of a recent commentary suggest that the pandemic and post-pandemic environment may present a combination of factors known to increase suicidal behaviors or ideation among isolated seniors
[40]. These factors include living alone, loneliness, and disconnectedness from society; loss of social opportunities; and reduced access to mental health resources
[40].
5. Exploring Immediate Solutions during a Pandemic
Considering the consequences of social isolation worsened by the pandemic, it is important to consider immediate outreach options. An approach being leveraged at this time focuses on volunteer phone outreach to engage older adults who are isolated at home. For example, one study described the development of a brief single-session intervention to deliver a “Connections Plan” program to engage socially isolated seniors and help them cope with social isolation during COVID-19
[32]. This study used the QAICPOA assessment along with cognitive behavioral therapy (CBT) strategies to design the intervention
[30][32]. In this approach, research clinicians work with participants remotely using strategies to cope with social isolation, by teaching various tools by phone, email, or mailed handouts. Skill building focuses on changing the individual’s perspective, actions, and body sensations to cope with feelings of isolation. Although under development at the time of this review, this approach has the potential to provide social connectedness and coping tools for seniors
[32].
Other new studies have quickly implemented telephone outreach programs to help socially isolated seniors since early 2020. One program recruited medical and healthcare student volunteers to call older adults at risk of isolation (
n = 25) during the COVID-19 crisis
[41]. The program, Seniors Overcoming Social Isolation (SOS), identified at-risk seniors through their healthcare providers, targeting both community-dwelling adults and those in long-term care facilities. Student volunteers used a script with conversation starter topics including personal history, health issues, technology use, family/friends, and COVID-19 concerns. In early results, older adult participants expressed appreciation for the calls/callers; student volunteers felt the calls were well received and also reported personal satisfaction
[41].
Another similar program was designed to address social isolation specifically among nursing home residents during the COVID-19 outbreak
[42]. The Telephone Outreach in the COVID-19 Outbreak (TOCO) program was developed to provide weekly telephone calls by medical student volunteers, with the goal of alleviating social isolation in nursing homes worsened by quarantine of residents in their rooms
[42]. Local nursing homes were contacted; at selected facilities (
n = 3 facilities), recreation directors identified at-risk residents who were willing to receive weekly phone calls (
n = 30 participants). Initial results were positive; participants reported that they looked forward to weekly phone calls with the student volunteers and expressed gratitude for the connections made with them. In fact, the student group in this study plans to continue the TOCO program beyond the pandemic to address social isolation in nursing homes
[42].
Meanwhile, other technology-based options have targeted social isolation, both prior to and during the pandemic. One recent literature review (2020) summarized the 15 smartphone applications most highly recommended as effective for addressing seniors’ needs and providing access to needed support while isolated at home
[43]. Many of these selected applications are highlighted in , although the availability of various application options continues to expand. Research indicates that seniors are increasingly using mobile technology, including smartphone applications, for healthcare purposes as well as to stay connected and access resources during this time
[43][44]. Thus, it is reasonable to consider that mobile technology could be useful for those who want to avoid leaving home while staying connected and maintaining access to healthcare services, medications, groceries, and other resources.
Table 1. Applications to Support Socially Isolated Older Adults.
| Category |
Application |
Cost |
Purpose |
| Social Networking |
Skype |
Free to download |
Individual or group phone/video calls |
| Social Networking |
FaceTime |
Free w/Apple products |
Phone and video calling |
| Telehealth |
Teladoc |
Free to download; Telehealth services depend on insurance |
Connect to a doctor by phone; Available 24/7 |
| Telehealth |
Doctor on Demand |
Free to download; Telehealth services depend on insurance |
Face-to-face digital connection with a doctor through video |
| Prescription Management |
GoodRx |
Free to download; Membership fee |
Finds Rx discounts and coupons |
| Prescription Management |
Medisafe Management |
Free to download; Membership fee |
Provides medication reminders; Drug interaction warnings |
| Cognitive Impairment |
Be My Eyes |
Free to download |
Connects visually impaired for help with tasks |
| Cognitive Impairment |
Glide Live Video |
Free to download; Subscription fee |
On-demand communication with sign language and visuals |
Health/
Fitness |
Calm |
Free to download; Subscription fee |
Mindfulness and meditation to reduce stress |
Health/
Fitness |
Headspace |
Free to download; Subscription fee |
Relaxation app with meditation techniques |
Health/
Fitness |
MyFitnessPal |
Free |
Online diet and exercise tracker |
Recent efforts are also exploring the benefits of online peer-to-peer communities for older adults, especially during this time of increased social isolation and disconnectedness. Online communities and social networks, part of the collective technological tools known as information and communication technologies (ICT), have become popular among older adults in recent years, especially since the start of the pandemic
[45]. One recent review compiled studies evaluating the effectiveness of ICT with older adults, finding that ICT had a positive impact on social support, social connectedness, and social isolation over the short term
[2]. Generally, online communities connecting older adults to their peers demonstrate success in sharing information, experiences regarding health conditions, and peer support for those with common interests
[45]. One ongoing study, which began following the onset of COVID-19 in April 2020, is exploring the feasibility of online communities for older adults as a medium to connect peers with one another and communicate with healthcare providers
[45]. Results describing whether these communities and social networks play a beneficial role in connectedness are expected in late 2021.
Finally, innovative options to address social isolation during the pandemic and beyond have been proposed. As one novel example worth mentioning, “sociable robots” have been suggested as companions for seniors who are socially isolated, even prior to the COVID-19 outbreak. Since the pandemic began, life-like sociable robots have been discussed primarily as a solution for use in COVID-19 testing and diagnosis, telemedicine, cleaning, decontamination, and monitoring of quarantine. However, some perspectives recommend the use of robots as social companions for older adults confined to their homes. Essentially, robots could function as companions in an innovative approach to reach seniors who are lonely and isolated, as well as to provide simple task-focused functions or assistance. Although this approach would present various challenges, it appears in various discussions about future directions for alleviating social isolation
[28][46][47][48]. Taken together, the commentaries and studies described here demonstrate the research quickly emerging since the start of the pandemic that could help inform solutions for supporting socially isolated older adults during a challenging time.