Primary polydipsia, or psychogenic polydipsia, is a form of polydipsia characterised by excessive fluid intake in the absence of physiological stimuli to drink. Psychogenic polydipsia which is caused by psychiatric disorders, often schizophrenia, is often accompanied by the sensation of dry mouth. Some forms of polydipsia are explicitly non-psychogenic. Primary polydipsia is a diagnosis of exclusion.
- polydipsia
- excessive fluid intake
- schizophrenia
1. Signs and Symptoms
Signs and symptoms of psychogenic polydipsia include:[1]
- Excessive thirst and xerostomia, leading to overconsumption of water
- Hyponatraemia, causing headache, muscular weakness, twitching, confusion, vomiting, irritability etc., although this is only seen in 20% – 30% of cases.[2]
- Hypervolemia, leading to oedema, hypertension and weight gain (due to the kidneys being unable to filter the excess blood)[3] in extreme episodes
- Tonic-clonic seizure[4]
- Behavioural changes, including fluid-seeking behaviour; patients have been known to seek fluids from any available source, such as toilets and shower rooms.[3][5]
The most common presenting symptom is tonic-clonic seizure, found in 80% of patients.[6] Psychogenic polydipsia should be considered a life-threatening condition, since it has been known to cause severe hyponatraemia, leading to cardiac arrest, coma and cerebral oedema.[1] It can also cause central pontine myelinolysis.
2. Brain Differences
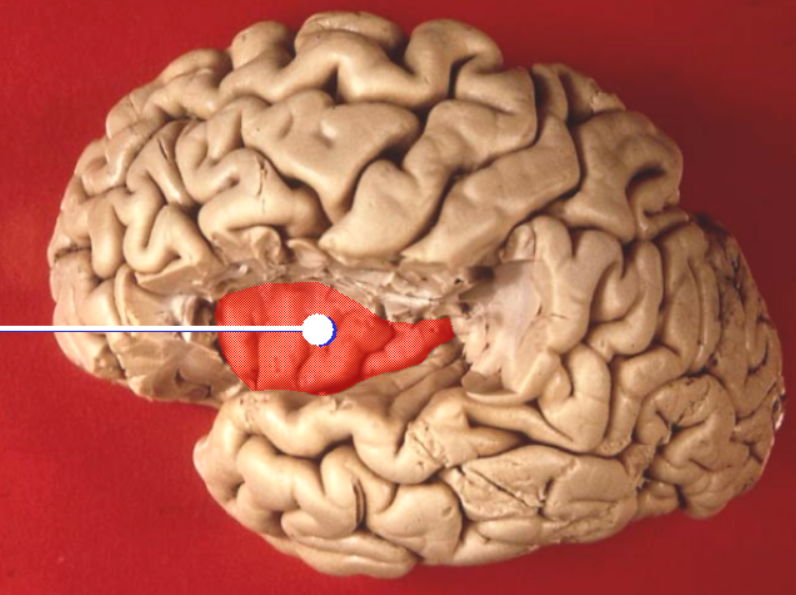
Psychogenic polydipsia in individuals with schizophrenia is associated with differences seen in neuroimaging. MRI scans may be used to help with differentiating between PPD and diabetes insipidus, such as by examining the signal of the posterior pituitary (weakened or absent in central DI).[7] Some patients, most often with a history of mental illness, show a shrunken cortex and enlarged ventricles on an MRI scan, which makes differentiation between psychogenic and physiological cause difficult.[3] However, these changes will likely only develop after chronic PPD associated with severe mental illness, as opposed to less severe forms of the disorder as seen in those with anxiety and affective disorders. PPD is also linked with significant reductions in insular cortex volume,[8] although this may be caused by the secondary hyponatraemia. It has been suggested that these deficits lead to moderate to severe cognitive impairments, especially affecting working memory, verbal memory, executive function, attention and motor speed.[9]
Other areas with volume reductions (both white and grey matter) include:[8][9]
- Right posterior lobe
- Right inferior temporal gyrus
- Parahippocampal gyrus
- Both left and right superior temporal gyri
- Right cuneus
- Left medial frontal gyryus and inferior frontal gyrus
- Right lingual gyrus
3. Diagnosis
As a diagnosis of exclusion, a diagnosis of primary polydipsia may be the result of elimination of the possibility of diseases causing similar signs and symptoms, such as diabetes insipidus.[10] Diagnosis may be complicated by the fact that chronic and extreme compulsive drinking may impair the response of the kidneys to vasopressin, thus reducing the kidney's ability to concentrate the urine.[11] This means that psychogenic polydipsia may lead to test results (e.g. in a water restriction test) consistent with diabetes insipidus or SIADH, leading to misdiagnosis.[12]
