Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Gastroenterology & Hepatology
Gastrointestinal Stromal Tumors (GISTs) are subepithelial lesions (SELs) that commonly develop in the gastrointestinal tract. GISTs, unlike other SELs, can exhibit malignant behavior, so differential diagnosis is critical to the decision-making process. Endoscopic ultrasound (EUS) is considered the most accurate imaging method for diagnosing and differentiating SELs in the gastrointestinal tract by assessing the lesions precisely and evaluating their malignant risk.
- Gastrointestinal Stromal Tumors
- endoscopic ultrasound
- subepithelial lesions
1. Introduction
Gastrointestinal stromal tumours (GISTs) are the most common type of mesenchymal neoplasia that arises from the digestive tract [1]. Their histogenesis has been attributed to Cajal interstitial cells, which are thought to be the pacemaker cells of the gastrointestinal tract and are immunohistochemically positive for CD117 [2,3,4,5,6].
GISTs are more common in middle-aged (6th decade) males, with a prevalence of 14–20 cases per million, and are typically located in the gastric body (55.6%) or small intestine (31.8%) [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15]. In 6.0% and less than 1% of cases, the colorectum and oesophagus are involved, respectively [7,8,9,10,11,12,13,14].
GIST-related complications are characterized by gastrointestinal bleeding (including acute melena and hematemesis, as well as chronic bleeding with subsequent anaemia) caused by mass ulceration, abdominal pain, weakness, and organ compression symptoms [3,4,5,12]. However, up to 30% of GISTs are incidentally discovered in asymptomatic patients or during routine examinations. They are typically uncovered as small subepithelial lesions (SELs) that are not ulcerated, are slightly elevated, and are covered by normal mucosa. Their subepithelial origin and commonly small size hamper their differentiation from other SELs, which have slow growth and an indolent course [10,15,16,17,18,19].
The diagnosis of a GIST relies on typical cell morphology (spindle cells) and immunohistochemistry, with strong reactivity for receptor tyrosine kinase KIT or CD34. Additional tests include DOG1 staining or mutation search of the KIT or PDGFRA genes [16].
GISTs have a known malignant potential, ranging between 10% and 30% [7,8,9,10,11]. The assessment of malignant potential allows for patient stratification according to very low, low, intermediate, or high-risk cases, which is necessary for the selection of treatment strategies [11]. Although the prognosis for patients with GISTs is mainly associated with the tumour size (>2 cm) and mitotic index (< or >5/50 HPF) [12,13], small GISTs with a low mitotic index can also have a malignant course with metastasis. Other prognostic factors include the primary tumour location, tumour rupture, and metastasis.
When lesions are larger than 20 or 30 mm in diameter, surgical resection is the mainstay of treatment of localized GISTs [17]. Smaller tumours can be safely considered for endoscopic resection, with or without a laparoscopic control. However, despite complete resection, postoperative recurrence can occur in at least half of patients. Therefore, an early diagnosis is desirable [18,19,20,21,22].
Endoscopic Ultrasonography (EUS) is a crucial diagnostic technique for determining the potential malignancy of SELs, even though it is difficult to distinguish GISTs from other SELs using only EUS images [23,24]. The use of contrast agents or elastography in conjunction with EUS improves the latter’s diagnostic ability [25,26,27]. Furthermore, advances in artificial intelligence (AI) appear to have the potential to improve the accuracy of EUS for GIST diagnosis. However, although frequently controversial due to its associated technical difficulties and moderate diagnostic sensitivity, endoscopic biopsies or EUS-guided tissue acquisition (EUS-TA, including fine-needle aspiration (EUS-FNA) and fine-needle biopsy (EUS-FNB)) [28,29,30] continue to constitute the gold standard for making a definitive diagnosis.
2. Endoscopic and EUS-Based Findings
The majority of SELs are asymptomatic and detected incidentally during endoscopy performed for unrelated causes. In general, their endoscopic appearance is typically characterized by a rounded protuberance with normal overlying mucosa, negative cushion signs, and, occasionally, a central depression or umbilication [31]. When GISTs increase in size, ulceration may become apparent. Spontaneous bleeding or fibrin clotting is associated with an increased risk of malignant transformation.
Even when magnifying endoscopy or chromoendoscopy are used, SELs are extremely difficult to distinguish using solely conventional endoscopy. In general, attempts to differentiate GISTs from other SELs based on endoscopic findings have been inadequate with respect to small lesions.
