Diabetes mellitus (DM) is a worldwide-spread chronic metabolic disease that occurs when the pancreas fails to produce enough insulin levels or when the body fails to effectively use the secreted pancreatic insulin, eventually resulting in hyperglycemia. According to the International Diabetes Federation, in 2021, 537 million adults were suffering from DM, resulting in 6.7 million deaths and a 966 billion dollars healthcare cost. Systematic glycemic control is the only procedure at the disposal to prevent diabetes long-term complications such as cardiovascular disorders, kidney diseases, nephropathy, neuropathy, and retinopathy. The gold standard for glycemic control assessment in clinics is the glycated hemoglobin (HbA1c) measurement, but glycated albumin (GA) has recently gained more and more attention as a control biomarker thanks to its shorter lifespan and wider reliability compared to HbA1c. Continuous glucose monitoring (CGM) and blood glucose monitoring (BGM) remain useful individual tools for diabetes self-management.
- diabetes mellitus
- glycemic control
- glycated proteins
- glycated hemoglobin
- glycated albumin
1. Introduction
2. Glycated Proteins

2.1. Glycated Hemoglobin
2.2. Glycated Albumin
| Condition | Brief Explanation | Reference |
|---|---|---|
| Intensive insulin therapy | HbA1c levels change too slowly, whereas GA tracks accurately the variations induced by the therapy. | [40] |
| Fulminant type 1 diabetes mellitus | HbA1c is usually normal or only slightly elevated in this clinical condition, whereas the GA/HbA1c ratio significantly increases due to the reactiveness of GA. In this case, the GA/HbA1c is even a better indicator than GA alone. | [41][42] |
| Anemia | Hemolytic anemia shortens the lifespan of erythrocytes hence HbA1c levels are lower, whereas iron deficiency anemia produces higher levels of HbA1c due to enhanced glycation processes and longer red blood cell survivability. Albumin instead is not affected by these pathologies. | [43][44] |
| Variant hemoglobin | The genetic structural variants affect the ability of hemoglobin to be glycated, hence HbA1c does not reflect properly the glycemic status. Albumin instead is not affected by this condition. | [45] |
| Pregnancy | Towards the end of pregnancy, iron deficiency affects HbA1c levels, whereas GA levels remain stable both in diabetic and non diabetic women. | [46][47] |
| Chronic kidney disease | Erythropoietin injections, blood transfusions and hemodialysis are frequent in patients with this condition. They all affect red blood cells’ lifespan and iron values, altering HbA1c levels. Special attention has to be put on proteinuria conditions that may develop in these patients because GA values can be altered. | [48][49][50] |
This entry is adapted from the peer-reviewed paper 10.3390/bios12090687
References
- Albisser, A.M.; Leibel, B.S.; Ewart, T.G.; Davidovac, Z.; Botz, C.K.; Zingg, W.; Schipper, H.; Gander, R. Clinical Control of Diabetes by the Artificial Pancreas. Diabetes 1974, 23, 397–404.
- Nelson, C.J. A Guide to Glucose Urine Testing Systems: For the Pharmacist Teaching the Diabetic Patient. Drug Intell. Clin. Pharm. 1974, 8, 422–429.
- McArthur, R.G.; Tomm, K.M.; Leahey, M.D. Management of diabetes mellitus in children. Can. Med. Assoc. J. 1976, 114, 783–787.
- Goldstein, D.E.; Little, R.R.; Lorenz, R.A.; Malone, J.I.; Nathan, D.; Peterson, C.M.; Sacks, D.B. Tests of Glycemia in Diabetes. Diabetes Care 2004, 27, 1761–1773.
- Laffel, L. Ketone bodies: A review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab. Res. Rev. 1999, 15, 412–426.
- Clarke, W.L.; Cox, D.; Gonder-Frederick, L.A.; Carter, W.; Pohl, S.L. Evaluating Clinical Accuracy of Systems for Self-Monitoring of Blood Glucose. Diabetes Care 1987, 10, 622–628.
- American Diabetes Association. Self-Monitoring of Blood Glucose. Diabetes Care 1994, 17, 81–86.
- Walford, S.; Gale, E.; Allison, S.; Tattersall, R. SELF-MONITORING OF BLOOD-GLUCOSE: Improvement of Diabetic Control. Lancet 1978, 311, 732–735.
- Hayford, J.T.; Weydert, J.A.; Thompson, R.G. Validity of Urine Glucose Measurements for Estimating Plasma Glucose Concentration. Diabetes Care 1983, 6, 40–44.
