Patients with severe COVID-19, such as individuals in intensive care units (ICU), are exceptionally susceptible to bacterial and fungal infections. The most prevalent fungal infections are aspergillosis and candidemia. Nonetheless, other fungal species (for instance, Histoplasma spp., Rhizopus spp., Mucor spp., Cryptococcus spp.) have recently been increasingly linked to opportunistic fungal diseases in COVID-19 patients. These fungal co-infections are described with rising incidence, severe illness, and death that is associated with host immune response. Awareness of the high risks of the occurrence of fungal co-infections is crucial to downgrade any arrear in diagnosis and treatment to support the prevention of severe illness and death directly related to these infections.
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the etiologic agent of coronavirus disease 2019 (COVID-19), has infected millions of patients worldwide, and placed an unprecedented stress on healthcare systems [
1,
2,
3,
4]. This disease has predisposed a relatively high number of patients to acute respiratory distress syndrome, and co-infections are a frequent complication [
5,
6], especially with prolonged hospital stays [
7]. Changes in humans’ microbiota have been recently observed in COVID-19 patients [
1], with patients often being colonized or infected by microorganisms responsible for secondary infections (co-infections or superinfections), often caused by bacteria and fungal pathogens [
5,
7,
8,
9]. Indeed, several opportunistic infections following severe respiratory viral infections have been recognized in COVID-19 patients [
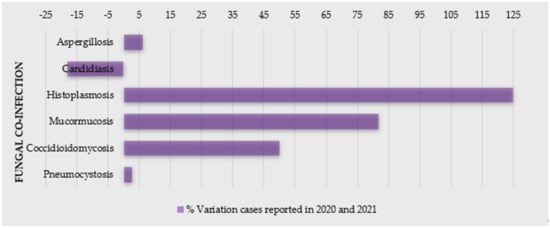
2]—particularly, a higher incidence of fungal co-infections (
Figure 1) [
10,
11,
12]. For example, in Spain, the incidence of candidemia cases was higher in the first and second waves and lower during the third wave, also with a prevalence of invasive pulmonary aspergillosis (IPA) cases [
11]. Moreover, the coronavirus-associated pulmonary aspergillosis (CAPA) showed to affect up to 30% of ventilated patients with COVID-19 admitted in intensive care units (ICU) [
13], and, in a hospital in Pisa (Italy), 21.9% of 315 hospitalized patients with COVID-19 had a superinfection [
14].
Figure 1. Percentage of variation of cases of COVID-19 patients with fungal co-infections reported in 2020 and 2021 (source: PubMed).
The main pathogens related to co-infections are reported to be Enterobacterales (44.9%), non-fermenting Gram-negative bacilli (15.6%), Gram-positive bacteria (15.6%), and fungi (5.5%) [
14]. In COVID-19 patients, the most fungi related to co-infections are
Aspergillus spp.,
Candida albicans, Candida glabrata,
Candida dubliniensis,
Candida parapsilosis sensu stricto,
Candida tropicalis, and
Candida krusei (Pichia kudriavzevii) [
8]. Moreover, these cases have been indicated as mainly primary and catheter-related infections [
15].
There is still lack of information regarding the long-term impact of secondary infections on the outcome of hospitalized COVID-19 patients [
9,
16]. Patients with co-infection undergoing invasive mechanical ventilation showed to be 3.8 times more likely to die than those without positive cultures [
9]. In order to perform an efficient treatment and reduce mortality, it is important to make an accurate early identification [
12]; however, these co-infections raise difficulties on diagnosis, treatment (including broad-spectrum antimicrobial drugs, mechanical ventilation, extracorporeal membrane oxygenation), prognosis, and even increase the disease the symptoms and mortality of COVID-19 [
8,
12,
15,
17,
18,
19].
The repercussions of SARS-CoV-2 infections on future global antimicrobial resistance must be explored profoundly [
3,
16]. In Valencia (Spain), the antifungal consumption increased in 2020 compared to previous year, especially echinocandins, voriconazole, and isavuconazole [
11]. Considering that the antimicrobials drugs for COVID-19 patients, both on and during admission, are almost all prescribed uncertainly in clinical settings, there is expected an increase in drug-resistant infections [
3].