According to the European Society of Gastrointestinal Endoscopy (ESGE), EUS’s ability to define the morphology and features of the suspicion of malignancy render this technique the best diagnostic tool with which to characterize these lesions. EUS images show the location, size, originating layer (the fourth layer, which corresponds to the muscolaris propria), shape, internal echo pattern, heterogeneity, and vascularity of the lesion, as well as the presence of lymph nodes adjacent to or surrounding the tumour [31,32]. Several EUS features, including irregular borders, cystic spaces, ulceration, and echogenic foci, have been linked to a higher risk of malignancy (Figure 1).
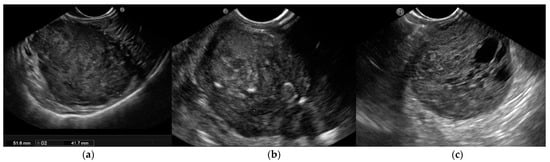
Figure 1. Endoscopic ultrasound (EUS) images of malignant gastrointestinal stromal tumors (GISTs): (a) A large submucosal lesion originating from the fourth layer of the gastric wall. Echopattern is inhomogeneous with irregular borders. (b) Another large subepithelial gastric mass with echoic foci, calcifications, and irregular profiles. (c) Cystic spaces are visible in EUS images.
Furthermore, EUS-guided techniques such as contrast enhancement, elastography, and tissue acquisition have been investigated in terms of their ability to predict diagnosis and malignant behaviour. The key issue is distinguishing GISTs from other SELs. It is especially important to guide efficient clinical therapy regarding leiomyomas because GISTs are potentially malignant, whereas leiomyomas are benign [33]. Duodenal GISTs and NETs may look similar in imaging studies, and GISTs arising from the second or third portion of the duodenum may be misdiagnosed as pancreatic NETs based solely on imaging criteria. In addition, the resection techniques differ between these two tumours. Surgical excision with regional lymph node dissection is the best treatment for pancreatic NETs. GISTs, on the other hand, are frequently treated with minimal resection and without lymph node dissection. Hence, the role of histological diagnosis is critical in determining their appropriate treatment and outcomes [31,32,33,34,35].
As SELs are located in the inner layer, with overlying normal mucosa and submucosa, the diagnostic yield of conventional endoscopic forceps-based biopsy is limited, ranging from 17% to 59%, despite the use of special devices such as the “jumbo” forceps or dedicated techniques such as the “bite-on-bite” biopsies. To address this limitation, the mucosal incision-assisted biopsy (MIAB) was developed. This technique entails lifting the mucosa that covers the SEL to make a more secure incision. The exposed lesion is sampled with biopsy forceps after an electrosurgical incision of the target mucosal and submucosal tissues with an endoscopic submucosal dissection knife [36,37,38,39,40,41].
As previously stated, EUS-based tissue acquisition, either FNA or FNB, is a viable alternative with a diagnostic rate ranging between 71% and 100%, which is strongly influenced by tumour size. The ability to perform a mitotic count, the risk of seeding, and the feasibility of the technique in specific sites were all observed to be critical issues.
Although EUS-FNB and MIAB are both recommended by ESGE guidelines, the procedure time, the size and location of the SELs, and expertise influence the choice of procedure. Tissue diagnosis is recommended for all SELs with GIST-like characteristics that are larger than 20 mm, have high-risk stigmata, or require surgical resection or oncological treatment.
3. Contrast-Enhanced Harmonic EUS
The use of contrast agents has improved the diagnostic performance of EUS, particularly with respect to differentiating GISTs from other gastrointestinal SELs [42].
Conventional EUS B-mode analysis is performed to assess the size and shape of SELs, their origin wall layer, and ultrasonographic characteristics (tissue echogenicity, calcifications, vascularization, or the presence of avascular areas using Power Doppler or hi-flow). Contrast-enhanced harmonic EUS (CH-EUS) can then visualize the microvascularization of SELs, enhancing their characterization, with hyperenhancement specific to GIST and hypo-enhancement specific to benign SELs.
