Hepatocellular carcinoma (HCC) is a common cause of cancer-related deaths worldwide. Unlike other types of cancer, HCC can be treated with locoregional treatments (LRTs) such as radiofrequency ablation (RFA) or transarterial chemoembolization (TACE). However, recurrences following LRTs are common, and strategies to improve long-term outcomes need to be developed. The exhaustion of anti-tumor immunity in HCC has been well established in many reports and the immunomodulatory effects of LRTs (enhancement of tumor antigen-specific T cell responses after RFA, reduction of effector regulatory T cells after TACE) have also been reported in several previous studies. However, a comprehensive review of previous studies and the possible roles of immunotherapy following LRTs in HCC are not known.
1. Effects of Cell Death in Anti-Tumor Immune Responses Induced by LRTs
Several mechanisms have been suggested regarding the effects of LRTs on anti-tumor immune responses; cancer cell death caused by LRTs is closely associated with immunomodulatory effects. Both apoptosis and necrosis of tumor cells can be induced by LRTs. In general, necrosis is known to be immunogenic, because the plasma membrane is broken, and necrotic cells release cellular contents including cancer-specific antigens and DAMPs [
49]. This phenomenon augments innate and adaptive immune responses via necroinflammation [
50]. Conversely, apoptosis has been known to be non-immunogenic, because that is a process of programmed cell death, in which the plasma membrane is not disrupted [
49]. Nevertheless, previous reports have also implicated that certain types of apoptosis could be immunogenic [
49]. For example, melphalan-induced cancer cell apoptosis was associated with the secretion of proinflammatory cytokines [
51]. Additionally, the exposure of cardiac glycosides induced HMGB-1, a representative DAMP, which resulted in immunogenic cancer cell apoptosis [
52]. Thus, in addition to the type of cell death, whether LRT-related cell death is immunogenic or non-immunogenic has been investigated.
The release of tumor antigens due to cell death and subsequent changes in antigen-presenting cells (APCs) and effector immune cells are the main processes responsible for the changes in anti-tumor immune responses after LRTs [
53]. Tumor cell death caused by RFA releases tumor antigens for DCs, which induce anti-tumor immune responses [
54]. In another study, RFA induced APC infiltration and effective anti-tumor immune responses [
55].
The type of cell death might also be important in inducing an anti-tumor immune response. In a previous study, the apoptosis of tumor cells due to irradiation (not injection) of necrotic tumor cells augmented the effects of tumor cell vaccines [
56]. In another report, necrosis of tumor cells failed to induce CD8
+ T cell responses and was associated with the release of peptidases [
57]. LRTs induce tumor cell necrosis by thermal injury, but may also induce tumor cell apoptosis. For example, subtotal thermal injury in the transitional zone of RFA caused apoptosis and increased expression of heat shock protein 70, which might be associated with enhanced immunogenicity [
58]. In another study, tumor cell apoptosis was shown to be activated by RFA in the early period [
59]. Most of the tumor cells in HCC patients who underwent TACE before surgical resection were necrotic, and 11% of the tumor cells exhibited apoptosis [
60]. These findings indicated that immunogenic cell death and apoptosis could also be induced by LRTs, as well as necrosis, which is considered as non-immunogenic cell death. However, considering the high recurrence rate even after successful LRTs, a strategy to augment the anti-tumor immune responses following LRTs might also be necessary to improve tumor surveillance.
Doxorubicin, which is the most commonly used agent in TACE, can induce immunogenic cell death. The effects on cell death can differ with the types of chemotherapeutics; doxorubicin can promote immunologic cell death, but cisplatin cannot [
61]. Conversely, doxorubicin in a transplantable murine lymphoma model expanded myeloid-derived suppressor cells (MDSCs) and resulted in PD-1/PD-L1-dependent immunosuppression [
62], indicating that targeting immune checkpoint molecules following TACE with doxorubicin is helpful for effective anti-tumor responses.
2. Immunological Changes Following LRTs in HCC
Evidence regarding immunological changes based on the HCC stage is lacking; however, in the analysis of the exhausted, dysfunctional immune cells within the tumor and adjacent liver, the surgical samples used in most immunological studies were from relatively early stage HCC patients. Immune dysfunction may begin in the early stage of tumor development. In a murine model, tumor-specific T cell exhaustion was initiated at the early pre-malignant phase of tumorigenesis [
63]. In a previous study with human samples, PD-1
+-exhausted CD8
+ T cells within the tumor were also increased in patients with stage I and stage II or III HCC [
64]. Furthermore, peritumoral CD8
+ T cells exhibit exhausted features [
64]. Although further investigation is necessary, these functional and phenotypic features of T cell exhaustion caused by chronic antigenic stimulation might be restored, but do not appear fully recovered by complete antigen clearance [
65]. Thus, immune dysfunction can remain after successful LRT for HCC and LRT alone may induce limited antitumor immune responses. In the following sections, the previous studies in which the immunological changes caused by LRT in HCC were investigated are introduced and summarized in
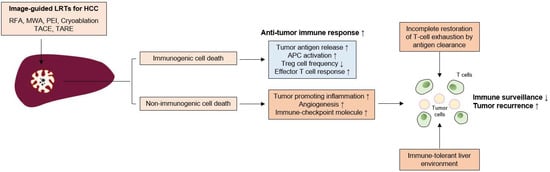
Figure 1.