Lastly, considering the immune response, there has been represented a host dysregulation triggered by SARS-CoV-2 infection, which has been hypothesized as a causal pathway for the increasingly reported mainly fungal (oral) manifestations associated with COVID-19 [
20,
21]. Additionally, the alteration in human microbiota (due to SARS-CoV-2 infection), which can also indicate the progression of COVID-19, may contribute to bacterial, fungal, or viral infections and affect the immune system [
1]. In these patients, this is normally described as an increase in pro-inflammatory markers, such as IL-1, IL-6, and tumor necrosis alpha (TNF-α), less CD4 interferon-gamma expression, and a decreased number of CD4 and CD8 cells, which increase susceptibility to bacterial and fungal infections [
12].
2. Fungal Infections as a Co-Morbidity of COVID-19
Fungal co-infections are frequent in the COVID-19 patients; therefore, its awareness is important for proper diagnosis and, subsequently, efficient treatment of the fungal co-infections for reducing morbidity and mortality. Due to a general neglected approach towards fungal tropical diseases, morbidity and mortality is expected to worsen in the context of the COVID-19 pandemic [
22]. SARS related to COVID-19 disease is known to increase the risk of invasive fungal infections (IFI) [
23,
24]. In addition, patients suffering from endemic mycoses and COVID-19 co-infection seem to be an at-risk population and have a poor prognosis. A significant number of cases of COVID-19-associated candidiasis, aspergillosis, mucormycosis, and histoplasmosis have been reported so far from the different region of the world [
22,
25,
26,
27]. Some reports even state that COVID-19 increases the mortality rate in the patients having fungal infections, but the case reports suggest that individuals with COVID-19 are more susceptible to a fungal infection mostly because of impaired immune responses, which further increases the awareness of clinicians for more effective diagnosis and treatment [
28,
29].
2.1. Candidiasis
One of the major complications of severe COVID-19 cases are yeast infections. They are mainly caused primarily by
Candida spp., which are associated with a high mortality rate, due to a longer ICU stay, catheterization, and broad-spectrum antibiotic use [
6] (
Table 1). Nucci et al. observed stable incidence of candidemia in their hospital during an 18-year period (1.3 episodes per 1000 admissions), but since March 2020, an increase in cases diagnosed with candidemia was noticed [
30]. Compared with non-COVID-19 patients, COVID-19 patients with candidemia were more likely to be under mechanical ventilation [
30]. Katz et al. evaluated the association between COVID-19 and oral and systemic candidiasis [
25]. Generally, candidiasis was significantly associated with increased risk for COVID-19, whereas oral candidiasis showed an insignificant trend [
25].
Table 1. Clinical characteristics of COVID-19 patients reported with candidiasis.
| Fungal Infection in COVID-19 Infection |
Observed Immune
Response |
Co-Morbidity/
Disease Models |
Test/Diagnosis Performed |
COVID-19
Treatment |
Antifungals Used |
Steroids? |
Outcome after Treatment |
References |
Candidemia
Candida duobushaemulonii
Candida parapsilosis, Candida lusitaniae |
Elevated
pro-inflammatory markers (d-dimer, ferritin, CRP, progressive
thrombocytosis) and neutrophilia |
Acute pulmonary
embolism
with subarachnoid hemorrhage
superimposed bacterial pneumonia |
CT scan, Culture,
RT-PCR
Blood, urine, and
DTA |
Meropenem,
Levofloxacin
Trimethoprim/sulfamethoxazole,
Amikacin, tigecycline,
colistin |
Intravenous
fluconazole |
NR |
Dead |
[32] |
Candidemia
(Candida glabrata) |
Leucocytes—normal,
C-reactive protein and interleukin 6—altered |
Type-2 diabetes
ischemic heart disease
stadium IV, leg amputation highly suspected bacterial superinfection |
Chest X-ray and CT scan, RT-PCR, serology,
MALDI-TOF |
Darunavir/ritonavir,
HCQ,
piperacillin/tazobactam,
teicoplanin,
ertapenem,
colistin |
Caspofungin |
NR |
Dead |
[39] |
Candidemia
Candida auris (n = 10),
Candida albicans (n = 3), Candida tropicalis (n = 1), Candida krusei (P. kudriavzevii) (n = 1) |
NA |
Underlying chronic conditions (e.g., hypertension, n = 7; DM, n = 6; and chronic kidney and liver disease, n = 2) |
MALDI-TOF and molecular identification—sequencing |
NR |