- Morris, L.R.; McGee, J.A.; Kitabchi, A.E. Correlation Between Plasma and Urine Glucose in Diabetes. Ann. Intern. Med. 1981, 94, 469–471.
- Walford, S.; McB Page, M.; Allison, S.P. The Influence of Renal Threshold on the Interpretation of Urine Tests for Glucose in Diabetic Patients. Diabetes Care 1980, 3, 672–674.
- American Diabetes Association. Urine Glucose and Ketone Determinations. Diabetes Care 1992, 15, 38.
- The Diabetes Control and Complications Trial Research Group. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986.
- American Diabetes Association. Implications of the Diabetes Control and Complications Trial. Diabetes Care 2002, 25, s25–s27.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998, 352, 837–853.
- American Diabetes Association Professional Practice Committee. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2022. Diabetes Care 2021, 45, S83–S96.
- Thorpe, S.R.; Baynes, J.W. Maillard reaction products in tissue proteins: New products and new perspectives. Amino Acids 2003, 25, 275–281.
- Singh, V.P.; Bali, A.; Singh, N.; Jaggi, A.S. Advanced Glycation End Products and Diabetic Complications. Korean J. Physiol. Pharmacol. 2014, 18, 1–14.
- Freitas, P.A.C.; Ehlert, L.R.; Camargo, J.L. Glycated albumin: A potential biomarker in diabetes. Arch. Endocrinol. Metab. 2017, 61, 296–304.
- Kohzuma, T.; Tao, X.; Koga, M. Glycated albumin as biomarker: Evidence and its outcomes. J. Diabetes Its Complicat. 2021, 35, 108040.
- Pohanka, M. Glycated Hemoglobin and Methods for Its Point of Care Testing. Biosensors 2021, 11, 70.
- Shapiro, R.; McManus, M.J.; Zalut, C.; Bunn, H.F. Sites of nonenzymatic glycosylation of human hemoglobin A. J. Biol. Chem. 1980, 255, 3120–3127.
- Wang, S.H.; Wang, T.F.; Wu, C.H.; Chen, S.H. In-Depth Comparative Characterization of Hemoglobin Glycation in Normal and Diabetic Bloods by LC-MSMS. J. Am. Soc. Mass Spectrom. 2014, 25, 758–766.
- Shemin, D.; Rittenberg, D. The life span of the human red blood cell. J. Biol. Chem. 1946, 166, 627–636.
- Cohen, R.M.; Franco, R.S.; Khera, P.K.; Smith, E.P.; Lindsell, C.J.; Ciraolo, P.J.; Palascak, M.B.; Joiner, C.H. Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood 2008, 112, 4284–4291.
- Franco, R.S. Measurement of Red Cell Lifespan and Aging. Transfus. Med. Hemotherapy 2012, 39, 302–307.
- International Diabetes Federation. IDF Diabetes Atlas—10th edition. 2021. Available online: https://diabetesatlas.org/ (accessed on 12 April 2022).
- Koga, M.; Kasayama, S. Clinical impact of glycated albumin as another glycemic control marker. Endocr. J. 2010, 57, 751–762.
- Yoshiuchi, K.; Matsuhisa, M.; Katakami, N.; Nakatani, Y.; Sakamoto, K.; Matsuoka, T.; Umayahara, Y.; Kosugi, K.; Kaneto, H.; Yamasaki, Y.; et al. Glycated Albumin is a Better Indicator for Glucose Excursion than Glycated Hemoglobin in Type 1 and Type 2 Diabetes. Endocr. J. 2008, advpub, 0804280122.
- Murai, J.; Soga, S.; Saito, H.; Koga, M. Usefulness of glycated albumin for early detection of deterioration of glycemic control state after discharge from educational admission. Endocr. J. 2013, 60, 409–413.
- Giglio, R.V.; Lo Sasso, B.; Agnello, L.; Bivona, G.; Maniscalco, R.; Ligi, D.; Mannello, F.; Ciaccio, M. Recent Updates and Advances in the Use of Glycated Albumin for the Diagnosis and Monitoring of Diabetes and Renal, Cerebro- and Cardio-Metabolic Diseases. J. Clin. Med. 2020, 9, 3634.
- Xiong, J.Y.; Wang, J.M.; Zhao, X.L.; Yang, C.; Jiang, X.S.; Chen, Y.M.; Chen, C.Q.; Li, Z.Y. Glycated albumin as a biomarker for diagnosis of diabetes mellitus: A systematic review and meta-analysis. World J. Clin. Cases 2021, 9, 9520–9534.