Dry mouth is often a side effect of medications used in the treatment of some mental disorders, rather than being caused by the underlying condition.[13] Such medications include antipsychotics, antidepressants, anticonvulsants, alpha agonists and anticholinergics.[14] It should also be ensured that the thirst isn't caused by diuretic use (particularly thiazide diuretics), MDMA use, excessive solute intake or chronic alcoholism. Alcoholism may cause physiological thirst since ethanol inhibits vasopressin, the hormone primarily responsible for water retention in osmoregulation.[15][16][17] The following conditions should also be excluded: DI, cerebral salt wasting, pseudohyponatraemia caused by hyperlipidemia or hyperparaproteinemia, SIADH, mineralcorticoid deficiency, salt-wasting nephropathy, nephrotic syndrome, chronic heart failure and cirrhosis.[18]
Tobacco smoking is an often overlooked factor linked to hyponatremia, due to the ADH-releasing effect of nicotine, although this is usually limited to heavy smokers.[19] One study suggested that around 70% of patients with self-induced polydipsia were tobacco smokers.[20] Diagnostic tests for primary polydipsia usually involves the fluid deprivation test to exclude ADH problems. The desmopressin test is also used, in which the synthetic hormone is used as a diagnostic workup to test for inappropriate secretion of vasopressin, as seen in DI and SIADH.
3.1. Patient Profiles
Psychogenic polydipsia is found in patients with mental illnesses, most commonly schizophrenia, but also anxiety disorders and rarely affective disorders, anorexia nervosa and personality disorders. PPD occurs in between 6% and 20% of psychiatric inpatients.[21] It may also be found in people with developmental disorders, such as those with autism.[22] While psychogenic polydipsia is usually not seen outside the population of those with serious mental disorders, it may occasionally be found among others in the absence of psychosis, although there is no existent research to document this other than anecdotal observations. Such persons typically prefer to possess bottled water that is ice-cold, consume water and other fluids at excessive levels. However, a preference for ice-cold water is also seen in diabetes insipidus.[23][24]
4. Treatment
| Weight gained (% body mass) | Estimated serum sodium (mmol/L) | Suggested intervention |
|---|---|---|
| 0-3 | 140 - 134 | No direct intervention, monitoring |
| 3-5 | 133 - 130 | Redirection from water sources |
| 5-7 | 129–126 | Oral NaCl and redirection |
| 7–10 | 125–120 | Oral NaCl and redirection, possibly restraint |
| > 10 | < 120 | Slow IV saline, seizure precautions |
Treatment for psychogenic polydipsia depends on severity and may involve behavioural and pharmacological modalities.[26]
4.1. Acute Hyponatraemia
If the patient presents with acute hyponatraemia (overhydration) caused by psychogenic polydipsia, treatment usually involves administration of intravenous hypertonic (3%) saline until the serum sodium levels stabilise to within a normal range, even if the patient becomes asymptomatic.[27]
4.2. Fluid Restriction
If the patient is institutionalised, monitoring of behaviour and serum sodium levels is necessary. In treatment-resistant polydipsic psychiatric patients, regulation in the inpatient setting can be accomplished by use of a weight-water protocol.[28] First, base-line weights must be established and correlated to serum sodium levels. Weight will normally fluctuate during the day, but as the water intake of the polydipsic goes up, the weight will naturally rise. The physician can order a stepped series of interventions as the weight rises. The correlation must be individualized with attention paid to the patient's normal weight and fluctuations, diet, comorbid disorders (such as a seizure disorder) and urinary system functioning. Progressive steps might include redirection, room restriction, and increasing levels of physical restraint with monitoring. Such plans should also include progressive increases in monitoring, as well as a level at which a serum sodium level is drawn.
