Lumbosacral traumatic injuries are reported as 39% of canine vertebral lesions. This area is prone to fracture and luxation.
- spinal fracture
- L7 fracture
- traumatic lumbosacral joint dislocation
- spine stabilization
- dog
1. Introduction
2. Canine Seventh Lumbar Vertebra Fracture
2.1. Anatomical and Biomechanical Considerations
2.2. Clinical Presentation
2.3. Imaging
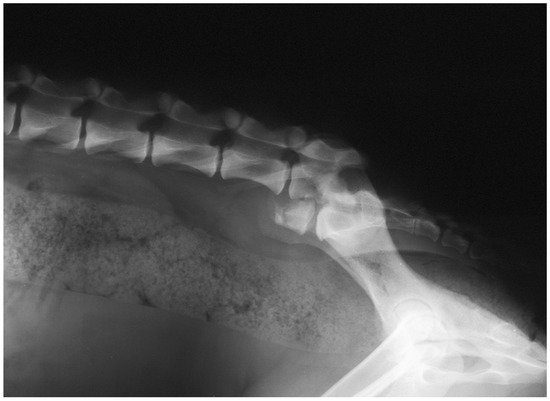
All patients with L7 fractures underwent survey radiographs in latero-lateral (LL) recumbency to confirm the diagnoses and assess the fracture or luxation [5][6][8][11][12][13][18][19][20] (Figure 1). The ventro-dorsal (VD) view was not performed for L7 fracture. In 4/38 patients, Computer Tomography (CT)-myelography was used [18].
2.4. Treatment
None of the patients with L7 fractures underwent to conservative treatment. Several surgical techniques were performed to reduce and stabilize the L7 fracture. Dulisch and colleagues, in 1981, used a double transilial pins and plastic plates to treat the L7 fracture in one patient [19]. McAnulty and colleagues in 1986 described the use of the Steinmann pins placed transversely through both ilial wings at the level of the sacral dorsal lamina, bent at a right angle, and then placed alongside the laminae and attached to the articular facets and spinous process by a stainless steel wire [8].
2.5. Complications and Prognosis
3. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/ani12020193
References
- Turner, W.D. Fractures and fracture-luxations of the lumbar spine: A retrospective study in the dog. J. Am. Anim. Hosp. Assoc. 1987, 23, 459–464.
- Selcer, R.R.; Bubb, W.J.; Walker, T.L. Management of vertebral column fractures in dogs and cats: 211 cases (1977–1985). J. Am. Vet. Med. Assoc. 1991, 198, 1965–1968.
- Jeffery, N.D. Vertebral fracture and luxation in small animals. Vet. Clin. N. Am. Small Anim. Pract. 2010, 40, 809–828.
- Bali, M.S.; Lang, J.; Jaggy, A.; Spreng, D.; Doherr, M.G.; Forterre, F. Comparative study of vertebral fractures and luxations in dogs and cats. Vet. Comp. Orthop. Traumatol. 2009, 22, 47–53.
- Di Dona, F.; Della Valle, G.; Lamagna, B.; Balestriere, C.; Murino, C.; Santangelo, B.; Lamagna, F.; Fatone, G. Percutaneous transilial pinning for treatment of seventh lumbar vertebral body fracture: A retrospective analysis of 17 cases. Vet. Comp. Orthop. Traumatol. 2016, 29, 164–169.
- Della Valle, G.; Di Dona, F.; Mennonna, G.; Lamagna, B.; Pasolini, M.P.; Caterino, C.; Lamagna, F.; Fatone, G. Traumatic lumbosacral joint dislocation in 3 dogs: Clinical presentation, diagnosis, treatment and short-term follow-up. Pak. Vet. J. 2021, 41, 97–101.
- Slocum, B.; Rudy, R.L. Fractures of the seventh lumbar vertebra in the dog. J. Am. Anim. Hosp. Assoc. 1975, 11, 167–174.
- McAnulty, J.F.; Lenehan, T.M.; Maletz, L.M. Modified Segmental Spinal Instrumentation in Repair of Spinal Fractures and Luxations in Dogs. Vet. Surg. 1986, 15, 143–149.
- Shores, A.; Nichols, C.; Rochat, M.; Fox, S.M.; Burt, G.J.; Fox, W.R. Combined Kirschner-Ehmer device and dorsal spinal plate fixation technique for caudal lumbar vertebral fractures in dogs. J. Am. Vet. Med. Assoc. 1989, 195, 335–339.
- Ullman, S.L.; Boudrieau, R.J. Internal Skeletal Fixation Using a Kirschner Apparatus for Stabilization of Fracture/Luxations of the Lumbosacral Joint in Six Dogs: A Modification of the Transilial Pin Technique. Vet. Surg. 1993, 22, 11–17.
- Harrington, M.L.; Bagley, R.S. Realignment of a Seventh Lumbar Vertebral Fracture/Luxation Using a Senn Retractor in Two Puppies. J. Am. Anim. Hosp. Assoc. 1998, 34, 377–380.
- Beaver, D.P.; MacPhersont, G.C.; Muir, P.; Johnson, K.A. Methyl-methacrylate and bone screw repair of seventh lumbar vertebral fracture-luxations in dogs. J. Small Anim. Pract. 1996, 37, 381–386.
- Weh, J.M.; Kraus, K.H. Use of a four pin and methylmethacrylate fixation in L7 and the iliac body to stabilize lumbosacral fracture-luxations: A clinical and anatomic study. Vet. Surg. 2007, 36, 775–782.
- Krauss, M.W.; Theyse, L.F.H.; Tryfonidou, M.A.; Hazewinkel, H.A.W.; Meij, B.P. Treatment of spinal fractures using Lubra plates: A retrospective clinical and radiological evaluation of 15 cases. Vet. Comp. Orthop. Traumatol. 2012, 25, 326–331.
- Hermanson, J.W.; de Lahunta, A. Spinal Cord and Meninges. In Miller’s Anatomy of the Dog, 5th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2018; pp. 589–610.
- Denis, F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin. Orthop. Relat. Res. 1984, 189, 65–76.
- Barquet, A.; Menendez, J.; Dubra, A.; Masliah, R.; Pereyra, D. Anterolateral dislocation of the lumbosacral junction. Can. Assoc. Radiol. J. 1993, 44, 129–132.
- Segal, U.; Bar, H.; Shani, J. Repair of lumbosacral fracture–luxation with bilateral twisted string-of-pearls locking plates. J. Small Anim. Pract. 2018, 59, 501–507.
- Dulisch, M.L.; Nichols, J.B. A Surgical Technique for Management of Lower Lumbar Fractures: Case Report. Vet. Surg. 1981, 10, 90–93.
- Wheeler, J.L.; Lewis, D.D.; Cross, A.R.; Sereda, C.W. Closed fluoroscopic-assisted spinal arch external skeletal fixation for the stabilization of vertebral column injuries in five dogs. Vet. Surg. 2007, 36, 442–448.