Micafungin |
NR |
Dead (n = 8) |
[4] |
Candidemia
Candida auris
(n = 3) |
NA |
DM,
hypertension, chronic renal
failure, coronary artery
disease, obesity |
Vitek 2 system,
MALDI-TOF, sequencing,
multiplex PCR |
NR |
Anidulafungin |
NR |
Dead |
[36] |
Candidemia
Candida auris
(n = 12) |
NA |
DM (n = 6), hypertension (n = 6), multiple myeloma (n = 1),
stem cell transplantation (n = 1), dyslipidemia (n = 1), end stage renal disease (n = 1), bladder cancer (n = 1), obesity (n = 1), systematic lupus erythematosus (n = 1) |
PCR,
MALDI-TOF,
Vitek2,
whole genome sequencing |
Remdesivir (n = 9), HCQ (n = 1), |
Amphotericin B
Micafungin, |
n = 10 |
Dead (n = 6)
Alive (n = 6) |
[40] |
Both fungi and virus display highly distinctive patterns of sudden emergence, and are based on simple infection-driven, human-to-human transmission [
31]. In times of SARS-CoV-2, the vigilance of multidrug-resistant
Candida spp. (e.g.,
Candida auris,
C. glabrata, and
Candida duobushaemulonii [
17,
32,
33]) is extremely important. Data regarding multidrug-resistant
Candida spp. in COVID-19 patients are scarce [
32].
C. auris, an emerging pathogen known for a reduced susceptibility to antifungals, is spread across all continents [
5], and it is easily transmitted between healthcare professionals. Both
C. auris and SARS-CoV-2 have been found on hospital surfaces including on bedrails, intravenous (IV) poles, beds, air conditioner ducts, windows, and hospital floors [
5]. Hospital-acquired
C. auris infections in coronavirus disease patients may lead to adverse outcomes and additional strain on healthcare resources [
34]. Moreover, the standard COVID-19 critical care of using mechanical ventilation and protracted ventilator-assisted management makes these patients potentially susceptible to colonization and infections by
C. auris [
5]. For example, during April–July 2020 in New Delhi (India),
C. auris accounted for two-thirds of cases, and the case-fatality rate was very high (60%) [
4]. In a phylogenetic molecular clock study (Genoa, Italy), Di Pilato and colleagues showed that all
C. auris isolates were resistant to amphotericin B, voriconazole, and fluconazole at a high level, owing to mutations in
ERG11 (K143R) and
TACB1 (A640V) genes. Critically,
C. auris could be easily spread because of the COVID-19 pandemic [
35]. After the first
C. auris-colonized case was diagnosed in a COVID-19 patient in ICU at a hospital in Salvador, Brazil, a multidisciplinary team conducted a local
C. auris prevalence investigation [
36]. Remarkably, findings revealed that among body swabs collected from 47 patients, eight samples from the axillae were positive for
C. auris. Contaminated axillary monitoring thermometer helped to
C. auris dissemination. Re-use of these devices must imply a careful disinfection or they should be replaced by other temperature monitoring methods [
36]. Moreover, in 2020, the Florida Department of Health was alerted to three
C. auris bloodstream infections and one urinary tract infection (UTI) in four patients with COVID-19 who had received care in the same COVID-19 ICU ward [
37]. A report from in a tertiary academic center (United States, May 2014 to October 2020) showed that in an entire sample (non-COVID-19 and COVID-19 groups),
C. albicans accounted for a minority of isolates collected [
38]. Compared to non-COVID-19 patients with candidemia, COVID-19 patients had lower ICU admission sequential organ failure assessment score, but longer ICU stays and central venous catheter dwell times at candidemia detection [
38].
Surveillance data assessed differences in candidemia patients with and without a prior COVID-19 diagnosis [
28]. COVID-19 patients with candidemia lacked established underlying conditions associated with candidemia but had two times the mortality rate versus candidemia patients without COVID-19 [
28]. Over a two-year period, patients followed in the ICU of Ankara City Hospital, Turkey, were divided into pre-pandemic and pandemic periods [
29]. In multivariate logistic regression analysis, corticosteroid use, presence of sepsis, and age older than 65 years were independent risk factors for mortality in candidemia patients [
29]. Indeed, candidemia with high mortality is reported as a more serious problem for COVID-19 patients due to its increased and earlier incidence, and a higher rate of mortality [
28,
29].