4.3. Behavioural
Behavioural treatments may involve the use of a token economy to provide positive reinforcement to desirable behaviour.[26] Furthermore, cognitive therapy techniques can be used to address the thought patterns that lead to compulsive drinking behaviour. Success has been seen in trials of this technique, with emphasis on the development of coping techniques (e.g. taking small sips of water, having ice cubes instead of drinks) in addition to challenging delusions leading to excessive drinking.[29]
Psychogenic polydipsia often leads to institutionalisation of mentally ill patients, since it is difficult to manage in the community.[3] Most studies of behavioural treatments occur in institutional settings and require close monitoring of the patient and a large degree of time commitment from staff.[27]
4.4. Pharmaceutical

A number of pharmaceuticals may be used in an attempt to bring the polydipsia under control, including:
- Atypical antipsychotics, such as clozapine,[30] olanzapine and risperidone[31]
- Demeclocycline, a tetracycline antibiotic, which is effective due to the side effect of inducing nephrogenic diabetes insipidus.[27][32] Demeclocycline is used for cases of psychogenic polydipsia, including those with nocturnal enuresis (bed-wetting). Its mechanism of action involves direct inhibition of vasopressin at the DCTs, thus reducing urine concentration.[27]
There are a number of emerging pharmaceutical treatments for psychogenic polydipsia, although these need further investigation:[33]
- ACE Inhibitors, such as enalapril[34]
- Clonidine, an alpha-2 adrenergic agonist[34]
- Irbesartan, an angiotensin II receptor antagonist[31]
- Propranolol, a sympatholytic beta blocker[35]
- Vasopressin receptor antagonists, such as conivaptan[36]
- Acetazolamide, a carbonic anhydrase inhibitor[37]
Lithium was previously used for treatment of PPD as a direct competitive ADH antagonist, but is now generally avoided due to its toxic effects on the thyroid and kidneys.[27]
It is important to note that the majority of psychotropic drugs (and a good many of other classes) can cause dry mouth as a side effect, but this is not to be confused with true polydipsia in which a dangerous drop in serum sodium will be seen.[38]
5. Terminology
In diagnosis, primary polydipsia is usually categorised as:
- Psychogenic (PPD) – caused by underlying psychiatric symptoms, including those caused by psychoses and rarely by affective disorders
- Non-psychogenic – another non-psychological cause, including idiopathic (unknown cause)
The terms primary polydipsia and psychogenic polydipsia are sometimes incorrectly used interchangeably – to be considered psychogenic, the patient needs to have some other psychiatric symptoms, such as delusions involving fluid intake or other unusual behaviours. Primary polydipsia may have physiological causes, such as autoimmune hepatitis.
Since primary polydipsia is a diagnosis of exclusion, the diagnosis may be made for patients who have medically unexplained excessive thirst, and this is sometimes incorrectly referred to as psychogenic rather than primary polydipsia.[11]
6. Non-psychogenic
Although primary polydipsia is usually categorised as psychogenic, there are some rare non-psychogenic causes. An example is polydipsia found in patients with autoimmune chronic hepatitis with severely elevated globulin levels.[39] Evidence for the thirst being non-psychogenic is gained from the fact that it disappears after treatment of the underlying disease.
7. Non-human Animals
Psychogenic polydipsia is also observed in some non-human patients, such as in rats and cats.[40]
The content is sourced from: https://handwiki.org/wiki/Medicine:Primary_polydipsia
References
- Gill, Melissa; McCauley, MacDara (2015-01-21). "Psychogenic Polydipsia: The Result, or Cause of, Deteriorating Psychotic Symptoms? A Case Report of the Consequences of Water Intoxication" (in en). Case Reports in Psychiatry 2015: 846459. doi:10.1155/2015/846459. ISSN 2090-682X. PMID 25688318. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4320790
- de Leon, Jose; Verghese, Cherian; Tracy, Joseph I.; Josiassen, Richard C.; Simpson, George M. (1994). "Polydipsia and water intoxication in psychiatric patients: A review of the epidemiological literature". Biological Psychiatry 35 (6): 408–419. doi:10.1016/0006-3223(94)90008-6. PMID 8018788. https://dx.doi.org/10.1016%2F0006-3223%2894%2990008-6
- Hutcheon, Donald. "Psychogenic Polydipsia (Excessive Fluid seeking Behaviour)". http://www.apadivisions.org/division-31/publications/articles/british-columbia/psychogenic-polydipsia.pdf.