Figure 1. Insufficient immune surveillance after LRTs for HCC. Image-guided locoregional treatments (LRTs) such as radiofrequency ablation (RFA), microwave ablation (MWA), percutaneous ethanol injection (PEI), cryoablation, transarterial chemoembolization (TACE), and transarterial radioembolization (TARE) cause tumor-cell necrosis or apoptosis. LRT can induce immunogenic cell death, which can be characterized by increased tumor-antigen release, antigen presenting cell (APC) activation, and decrease of regulatory T (Treg) cell frequency. These phenomena result in the augmentation of anti-tumor T cell responses and tumor surveillance. However, LRT can also induce a non-immunogenic cell death, which increases the tumor-promoting inflammation, angiogenesis, and the expression of immune checkpoint molecules. Furthermore, incomplete T cell restoration despite antigen clearance and immune-tolerant liver environment might also affect the attenuation of immune surveillance; these factors might be associated with frequent tumor recurrence even after successful LRTs for HCC.
2.1. Local Ablative Therapies
RFA is the most studied LRT in terms of immunological changes following LRTs. The immunomodulatory effect of RFA may be associated with tumor cell death caused by coagulative necrosis and apoptosis [
66]. Cryoablation also showed inflammatory and coagulative responses, which may be associated with immune activation [
67].
The increased number of tumor-specific T cells is associated with reduced tumor recurrence following RFA [
68]. Similarly, MWA also increased the peripheral T cell number and increased the Th1/Th2 cytokine ratio [
69]. A rat model of HCC showed that RFA treatment of the tumor in the left hepatic lobe enhanced T cell infiltration in the right lobe, thereby reducing tumor growth [
70]. RFA enhanced T cell trafficking to the liver, which possesses an effector function against tumor antigens, but has no effect on B cell responses [
71]. Notably, T cell activation caused by RFA tended to be stronger than that caused by surgical resection [
72]. The activation of T cells may also be associated with DC activation. In HCC patients treated with RFA or PEI, activation of myeloid DCs and increased serum levels of tumor necrosis factor-α (TNF-α) and IL-1β were observed [
73]. RFA or cryoablation also increases antigen-loaded DCs within the lymph nodes [
54]. RFA also increased Th1 cytokines (interferon-γ and TNF-α) in HCC patients, which might be associated with enhanced T cell responses [
74]. These results indicated that RFA can augment T cell infiltration into the liver and anti-tumor T cell responses in number and strength.
A 50–70% recurrence rate after successful RFA within 20–30 months has been reported in several studies [
4]. In a previous study, tumor-specific T cell responses were enhanced by RFA in a liver cancer rabbit model, including circulating T cell activation and intrahepatic T cell infiltration; however, a high recurrence rate was also observed [
75]. This finding was further validated in human subjects, which showed that immune activation following RFA was not associated with the prevention of HCC recurrence [
76]. In addition, circulating PD-L1/PD-1 expression was significantly increased after cryoablation, correlating with poor clinical outcomes [
77]. Increased Th17 cells after MWA have been shown to be a risk factor for tumor recurrence [
78]. These findings indicate that the augmentation of immune responses following RFA is insufficient to prevent tumor recurrence.
The Toll-like receptor 9 agonist CpG increased anti-tumor T cell responses following RFA and prolonged survival and reduced new tumor growth [
79]. A weak tumor-specific T cell response induced by RFA was potentiated by an anti-CTLA-4 blockade [
80]. In another study, anti-CTLA-4 blockade or Treg cell depletion after RFA or cryoablation increased tumor-specific T cell number and cytokine secretion [
54]. Interestingly, RFA of liver metastases increased T cell infiltration but also increased PD-L1 expression in primary tumors, which was overcome by anti-PD-1 blockade [
81]. Furthermore, a mouse model showed that the administration of CC chemokine ligand 3 after RFA potentiated tumor-specific T cell responses via CD11c
+cells in a CCR1-dependent manner [
82]. In addition to the activation of T cell responses, RFA reduces the frequency of MDSCs, which is associated with a better recurrence-free survival [
83]. These findings indicate that further immunotherapeutic strategies after local ablation treatments is helpful for improving clinical outcomes and enhancing tumor surveillance by effective immune responses, and strategies beyond targeting immune checkpoint molecules need to be investigated.