2.2. Aspergillosis
Aspergillosis is one of the most common opportunistic fungal co-infections caused by some
Aspergillus spp., which particularly affects immunocompromised persons, such as COVID-19 patients. It critically affects the respiratory system, leading to a mild/serious lung infection, known as pulmonary aspergillosis, a serious form of aspergillosis, which becomes worse over time and does not have an effective treatment [
26,
41]. Clinical characteristics of the COVID-19 patients co-infected with aspergillosis can be analyzed in
Table 2. Based on the available literature, it is suggested to keep a low threshold to investigate for COVID-19 associated pulmonary aspergillosis (CAPA), since an early detection and respective treatment may significantly improve outcomes. Moreover, prolonged courses of steroids should not be given unless further conclusive evidence is available [
42], because steroids suppress the immune system, making the patient more susceptible to secondary infections. A rapid and aggressive treatment approach with judicious use of steroids while treating co-infections turns out to be the best possible outcome and solution.
Table 2. Clinical characteristics of COVID-19 patients reported with aspergillosis.
| Fungal Infection in COVID-19 Infection |
Observed Immune Response |
Co-morbidity/
DiseaseModels |
Test/Diagnosis Performed |
COVID-19 Treatment |
Antifungals Used |
Steroids? |
Outcome after Treatment |
References |
Aspergillosis
Aspergillus spp., CAPA |
Highly permissive inflammatory response |
DM, CVD |
CT scan, Culture |
HCQ |
Azoles, liposomal amphotericin B |
NR |
Alive |
[43] |
| Immunocompromised |
ARD, HT |
CT scan, RT-PCR, Culture, ELISA |
NR |
Voriconazole |
Yes
(n = 7) |
Some alive and some dead |
[44] |
Aspergillosis
Aspergillus fumigatus, CAPA |
Immunocompromised |
DM, HT |
CT scan, Culture |
NR |
Isavuconazole, voriconazole |
No |
Alive |
[42] |
| HT, coronary heart disease, obesity |
CT scan, RT-PCR, Culture, |
HCQ, meropenem, azithromycin |
Voriconazole |
Yes |
Dead |
[26] |
| Low B-cell and T-cell response |
Severe dyspnea, hypertension, DM |
CT scan, RT-PCR, Serology |
RD, multiple antibiotics |
Multiple antifungals |
No |
Alive |
[45] |
| Systemic pro-inflammatory cytokine responses |
Asthma, DM, Myeloma |
CT scan, RT-PCR, Culture, |
NR |
Voriconazole, isavuconazole, liposomal amphotericin B, caspofungin, anidulafungin |
Yes |
Some alive and some dead |
[46] |
| High inflammatory response and immunosuppression |
ALL, AML |
RT-PCR, CT scan, Culture, Serology |
NR |
Caspofungin, fluconazole, liposomal amphotericin B, caspofungin, itraconazole |
No |
Some alive and some dead |
[47] |
Aspergillosis
Aspergillus spp., IA |
Acquired immunodeficiency and immunosuppression |
ARD |
Antigen, CT scan, Culture, Serology |
NR |
NR |
Yes |
Death
(quick evolution) |
[48] |
| Strong deregulation of core components of innate immune and inflammatory responses |
RHAEM |
NA |
NA |
NA |
NA |
NR |
[49] |
2.3. Histoplasmosis
Histoplasmosis is a systemic mycosis, highly endemic in certain regions of America and Asia, including Brazil and India. It is caused by a dimorphic fungus,
Histoplasma capsulatum, which predominately occurs in soil containing large amounts of bird or bat droppings. The infection occurs through the inhalation of fungal microconidia after perturbation of these environmental sources [
50]. Similarly to aspergillosis, the disease is usually associated with immunosuppressive conditions, clinically presenting severe acute disseminated forms. Underlying lung disorders can predispose individuals to chronic pulmonary histoplasmosis, whereas acute and subacute pulmonary forms mainly occur in healthy individuals after a large fungal inoculum inhalation [
50,
51]. These clinical forms are less known, often misdiagnosed as bacterial pneumonia and pulmonary tuberculosis (
Table 3). In the case of this particular fungal disease, it was indicated that most patients who received steroids for COVID-19 treatment developed histoplasmosis (
Table 3). Histoplasmosis is mainly associated with COVID-19 patients with AIDS, and there are very few studies on the co-infection of
H. capsulatum and COVID-19 [
27,
52]. Actually, the important findings were all patients of COVID-19 having co-infection of
H. capsulatum survived after antifungal treatment with amphotericin B and itraconazole (
Table 3) [
27,
52,
53,
54,
55].