- Hedges, D.; Jeppson, K.; Whitehead, P. (2003). "Antipsychotic medication and seizures: A review". Drugs of Today 39 (7): 551–557. doi:10.1358/dot.2003.39.7.799445. PMID 12973403. https://dx.doi.org/10.1358%2Fdot.2003.39.7.799445
- Perch, Julia; O’Connor, Kevin M.. "Insatiable thirst: Managing polydipsia". Current Psychiatry 8 (7): 82. http://www.mdedge.com/currentpsychiatry/article/63646/insatiable-thirst-managing-polydipsia#bib2.
- Ferrier, I N (1985-12-07). "Water intoxication in patients with psychiatric illness.". British Medical Journal (Clinical Research Ed.) 291 (6509): 1594–1596. doi:10.1136/bmj.291.6509.1594. ISSN 0267-0623. PMID 3935199. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1418423
- Moses, A. M.; Clayton, B.; Hochhauser, L. (1992-09-01). "Use of T1-weighted MR imaging to differentiate between primary polydipsia and central diabetes insipidus." (in en). American Journal of Neuroradiology 13 (5): 1273–1277. ISSN 0195-6108. PMID 1414815. http://www.ajnr.org/content/13/5/1273.
- Nagashima, Tomohisa; Inoue, Makoto; Kitamura, Soichiro; Kiuchi, Kuniaki; Kosaka, Jun; Okada, Koji; Kishimoto, Naoko; Taoka, Toshiaki et al. (2012-01-01). "Brain structural changes and neuropsychological impairments in male polydipsic schizophrenia". BMC Psychiatry 12: 210. doi:10.1186/1471-244X-12-210. ISSN 1471-244X. PMID 23181904. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3532364
- "Polydipsia linked to brain alterations in schizophrenia". News-Medical.net. 2012-11-28. http://www.news-medical.net/news/20121128/Polydipsia-linked-to-brain-alterations-in-schizophrenia.aspx.
- "Psychogenic polydipsia – Diagnosis – Approach". British Medical Journal. 5 May 2016. http://bestpractice.bmj.com/best-practice/monograph/865/diagnosis/step-by-step.html. Retrieved 29 October 2016.
- "Primary polydipsia – General Practice Notebook". http://www.gpnotebook.co.uk/simplepage.cfm?ID=-2087059408.
- Zerbe, R. L.; Robertson, G. L. (1981-12-24). "A comparison of plasma vasopressin measurements with a standard indirect test in the differential diagnosis of polyuria". The New England Journal of Medicine 305 (26): 1539–1546. doi:10.1056/NEJM198112243052601. ISSN 0028-4793. PMID 7311993. https://dx.doi.org/10.1056%2FNEJM198112243052601
- Rippe, James M.; Irwin, Richard S. (2008). Irwin and Rippe's Intensive care medicine. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 909. ISBN 978-0-7817-9153-3.
- "Psychotropic-induced dry mouth: Don't overlook this potentially serious side effect". Current Psychiatry 10 (12): 54–58. December 2011. http://www.mdedge.com/currentpsychiatry/article/64550/depression/psychotropic-induced-dry-mouth-dont-overlook-potentially.
- Swift, R.; Davidson, D. (1998-01-01). "Alcohol hangover: mechanisms and mediators". Alcohol Health and Research World 22 (1): 54–60. ISSN 0090-838X. PMID 15706734. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=6761819
- Taivainen, H.; Laitinen, K.; Tähtelä, R.; Kilanmaa, K.; Välimäki, M. J. (1995-06-01). "Role of plasma vasopressin in changes of water balance accompanying acute alcohol intoxication". Alcoholism, Clinical and Experimental Research 19 (3): 759–762. doi:10.1111/j.1530-0277.1995.tb01579.x. ISSN 0145-6008. PMID 7573805. https://dx.doi.org/10.1111%2Fj.1530-0277.1995.tb01579.x
- Fichman, M. P.; Kleeman, C. R.; Bethune, J. E. (1970-01-01). "Inhibition of Antidiuretic Hormone Secretion by Diphenylhydantoin" (in en). Archives of Neurology 22 (1): 45–53. doi:10.1001/archneur.1970.00480190049008. ISSN 0003-9942. PMID 5409600. https://dx.doi.org/10.1001%2Farchneur.1970.00480190049008
- "Psychogenic polydipsia – Diagnosis – Differential diagnosis". British Medical Journal. 5 May 2016. http://bestpractice.bmj.com/best-practice/monograph/865/diagnosis/differential.html. Retrieved 29 October 2016.