2.2. Transarterial Therapies
2.2.1. TACE
TACE is the preferred method for treating intermediate-stage, unresectable HCCs. Despite procedural advancement, the clinical outcome has not been satisfactory and the median OS, which is affected by tumor size, tumor markers, liver function, and vascular invasion, was 19.9 months based on a recent report [
84]. Similar to local ablative treatments, immune dysfunction may remain even after successful treatment. Furthermore, in a previous study with human samples, PD-1
+-exhausted CD8
+ T cells in the tumor were more increased in stage II or III patients than in stage I patients [
64], indicating that T-cell exhaustion is more advanced in patients receiving TACE than in patients receiving local ablation treatments. As TACE is not a curative treatment and a small number of tumor cells can remain in circulation and within the liver, surveillance and clearance by immune cells and their augmentation using ICBs could have clinical benefit [
13] and clinical trials are ongoing.
The changes in the composition or function of immune cells after TACE remain to be elucidated, and whether the peripheral T cell population might be affected by TACE has been investigated in only a few studies. Growing evidence indicates that tumor necrosis caused by TACE induces immunological activation. For example, the inflammatory cytokine IL-6 significantly increased early after TACE [
85]. However, Th2 cytokines (IL-4, IL-5, or suppressive cytokine IL-10) were also increased in the late phase after TACE, indicating that the immunological changes caused by TACE are complicated processes.
Immunologic cell death markers, such as high mobility group box 1 (HMGB1) and soluble receptor for advanced glycation end products (sRAGE), inducers of PD-L1 in tumor cells, are increased by TACE in HCC patients [
86,
87]. In a previous report, the peripheral CD4
+/CD8
+ T cell ratio was significantly lower in patients with HCC prior to TACE than in healthy volunteers and was increased 1 month after TACE [
88,
89], although its effect on anti-tumor immunity was not investigated in those studies. However, in another study, TACE increased the frequency of tumor-specific CD4
+ T cells, which was associated with improved clinical outcomes [
90]. Notably, a recent report showed that baseline PD-L1 expression within peripheral blood mononuclear cells was significantly higher in poor TACE responders, which were defined as SD or PD by RECIST criteria, and patients with high PD-L1 expression of PBMCs after TACE showed poor OS [
91]. Additionally, TACE increases PD-1 expression in peripheral mononuclear cells [
91]. These findings indicate that targeting the PD-1-PD-L1 axis might benefit the clinical outcome after TACE in terms of response rate and survival, although the effects of PD-1 expression on anti-tumor immunity before and after TACE remain unclear.
Several studies have indicated that TACE also affects Treg cells. Peripheral Treg cells were significantly increased in HCC patients and decreased by TACE [
88,
92]; their reduction was associated with improved clinical outcomes [
93]. Among Treg cells, the effector Treg population, which exerts suppressive function, was also decreased by TACE, and post-TACE frequency in this population was associated with clinical outcome [
92]. As Treg cells also highly express PD-1 in HCC patients [
94], ICBs including PD-1 or CTLA-4 inhibitors might also be beneficial for HCC patients following TACE via further Treg reduction. Taken together, partial immune reconstitution due to TACE can occur, and targeting immune checkpoint molecules and immune-suppressive components, including Treg cells, would further augment anti-tumor immune responses and tumor surveillance even after successful TACE.
2.2.2. Transarterial Radioembolization (TARE)
Transarterial radioembolization (TARE) using yttrium-90 (Y90) is an emerging option for treating locally advanced HCC that is not eligible for surgical resection. The method delivers Y90 via tumor-supplying arteries and provides tumor-restricting effects without damaging the non-malignant liver [
95], although its long-term clinical outcome has yet to be determined. Similar to TACE, TARE also activates pro-inflammatory cytokines such as IL-6 and IL-8 [
96], and baseline values of these cytokines are associated with liver function and survival [
97].
A recent in-depth analysis using CyTOF in resected HCC samples who underwent TARE before resection showed that TARE induces the activation of local immune cells, including CD8
+ T cells, CD56
+ NK cells, and CD8
+CD56
+ NKT cells [
98]. Notably, TARE also induces peripheral T-cell function and increases APCs [
98]. Furthermore, PD-1
+TIM-3
+CD8
+ T cells were observed in TARE responders, indicating that further enhancement of T cell responses might be feasible by using ICBs following TARE.
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics13091387