When exposed to an ultrasonic wave, the contrast agents oscillate or break [42]. SonoVue (Bracco SpA, Milan, Italy) and Sonozaid (Daiichin-Sankyo, Tokyo, Japan) are contrast media that contain safe microbubbles covered by a protective lipophilic shell that carries carbon dioxide gas. In response to acoustic stimuli, these bubbles oscillate, thereby increasing the echo levels in the target tissue. During CH-EUS, the optimal amount of contrast medium is injected intravenously while the ultrasound machine is in contrast-harmonic mode. When performing CH-EUS with the SonoVue® contrast agent, a 4.8 mL bolus of SonoVue® is injected through a peripheral intravenous cannula, followed by a 10 mL saline flush [43]. Each patient’s contrast study usually lasts 90 s after the intravenous bolus injection and is documented by a video clip that includes B-mode examination and the arterial, portal, and late phases.
Contrast enhancement is typically evaluated in the early (after a few seconds) and late phases (after more than 30 s), and the enhancement patterns are then classified (as hyper-, iso-, or hypo-enhancement, and as homogeneous or inhomogeneous) along with the features (the presence or absence of regular or irregular intratumoral vessels, and the presence or absence of an unenhanced area) that can be observed after the injection of the contrast medium [44].
Pancreatic diseases are the primary application field for CH-EUS [45]. The pooled sensitivity and specificity of CE-EUS with respect to distinguishing pancreatic cancers from solid inflammatory masses were reported as 93% and 88%, respectively, in a 2017 meta-analysis [45]. Moreover, CH-EUS is also recommended for investigating pancreatic cysts, gallbladder and biliary tract lesions, lymph nodes, and SELs [46,47,48].
Several studies [31,44,49,50,51,52,53,54,55] have found CH-EUS to be useful for the characterization of GISTs. The pooled sensitivity and specificity were 89% (95%CI 82–93%) and 82% (95%CI 66–92%), respectively, in a meta-analysis [44] published in 2019 that included seven studies [49,50,51,52,53,54,55] with a total of 187 patients and assessed the value of CH-EUS towards distinguishing between GISTs and other benign SELs. One limitation of this meta-analysis was the inclusion of only two prospective studies [49,50]. The first [50], an international multicentre study, compared GISTs with leiomyoma using the CH-EUS-based characterization of 62 SELs in different locations in the upper gastrointestinal tract. Despite the small number of benign SELs discovered (5 leiomyomas vs. 57 GISTs), CH-EUS revealed hyperenhancement and avascular areas in a high percentage of GISTs but not in leiomyomas. However, the lesion size was not uniform (mean size 62.6 ± 42.1 with a range from 16 to 200), and there was a trend toward a smaller size for GISTs without avascular areas (65.8 ± 43 (16–200) vs. 39.6 ± 26.9 (22–90) p = 0.062). Moreover, there was no attempt to stratify malignant potential. In the second study, Sakamoto et al. used microvasculature evaluation with intratumoral vessel quantification (regular pattern, irregular pattern, or absence of vessels) to characterize 29 GISTs, and compared the results to histological or surgical specimen diagnosis and malignancy assessment. Similarly, many studies reported sensitivity and specificity ranging from 75% to 100% and 63% to 100%, respectively [44,49,52]. Sakamoto et al. demonstrated that an irregular intratumoral vessel pattern was an 83% accurate predictor of high-grade malignant GISTs [49] (Figure 2).
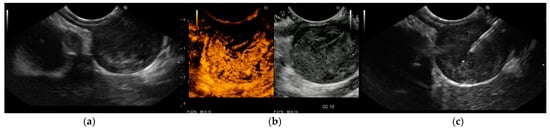
Figure 2. Endoscopic ultrasound (EUS) images of gastrointestinal stromal tumor (GIST) of the stomach: (a) The originating layer is visible when the ultrasound transducer is placed at the peripheral portion of the lesion. (b) Contrast-enhanced harmonic EUS (CH-EUS) demonstrated a hypervascular pattern. Moreover, CH-EUS allowed for the identification of irregular large vessels and avascular areas inside the tumor. (c) EUS-guided fine-needle biopsy was performed using a 22-gauge end-cutting needle while trying to avoid avascular areas previously defined using CH-EUS. Histology confirmed a GIST with a high replicative index.
According to Tamura T and Kitano M’s 2019 review, CH-EUS can distinguish between GISTs and other gastrointestinal SELs with sensitivity and specificity ranging from 78–100% and 60–100%, respectively [43].