- Khera, P.K.; Joiner, C.H.; Carruthers, A.; Lindsell, C.J.; Smith, E.P.; Franco, R.S.; Holmes, Y.R.; Cohen, R.M. Evidence for Interindividual Heterogeneity in the Glucose Gradient Across the Human Red Blood Cell Membrane and Its Relationship to Hemoglobin Glycation. Diabetes 2008, 57, 2445–2452.
- Anguizola, J.; Matsuda, R.; Barnaby, O.S.; Hoy, K.; Wa, C.; DeBolt, E.; Koke, M.; Hage, D.S. Review: Glycation of human serum albumin. Clin. Chim. Acta 2013, 425, 64–76.
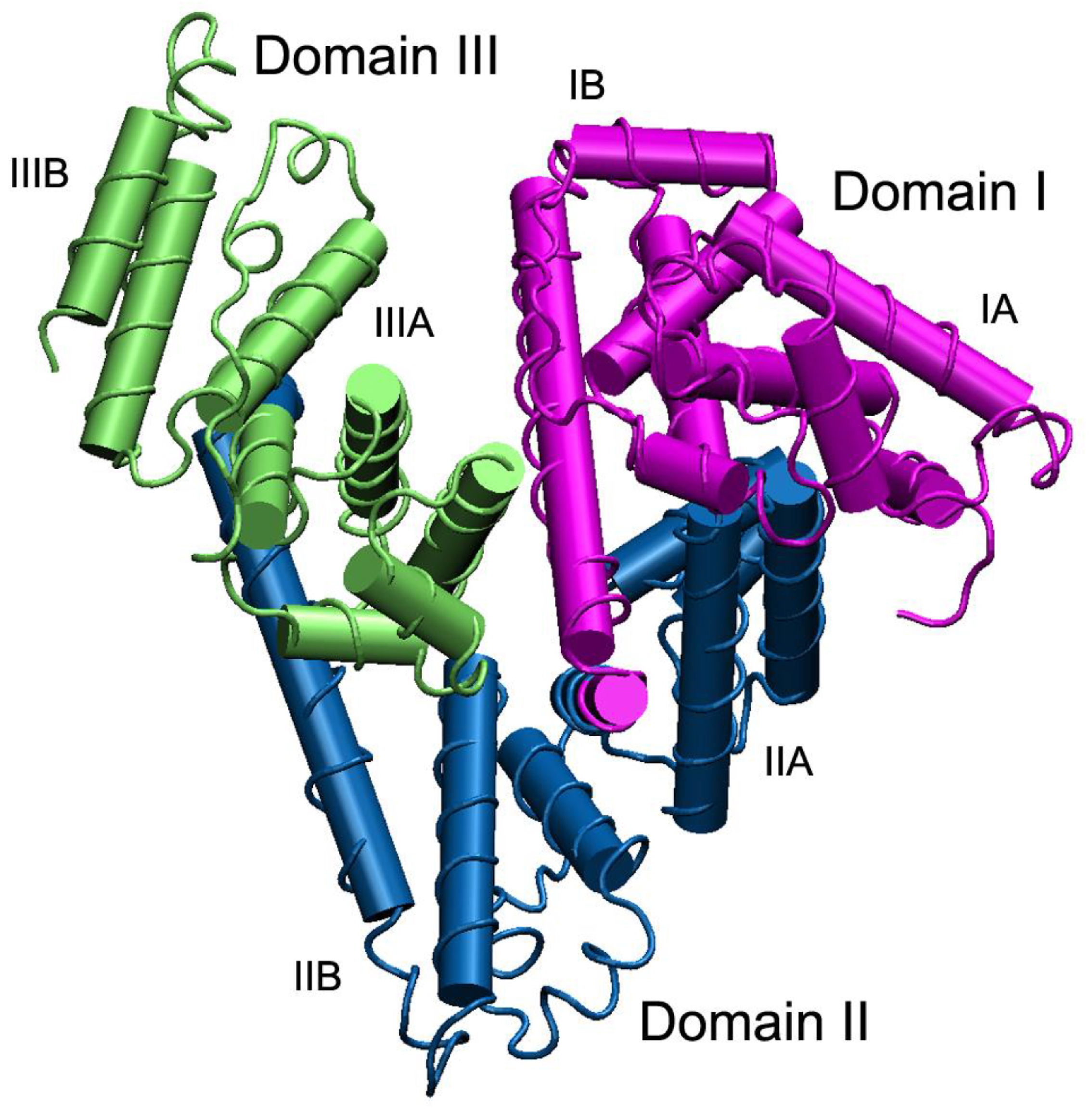
- Rabbani, G.; Ahn, S.N. Structure, enzymatic activities, glycation and therapeutic potential of human serum albumin: A natural cargo. Int. J. Biol. Macromol. 2019, 123, 979–990.