Table 3. Clinical characteristics of COVID-19 patients reported with histoplasmosis.
| Fungal Infection in COVID-19 Infection |
Observed Immune Response |
Co-morbidity/
Disease
Models |
Test/Diagnosis Performed |
COVID-19 Treatment |
Antifungals Used |
Steroids? |
Outcome after Treatment |
References |
Histoplasmosis
Histoplasma capsulatum |
Acquired immunodeficiency |
HIV |
CT-scan,
RT-PCR |
Tenofovir/lamivudine and atazanavir/ritonavir
ceftriaxone, azithromycin |
Itraconazole |
Yes
(dexamethasone) |
Alive |
[27,52] |
| HIV |
HIV |
CT-scan,
RT-PCR |
Atazanavir/ritonavir, tenofovir/emtricitabine |
Itraconazole,
amphotericin B deoxycholate |
No |
Alive |
[27] |
| Inflammatory response |
NA |
CT-scan,
RT-PCR |
Levofloxacin |
Itraconazole |
Yes
(methylprednisolone) |
Alive |
[53] |
| NA |
NA |
CT scan,
RT-PCR |
NA |
Itraconazole |
No |
Alive |
[54] |
Histoplasmosis
Histoplasma capsulatum-like intracellular yeasts |
Acquired immunodeficiency |
HIV |
CT-scan,
RT-PCR |
HCQ, lopinavir/ritonavir, tenofovir disoproxil fumarate/emtricitabine plus dolutegravir |
Amphotericin B deoxycholate,
itraconazole |
No |
Lost to follow-up |
[55] |
2.4. Mucormycosis
The presence of hyphal infiltration of sinus tissue and a temporal course of less than four weeks defines mucormycosis [
56,
57]. The most common species related to mucormycosis are
Rhizopus spp. and
Mucor spp., but recently, a new
Cunninghamella species,
Cunninghamella bigelovii, was described [
58]. Clinically, rhino-cerebral mucormycosis (RCM) can have atypical symptoms and signs that are similar to complicated sinusitis, such as crusting, nasal blockage, facial pain, proptosis and chemosis, edema, ptosis, and even ophthalmoplegia, as well as fever and headache and symptoms of intracranial extension [
59,
60]. A black eschar can be found on the hard palate or in the nasal cavity, but it is not typical [
61,
62]. Mycotic infiltration of blood vessels, thrombosis with vasculitis, acute neutrophilic infiltrate, bleeding, and tissue infarction are all histological characteristics [
63].
Without early treatment and identification, this illness may advance quickly, with reported death rates of 50–80%, due to intra-orbital and cerebral complications. Even with timely treatment of underlying illnesses, diagnosis, and surgical intervention, therapy is frequently ineffective, resulting in infection spread and eventually death [
64].
Recently, there has been a shift in the occurrence of sinus mucormycosis infection, and patients have been identified more often. A dramatic increase in cases of invasive fungal sinusitis, especially mucormycosis, has occurred in the past months, with many patients needing drastic surgical operations to treat this illness [
65,
66]. The use of steroids to control COVID-19 may be directly related to the suppression in immunity; thus, it also allows the colonization of opportunistic fungi, leading to mucormycosis, during any stages of the disease (
Table 4) [
23].
Table 4. Clinical characteristics of COVID-19 patients reported with mucormycosis.