Even though CH-EUS improves the accuracy of EUS towards SEL characterization, it cannot replace tissue acquisition for differentiating GISTs from other spindle cell neoplasms (leiomyomas), which share a “regular” vessel pattern. As a result, histology must be used to assess the malignant potential of GISTs.
4. EUS-Elastography
EUS-E is a real-time imaging technique that analyses tissue elasticity and displays this information graphically as a colour spectrum of shades [59]. While green represents average stiffness, blue represents harder tissue and red represents softer tissue. Each colour is associated with a specific value of tissue elasticity in a defined region of interest, ranging from 1 to 255 kPa [59] (Figure 3).
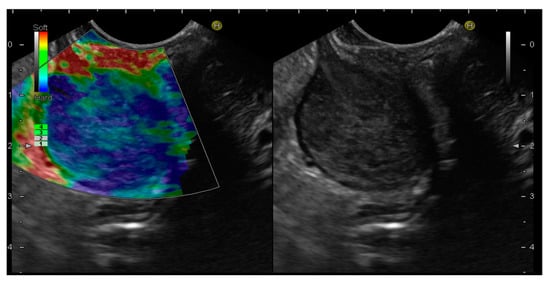
Figure 3. Endoscopic ultrasound elastography (EUS-E) images of gastrointestinal stromal tumor (GIST) of the stomach. The lesion shows a blue color, indicative of a hard tissue, compared to the red color of the gastric wall.
In addition, EUS-E compares the strain between the target and other reference areas, delivering a semi-quantitative analysis of tissue stiffness [60]. In more detail, strain ratio (SR) is a value derived from the ratio of the stiffness of two user-defined areas within an elastogram that provides an objective estimation of the lesion’s hardness [61].
Due to its lack of invasiveness, EUS-E was initially used for the differential diagnosis of SELs by providing a qualitative/semi-quantitative stiffness analysis [58,62,63,64,65,66,67,68,69,70]. EUS-E is an imaging technique that detects diseased and normal tissue elasticity changes on conventional B-mode ultrasound images [70]. The fundamental principle of EUS-E imaging is that tissues have varying elasticity, thus causing different strains when compressed by an external force or when compressed by normal breathing and blood circulation. An ultrasonic system’s software program can then characterize and visualize these strain values in real-time [71]. The elasticity values are then visually characterized in different colours on the elastography images based on tissue deformation [50,64]. Elastography is commonly used in clinical practice to diagnose diseases of the liver, thyroid, kidney, lymph nodes, prostate, mammary glands, and pancreas [34,69,72].
However, to date, only a few studies have examined the role of EUS-E in the diagnosis of SELs in the gastrointestinal tract, and the results are still debatable. The first pilot study on the efficacy of EUS-E for differentiating 25 consecutive gastric SELs demonstrated that GISTs were qualitatively harder than other SELs by rating the degree of stiffness based on the majority and colour distribution [62]. As proven by a prior study, GISTs tend to have a blue colour (61/62, 98%), which was confirmed by a subsequent study. This tendency, however, resembles that of leiomyoma (4/5, 80%) [50]. The feasibility of quantitative EUS-E based on SR with respect to the differential diagnosis of SELs has been investigated since its introduction. A preliminary retrospective study of 30 patients found that EUS-E with SR may be promising in terms of differentiating GI SELs, wherein a cut-off of 11.18 can distinguish between GISTs and leiomyomas with a sensitivity of 81.8% and a specificity of 85.7% [73]. In a prospective study by Kim et al., the SR of 41 gastric SELs was compared with the histopathologic diagnosis. GISTs presented an elevated SR (mean 51.1 ± 11.1) that enabled them to be distinguished from leiomyoma, whose SR was considerably lower (6.0 ± 6.9), with a favourable sensitivity of 100% and a specificity of 94.1% when using an SR cut-off of 22.7 [63]. The distinction of GISTs from schwannoma, a mesenchymal tumour with a similar appearance to a GIST, appears to be challenging, given that the mean SR of the only schwannoma in the series was 62.0 [32]. In a recent study, Guo et al. utilized hue histograms to quantify EUS-E images but did not find adequate evidence to support the utility of EUS-E for differentiating between GISTs and gastrointestinal leiomyomas using EUS-E [66].
This entry is adapted from the peer-reviewed paper 10.3390/cancers15041285
This entry is offline, you can click here to edit this entry!