- Belinskaia, D.A.; Voronina, P.A.; Batalova, A.A.; Goncharov, N.V. Serum Albumin. Encyclopedia 2021, 1, 65–75.
- Soboleva, A.; Mavropulo-Stolyarenko, G.; Karonova, T.; Thieme, D.; Hoehenwarter, W.; Ihling, C.; Stefanov, V.; Grishina, T.; Frolov, A. Multiple Glycation Sites in Blood Plasma Proteins as an Integrated Biomarker of Type 2 Diabetes Mellitus. Int. J. Mol. Sci. 2019, 20, 2329.
- Zendjabil, M. Glycated albumin. Clin. Chim. Acta 2020, 502, 240–244.
- Suwa, T.; Ohta, A.; Matsui, T.; Koganei, R.; Kato, H.; Kawata, T.; Sada, Y.; Ishii, S.; Kondo, A.; Murakami, K.; et al. Relationship between Clinical Markers of Glycemia and Glucose Excursion Evaluated by Continuous Glucose Monitoring (CGM). Endocr. J. 2010, 57, 135–140.
- Kohzuma, T.; Koga, M. Lucica® GA-L Glycated Albumin Assay Kit. Mol. Diagn. Ther. 2010, 14, 49–51.
- Koga, M.; Murai, J.; Saito, H.; Kasayama, S.; Imagawa, A.; Hanafusa, T.; Kobayashi, T.; The Members of the Japan Diabetes Society’s Committee on Research on Type 1 Diabetes. Serum glycated albumin to haemoglobin A1C ratio can distinguish fulminant type 1 diabetes mellitus from type 2 diabetes mellitus. Ann. Clin. Biochem. 2010, 47, 313–317.
- Koga, M.; Inada, S.; Nakao, T.; Kawamori, R.; Kasayama, S. The Glycated Albumin (GA) to HbA1c Ratio Reflects Shorter-Term Glycemic Control than GA: Analysis of Patients with Fulminant Type 1 Diabetes. J. Clin. Lab. Anal. 2017, 31, e22023.
- Hellman, R. When are HBA1C Values Misleading? AACE Clin. Case Rep. 2016, 2, e377–e379.
- Silva, J.F.; Pimentel, A.L.; Camargo, J.L. Effect of iron deficiency anaemia on HbA1c levels is dependent on the degree of anaemia. Clin. Biochem. 2016, 49, 117–120.
- Bry, L.; Chen, P.C.; Sacks, D.B. Effects of Hemoglobin Variants and Chemically Modified Derivatives on Assays for Glycohemoglobin. Clin. Chem. 2001, 47, 153–163.
- Hashimoto, K.; Noguchi, S.; Morimoto, Y.; Hamada, S.; Wasada, K.; Imai, S.; Murata, Y.; Kasayama, S.; Koga, M. A1C but Not Serum Glycated Albumin Is Elevated in Late Pregnancy Owing to Iron Deficiency. Diabetes Care 2008, 31, 1945–1948.
- Hashimoto, K.; Osugi, T.; Noguchi, S.; Morimoto, Y.; Wasada, K.; Imai, S.; Waguri, M.; Toyoda, R.; Fujita, T.; Kasayama, S.; et al. A1C but Not Serum Glycated Albumin Is Elevated Because of Iron Deficiency in Late Pregnancy in Diabetic Women. Diabetes Care 2009, 33, 509–511.
- Inaba, M.; Okuno, S.; Kumeda, Y.; Yamada, S.; Imanishi, Y.; Tabata, T.; Okamura, M.; Okada, S.; Yamakawa, T.; Ishimura, E.; et al. Glycated Albumin Is a Better Glycemic Indicator than Glycated Hemoglobin Values in Hemodialysis Patients with Diabetes: Effect of Anemia and Erythropoietin Injection. J. Am. Soc. Nephrol. 2007, 18, 896–903.