Co-Morbidity/
DiseaseModels |
Test/Diagnosis Performed |
COVID-19 Treatment |
Antifungals Used |
Steroids? |
Outcome after Treatment |
References |
Obesity
HT |
CT-scan,
RT-PCR |
None mentioned |
Linezolid, meropenem |
NA |
Died |
[67] |
Asthma
HT
DM |
CT-scan,
RT-PCR |
Remdesivir |
Amphotericin B |
NA |
Died |
[68] |
DM
Vascular disease |
CT-scan,
RT-PCR |
Tocilizumab, methylprednisolone, dexamethasone |
Amphotericin B |
Methylprednisolone, dexamethasone |
Died |
[69] |
| HT |
CT-scan,
RT-PCR |
Hydrocortisone |
Amphotericin B |
Hydrocortisone |
Died |
[70] |
| NA |
CT-scan,
RT-PCR |
Remdesivir, tocilizumad, dexamethasone |
Amphotericin B |
Dexamethasone |
Died |
[71] |
Asthma
HT
DM |
CT-scan,
RT-PCR |
Remdesivir, dexamethasone |
Amphotericin B |
Dexamethasone |
Died |
[72] |
| HT |
CT-scan,
RT-PCR |
HCQ, lopinavir–ritonavir |
Amphotericin B |
NA |
Died |
[73] |
DM
ICM
RD |
CT-scan,
RT-PCR |
Meropenem |
Amphotericin B |
Dexamethasone |
Alive |
[74] |
| DM |
CT-scan,
RT-PCR |
NA |
Amphotericin B |
NA |
Alive |
[75] |
HT,
DM |
CT-scan,
RT-PCR |
NA |
Liposomal amphotericin B, itraconazole |
NA |
Alive |
[76] |
| NA |
RT-PCR
CT-scan |
Remdesivir, dexamethasone, metformin, glipizide |
Amphotericin B, ceftriaxone |
Dexamethasone |
Live |
[77] |
| DM |
CT-scan,
RT-PCR |
Meropenem, oseltamivir
tocilizumab, sitagliptin/metformin |
Amphotericin B |
Methylprednisolone,
dexamethasone |
Died |
[69] |
| DM |
CT-scan,
RT-PCR |
Remdesivir, ceftriaxone, azithromycin, dexamethasone |
Voriconazole, liposomal amphotericin B |
Dexamethasone |
Live |
[78] |
DM (1 patient)
No co-morbidity (1 patient) |
CT-scan |
Remdesivir, convalescent plasma,
vancomycin, piperacillin-tazobactam |
Amphotericin B |
NA |
Live (n = 1)
Died n = (1) |
[68] |
Obesity
DM |
CT-scan,
RT-PCR |
Amoxicillin-clavulanate,
imipenem/linezolid |
Amphotericin B |
NA |
Died |
[79] |
DM (n = 8)
CRF (n = 3) |
CT-scan |
Broad-spectrum antibiotics |
Liposomal amphotericin B |
Dexamethasone |
Died (n = 7)
Alive (n = 4) |
[80] |
DM
HT
(all patients) |
RT-PCR |
HCQ,
glucocorticoids |
Systemic antifungals |
Glucocorticoids |
Died (n = 7)
Live (n = 8) |
[81] |
T2DM (4)
T2DM with HT (1)
HT (1)
Kidney Disease (1) |
CT-scan,
RT-PCR |
Tocilizumab, prednisolone,
piperacillin/tazobac, linezolid |
Voriconazole |
Prednisolone |
Died (n = 3)
Alive (n = 4) |
[82] |
DM (21-cases)
HT (14-cases)
Renal failure (1-case) |
CT-scan,
RT-PCR |
HCQ, azithromycin |
Caspofungin |
Combination of steroids |
All Live |
[76] |
| DM (16) |
RT-PCR |
Corticosteroids |
Liposomal amphotericin B, voriconazole,
posaconazole |
On Steroid |
Alive (n = 10)
Died n = (6) |
[83] |
HT,
UTI |
CT-scan,
RT-PCR |
Either
dexamethasone or
methylprednisolone (7 patients); interferon (2 patient);
remdesivir (1 patient);
flavipiravir and HCQ (1 patient) |
Amphotericin B, posaconazole |
Dexamethasone or
Methylprednisolone
(n = 7) |
Live |
[84] |
| DM |
RT-PCR
CT-scan |
Remdesivir, levofloxacin, dexamethasone, meropenem, vancomycin, piperacillin/tazobactam |