- Blum, Alexander (1984-11-23). "The Possible Role of Tobacco Cigarette Smoking in Hyponatremia of Long-term Psychiatric Patients". JAMA: The Journal of the American Medical Association 252 (20): 2864. doi:10.1001/jama.1984.03350200050022. ISSN 0098-7484. https://dx.doi.org/10.1001%2Fjama.1984.03350200050022
- Jose, C. J.; Evenson, R. C. (1980-08-01). "Antecedents of self-induced water intoxication. A preliminary report". The Journal of Nervous and Mental Disease 168 (8): 498–500. doi:10.1097/00005053-198008000-00009. ISSN 0022-3018. PMID 7400803. https://dx.doi.org/10.1097%2F00005053-198008000-00009
- de Leon, Jose (2003-02-01). "Polydipsia—a study in a long-term psychiatric unit". European Archives of Psychiatry and Clinical Neuroscience 253 (1): 37–39. doi:10.1007/s00406-003-0403-z. ISSN 0940-1334. PMID 12664312. https://dx.doi.org/10.1007%2Fs00406-003-0403-z
- "Psychogenic polydipsia – Theory – Aetiology". British Medical Journal. 5 May 2016. http://bestpractice.bmj.com/best-practice/monograph/865/basics/aetiology.html. Retrieved 29 October 2016.
- Mayo Clinic internal medicine board review.. Ghosh, Amit., Mayo Foundation for Medical Education and Research., Mayo Clinic. (9th ed.). [Rochester, MN.]: Mayo Clinic Scientific Press. 2010. pp. 192. ISBN 9780199755691. OCLC 646395464. http://www.worldcat.org/oclc/646395464
- Assessment (Lippincott Manual Handbook). Springhouse Publishing Co. 2006. pp. 189. ISBN 978-1582559391.
- Leadbetter, Shutty Jr., Higgins, Pavalonis, Robert, Michael, Patricia, Diane (1994). "Multidisciplinary Approach to Psychosis, Intermittent Hyponatremia, and Polydipsia". Schizophrenia Bulletin 20 (2): 375–385. doi:10.1093/schbul/20.2.375. PMID 8085139. https://dx.doi.org/10.1093%2Fschbul%2F20.2.375
- Dundas, Brian; Harris, Melissa; Narasimhan, Meera (2007-07-03). "Psychogenic polydipsia review: Etiology, differential, and treatment" (in en). Current Psychiatry Reports 9 (3): 236–241. doi:10.1007/s11920-007-0025-7. ISSN 1523-3812. PMID 17521521. https://dx.doi.org/10.1007%2Fs11920-007-0025-7
- "Psychogenic polydipsia – Management – Step by step". British Medical Journal. 5 May 2016. http://bestpractice.bmj.com/best-practice/monograph/865/treatment/details.html. Retrieved 29 October 2016.
- Bowen, L.; Glynn, S. M.; Marshall, B. D.; Kurth, C. L.; Hayden, J. L. (1990-03-01). "Successful behavioral treatment of polydipsia in a schizophrenic patient". Journal of Behavior Therapy and Experimental Psychiatry 21 (1): 53–61. doi:10.1016/0005-7916(90)90049-q. ISSN 0005-7916. PMID 2373769. (Subscription content?) https://dx.doi.org/10.1016%2F0005-7916%2890%2990049-q
- Costanzo, Erin S.; Antes, Lisa M.; Christensen, Alan J. (2016-11-01). "Behavioral and medical treatment of chronic polydipsia in a patient with schizophrenia and diabetes insipidus". Psychosomatic Medicine 66 (2): 283–286. doi:10.1097/01.psy.0000116717.42624.68. ISSN 1534-7796. PMID 15039516. (Subscription content?) https://dx.doi.org/10.1097%2F01.psy.0000116717.42624.68
- Lee, H. S.; Kwon, K. Y.; Alphs, L. D.; Meltzer, H. Y. (1991-06-01). "Effect of clozapine on psychogenic polydipsia in chronic schizophrenia". Journal of Clinical Psychopharmacology 11 (3): 222–223. doi:10.1097/00004714-199106000-00022. ISSN 0271-0749. PMID 2066464. https://dx.doi.org/10.1097%2F00004714-199106000-00022
- Kruse, D.; Pantelis, C.; Rudd, R.; Quek, J.; Herbert, P.; McKinley, M. (2001-02-01). "Treatment of psychogenic polydipsia: comparison of risperidone and olanzapine, and the effects of an adjunctive angiotensin-II receptor blocking drug (irbesartan)". The Australian and New Zealand Journal of Psychiatry 35 (1): 65–68. doi:10.1046/j.1440-1614.2001.00847.x. ISSN 0004-8674. PMID 11270459. (Subscription content?) https://dx.doi.org/10.1046%2Fj.1440-1614.2001.00847.x
- Goh, Kian Peng (2004-05-15). "Management of Hyponatremia – American Family Physician". American Family Physician 69 (10): 2387–2394. http://www.aafp.org/afp/2004/0515/p2387.html. Retrieved 2016-10-29.