- Peacock, T.; Shihabi, Z.; Bleyer, A.; Dolbare, E.; Byers, J.; Knovich, M.; Calles-Escandon, J.; Russell, G.; Freedman, B. Comparison of glycated albumin and hemoglobin A1c levels in diabetic subjects on hemodialysis. Kidney Int. 2008, 73, 1062–1068.
- Zheng, C.M.; Ma, W.Y.; Wu, C.C.; Lu, K.C. Glycated albumin in diabetic patients with chronic kidney disease. Clin. Chim. Acta 2012, 413, 1555–1561.
- Furusyo, N.; Hayashi, J. Glycated albumin and diabetes mellitus. Biochim. Biophys. Acta Gen. Subj. 2013, 1830, 5509–5514.
- Bhonsle, H.S.; Korwar, A.M.; Kote, S.S.; Golegaonkar, S.B.; Chougale, A.D.; Shaik, M.L.; Dhande, N.L.; Giri, A.P.; Shelgikar, K.M.; Boppana, R.; et al. Low Plasma Albumin Levels Are Associated with Increased Plasma Protein Glycation and HbA1c in Diabetes. J. Proteome Res. 2012, 11, 1391–1396.
- Koga, M.; Kasayama, S.; Kanehara, H.; Bando, Y. CLD (chronic liver diseases)-HbA1C as a suitable indicator for estimation of mean plasma glucose in patients with chronic liver diseases. Diabetes Res. Clin. Pract. 2008, 81, 258–262.
- Koga, M.; Murai, J.; Saito, H.; Matsumoto, S.; Kasayama, S. Effects of thyroid hormone on serum glycated albumin levels: Study on non-diabetic subjects. Diabetes Res. Clin. Pract. 2009, 84, 163–167.
- Okada, T.; Nakao, T.; Matsumoto, H.; Nagaoka, Y.; Tomaru, R.; Iwasawa, H.; Wada, T. Influence of Proteinuria on Glycated Albumin Values in Diabetic Patients with Chronic Kidney Disease. Intern. Med. 2011, 50, 23–29.
- Wang, Z.; Xing, G.; Zhang, L. Chapter Eighteen—Glycated albumin level is significantly decreased in patients suffering nephrotic syndrome. In Glycans and Glycosaminoglycans as Clinical Biomarkers and Therapeutics—Part A; Progress in Molecular Biology and Translational Science; Zhang, L., Ed.; Academic Press: Cambridge, MA, USA, 2019; Volume 162, pp. 307–319.
- Koga, M.; Matsumoto, S.; Saito, H.; Kasayama, S. Body Mass Index Negatively Influences Glycated Albumin, but not Glycated Hemoglobin, in Diabetic Patients. Endocr. J. 2006, advpub, 0605220014.
- He, X.; Mo, Y.; Ma, X.; Ying, L.; Zhu, W.; Wang, Y.; Bao, Y.; Zhou, J. Associations of body mass index with glycated albumin and glycated albumin/glycated hemoglobin A1c ratio in Chinese diabetic and non-diabetic populations. Clin. Chim. Acta 2018, 484, 117–121.
- Suzuki, S.; Koga, M.; Niizeki, N.; Furuya, A.; Takahashi, H.; Matsuo, K.; Tanahashi, Y.; Kawata, Y.; Asai, H.; Tsuchida, E.; et al. Glycated albumin is lower in infants than in adults and correlated with both age and serum albumin. Pediatr. Diabetes 2013, 14, 25–30.
- Zhou, Q.; Shi, D.B.; Lv, L.Y. The establishment of biological reference intervals of nontraditional glycemic markers in a Chinese population. J. Clin. Lab. Anal. 2017, 31, e22097.
- Bellia, C.; Zaninotto, M.; Cosma, C.; Agnello, L.; Sasso, B.L.; Bivona, G.; Plebani, M.; Ciaccio, M. Definition of the upper reference limit of glycated albumin in blood donors from Italy. Clin. Chem. Lab. Med. CCLM 2018, 56, 120–125.
- Japanese Diabetes Society. Treatment Guide for Diabetes 2016–2017. 2016. Available online: http://www.fa.kyorin.co.jp/jds/uploads/Treatment_Guide_for_Diabetes_2016-2017.pdf (accessed on 24 April 2022).
- Roohk, H.V.; Zaidi, A.R. A Review of Glycated Albumin as an Intermediate Glycation Index for Controlling Diabetes. J. Diabetes Sci. Technol. 2008, 2, 1114–1121.