Amphotericin B, posaconazole |
Dexamethasone |
Live |
[85] |
| No co-morbidity |
CT-scan,
RT-PCR |
HCQ |
Amphotericin B |
NA |
Died |
[86] |
chronic lymphocytic leukemia
DM |
RT-PCR |
NA |
Amphotericin B |
NA |
Died |
[87] |
DM
HT
asthma |
RT-PCR |
NA |
Amphotericin B |
No |
Died |
[88] |
| AML |
CT-scan,
RT-PCR |
HCQ
lopinavir-ritonavir |
Amphotericin B |
NA |
Died |
[73] |
| renal disease |
CT-scan,
RT-PCR |
Remdesivir, vancomycin, cefepime |
Liposomal amphotericin B, posaconazole |
Dexamethasone |
Died |
[72] |
ICM
HF s/p OHT DM
HT
CKD |
RT-PCR |
Remdesivir
methylprednisolone |
Fluconazole |
Methylprednisolone,
dexamethasone |
Died |
[89] |
| No history of any co-morbidity |
CT-scan,
RT-PCR |
Tocilizumab |
Liposomal amphotericin B, posaconazole, isavuconazole |
Dexamethasone |
Live |
[90] |
DM
HT |
|
Piperacillin/tazobactam, HCQ, azithromycinlopin, vir/ritonavir, prednisone
Dexamethasone |
Liposomal amphotericin B, isavuconazole, posaconazole |
Prednisone, Dexamethasone |
Live |
[91] |
| HT |
RT-PCR |
Remdesivir, dexamethasone |
Amphotericin B |
Dexamethasone |
Died |
[92] |
T2DM
(all 6 patients) |
CT-scan,
RT-PCR |
Prednisolone, dexamethasone, methylprednisolone |
Amphotericin B, posaconazole |
Prednisolone,
Dexamethasone,
methylprednisolone |
All
Live |
[93] |
DM
HT |
CT-scan,
RT-PCR |
Remdesivir, interferon-alpha |
Systemic antifungals |
Systemic corticosteroid |
Died |
[94] |
T2DM, HT (2)
T2DM (3) |
CT-scan,
RT-PCR |
Tocilizumab,
convalescent plasma,
methylprednisolone |
Liposomal amphotericin B,
posaconazole |
Methylprednisolone |
Died (n = 2)
Alive (n = 3) |
[95] |
| T1DM |
CT-scan,
RT-PCR |
Ceftriaxone, azithromycin,
dexamethasone,
remdesivir,
tocilizumab |
Amphotericin B |
Dexamethasone |
Live |
[71] |
Obesity
hypothyroidism |
CT-scan,
RT-PCR |
HCQ, remdesivir, vancomycin, meropenem |
Liposomal amphotericin B,
posaconazole |
Prednisone |
Died |
[96] |
HT
Asthma |
RT-PCR |
Meropenem, remdesivir, dexamethasone |
Liposomal amphotericin B |
Dexamethasone, prednisolone |
Died |
[97] |
2.5. Cryptococcus
Cryptococcus neoformans is also related to a very serious opportunistic infection in immunocompromised patients. It has been reported that
C. neoformans can infect COVID-19 patients. Mohamad Y et al. described the importance of early suspicion of
C. neoformans infections in patients with immunocompromised state, considering that Cryptococci patients have a high risk of mortality [
98]. In the current perspective, the use of immunosuppressive drugs should be justified and to be alert for infections such as
C. neoformans, which can cause sepsis and mortality [
98]. Studies have shown that almost all patients with COVID-19 having co-infection of
C. neoformans did not survive, even after treatment with fluconazole and amphotericin B (
Table 5).
Table 5. Clinical characteristics of COVID-19 patients reported with cryptococcosis and other fungal infections.