- "Psychogenic polydipsia – Management – Emerging treatments". British Medical Journal. 5 May 2016. http://bestpractice.bmj.com/best-practice/monograph/865/treatment/emerging.html. Retrieved 29 October 2016.
- Greendyke, Robert M.; Bernhardt, Alan J.; Tasbas, Hedy E.; Lewandowski, Kathleen S. (1998-04-01). "Polydipsia in Chronic Psychiatric Patients: Therapeutic Trials of Clonidine and Enalapril" (in en). Neuropsychopharmacology 18 (4): 272–281. doi:10.1016/S0893-133X(97)00159-0. ISSN 0893-133X. PMID 9509495. https://dx.doi.org/10.1016%2FS0893-133X%2897%2900159-0
- Shevitz, S. A.; Jameison, R. C.; Petrie, W. M.; Crook, J. E. (1980-04-01). "Compulsive water drinking treated with high dose propranolol". The Journal of Nervous and Mental Disease 168 (4): 246–248. doi:10.1097/00005053-198004000-00011. ISSN 0022-3018. PMID 7365485. https://dx.doi.org/10.1097%2F00005053-198004000-00011
- Douglas, Ivor (2006-09-01). "Hyponatremia: why it matters, how it presents, how we can manage it". Cleveland Clinic Journal of Medicine 73 Suppl 3: S4–12. doi:10.3949/ccjm.73.suppl_3.s4. ISSN 0891-1150. PMID 16970147. https://semanticscholar.org/paper/cd1f8147bc7b4d54ed6efad03eb10fe65304a919.
- Takagi, Shunsuke; Watanabe, Yutaka; Imaoka, Takefumi; Sakata, Masuhiro; Watanabe, Masako (2017-02-01). "Treatment of psychogenic polydipsia with acetazolamide: a report of 5 cases". Clinical Neuropharmacology 34 (1): 5–7. doi:10.1097/WNF.0b013e318205070b. ISSN 1537-162X. PMID 21242740. (Subscription content?) https://dx.doi.org/10.1097%2FWNF.0b013e318205070b
- Meulendijks, Didier; Mannesse, Cyndie K.; Jansen, Paul A. F.; van Marum, Rob J.; Egberts, Toine C. G. (2010-02-01). "Antipsychotic-induced hyponatraemia: a systematic review of the published evidence". Drug Safety 33 (2): 101–114. doi:10.2165/11319070-000000000-00000. ISSN 1179-1942. PMID 20082537. (Subscription content?) https://dx.doi.org/10.2165%2F11319070-000000000-00000
- "Non-psychogenic primary polydipsia in autoimmune chronic active hepatitis with severe hyperglobulinaemia". Gut 29 (4): 548–9. April 1988. doi:10.1136/gut.29.4.548. PMID 3371724. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1433532
- Falk, John L. (1969-05-01). "Conditions Producing Psychogenic Polydipsia in Animals*" (in en). Annals of the New York Academy of Sciences 157 (2): 569–593. doi:10.1111/j.1749-6632.1969.tb12908.x. ISSN 1749-6632. PMID 5255630. Bibcode: 1969NYASA.157..569F. https://dx.doi.org/10.1111%2Fj.1749-6632.1969.tb12908.x