| Fungal Infection in COVID-19 Infection |
Observed Immune Response |
Co-morbidity/
Disease
Models |
Test/Diagnosis Performed |
COVID-19 Treatment |
Antifungals Used |
Steroids? |
Outcome after Treatment |
References |
| Cryptococcus neoformans |
High inflammatory response and immunosuppression |
HAT, HBV |
CT-scan,
RT-PCR |
meropenem, vancomycin |
Fluconazole |
Yes
(tacrolimus, prednisone) |
Death |
[102] |
| Acquired immunodeficiency and immunosuppression |
HIV |
CT-scan,
RT-PCR |
Tenofovir-DF/
Emtricitabine-atazanavir/ritonavir |
Amphotericin B deoxycholate plus fluconazole |
No |
Death |
[103] |
| High inflammatory response and immunosuppression |
Stage IV prostate cancer
HT, colon-sigma diverticulosis |
CT-scan |
No |
Fluconazole
Amphotericin B plus flucytosine |
Dexamethasone |
Death |
[104] |
| High inflammatory response and immunosuppression |
HT, DM |
NA
but COVID19 positive mentioned |
Tocilizumab and corticosteroids |
Anidulafungin,
Amphotericin,
flucytosine |
Methylprednisolone |
Death |
[98] |
| Coccidioidomycosis (Coccidioides immitis, C. posadasii) |
Impaired cytokine signaling from CD4+ Th1 and cytotoxic CD8+ T-cells among patients |
No associated respiratory symptoms & disease |
CT scan, Culture, Serology |
NR |
Liposomal Amphotericin B |
No |
Alive |
[105] |
| Coccidioidomycosis (Coccidioides immitis) |
Depressed cellular immunity |
Progressive respiratory symptoms, hypoxemia |
CT scan, Culture, |
Remdesivir |
Fluconazole |
No |
Alive |
[106] |
| Pneumocystis jirovecii |
Cytokine release storm |
RA |
CT scan, Culture, Serology |
HCQ, Tocilizumab |
Caspofungin, ganciclovir, cefoperazone |
Glucocorticoids |
NR |
[107] |
| Functional immune suppression related to CD4+ lymphocytopenia |
HIV, progressive hypoxemia |
RT-PCR, Culture, Serology, CT |
NR |
Trimethoprim- sulfamethoxazole |
NR |
NR |
[108] |
| Immunocompromised |
ARD, DM, HT |
RT-PCR, Culture, Serology, |
HCQ, Lopinavir-ritonavir |
Antifungals and antibacterials |
Yes |
Some alive and some dead |
[109] |
| Low CD4 count (35.6%) |
HIV |
CT, RT-PCR, Multiplex PCR |
NR |
Co-trimoxazole and oral prednisolone |
No |
Alive |
[110] |
| Anemia, lymphopenia, raised C-reactive protein, immunosuppression |
HIV |
CT, RT-PCR |
NR |
Co-trimoxazole, IV pentamidine |
No |
Death |
[111] |
| Severe depletion of CD4+ cells |
HIV |
RT-PCR, Culture, CT |
Emtricitabine, Ritonavir |
Trimethoprim-sulfamethoxazole |
No |
NR |
[99] |
| Immunocompetent patient |
Recovered from COVID-19 |
RT-PCR, Culture, CT |
Enoxaparin, ceftaroline |
Trimethoprim-sulfamethoxazole, methylprednisolone |
Yes |
Alive |
[100] |
| Immunocompromised patients |
HT, hepatic steatosis, massive lung thromboses |
RT-PCR, Culture, CT, Histopathology |
Remdesivir |
Trimethoprim-sulfamethoxazole, prednisone |
Yes |
Some alive and some dead |
[101] |
Saccharomyces cerevisiae (boulardii)
(n = 2) |
Immunosuppression |
HT (first)
Diabetes (Second) |
RT-PCR |
Oseltamivir
HCQ |
Anidulafungin,
fluconazole |
No
treated with Ultra-Levure [preparation of Saccharomyces cerevisiae (boulardii)] |
Both live |
[112] |
| Fusarium proliferatum |
immunocompetent diabetic patient |
HAT
substituted hypothyroidism |
RT-PCR |
No |
Amphotericin B
caspofungin |
No |
Live |
[113] |
2.6. Other Fungal Infections
Some other types of fungal infections have also been reported along with COVID-19. This is the case of
Coccidioides immitis and
Pneumocystis jirovecii (
Table 5). Although co-infection with
P. jirovecii is considered life-threatening, according to recent publications, patients improved clinically when treated with common drugs, such as trimethoprim–sulfamethoxazole [
99,
100]. Similarly to the other cases, during these co-infections, steroids had a negative impact on COVID-19-associated fungal co-infections conditions [
100,
101].
This entry is adapted from the peer-reviewed paper 10.3390/jof7090720