Chronic lymphocytic leukemia (CLL) is an extremely heterogeneous disease. With the advent of oral targeted agents (Tas) the treatment of CLL has undergone a revolution, which has been accompanied by an improvement in patient’s survival and quality of life.
- chronic lymphocytic leukemia
- prognosis
- targeted therapy
1. Introduction
Chronic lymphocytic leukemia (CLL) is the most frequent chronic leukemia in Western countries. The diagnosis is usually incidental in a routine blood test and its outcome is extremely heterogeneous. Some patients present with a rapidly progressive evolution, while others remain at an indolent state for the rest of their lives. Antitumor therapy is only required if active disease is documented, according to the International Workshop on Chronic Lymphocytic Leukemia (iwCLL) criteria [1]. Furthermore, response to treatment is also variable and may be predicted by different biomarkers. This is of vital importance at this time, in which treatment algorithms have drastically changed and chemoimmunotherapy (CIT) has been replaced by targeted agents (Tas) for most patients [2,3]. Research is moving ahead at a staggering speed and, consequently, the therapeutic arsenal is growing. Oral targeted treatments approved and available worldwide are: ibrutinib, the first generation of Bruton Tirosine Kinase inhibitors (BTKi); idelalisib, the first generation of phosphatidyl-inositol 3-kinase inhibitors (PI3Ki); and venetoclax (BCL-2 inhibitor). The European Medicine Agency (EMA) has just approved acalabrutinib, a second class BTKi. The second class PI3Ki, duvelisib is also available in some countries. Other second class BTKi (zanubrutinib), PI3Ki (umbralisib) or new reversible, non-covalent BTKi (pirtobrutinib, ARQ 531) are under investigation and will hopefully be available soon [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18]. Therefore, the identification of prognostic and predictive biomarkers is relevant, not only for patient counseling but also for planning follow-up or selecting treatment at a time where a shift towards personalized medicine is taking place. Table S1 summarizes the names and principal characteristics of clinical trials with TAs and CIT in CLL mentioned throughout this review.
The difference between the terms prognostic and predictive biomarker has been previously addressed in depth [19,20]. In brief, prognostic biomarkers separate groups of patients with different outcomes regardless of treatment. On the contrary, a predictive biomarker provides information about the possible benefit of a specific treatment and can be used in the clinical decision-making process [21]. Many of the most powerful prognostic and predictive biomarkers were identified in the CIT era [22,23,24,25,26,27,28] but the validity of most of them has been evaluated also with oral Tas [6,11,12,29,30,31].
Although individual factors can be a very important prognostic tool, reality is more complex, as each patient may harbor several biomarkers with different prognostic value. To overcome this issue, prognostic scores have been developed integrating biomarkers into models. The Rai and Binet systems, proposed almost half a century ago, were the pioneers and, despite their limitations, they are still in force today [32,33]. Since then, various prognostic models and nomograms were proposed that can be applied at different moments during the course of the disease. The most established today is the CLL-International Prognostic Index (CLL-IPI), which has demonstrated its ability to predict overall survival (OS), time to first therapy (TTFT) and progression-free survival (PFS) in the CIT setting [34,35]. It has also shown to predict TTFT in early-stage CLL [36] and community-based cohorts of patients [37,38]. However, its utility to predict PFS and even OS in patients treated with Tas is limited [39]. Thus, other models have recently emerged to evaluate prognosis in this setting [40,41].
2. Prognostic Biomarkers: All That Glitters Is Not Gold
Over the last 50 years, plenty of biomarkers with ability to predict CLL evolution were identified. The most relevant, classified by categories, are illustrated in Figure 1.
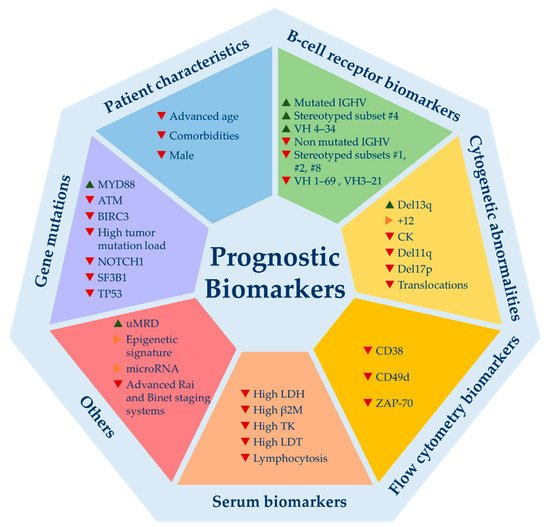
Figure 1. Relevant prognostic biomarkers for chronic lymphocytic leukemia. Del13q = 13q deletion; +12 = trisomy 12; CK = complex karyotype; del11q = 11q deletion; del17p = 17p deletion; LDH = lactate dehydrogenase levels; β2M = beta-2-microglobulin levels; TK = thymidine kinase; LDT = lymphocyte doubling time; uMRD = undetectable minimal residual disease. ▲ indicates good prognosis; ▶ indicates good and bad prognosis or intermediate prognosis; ▼ indicates poor prognosis.
Even though they emerged in the era of CIT, most are valid today, since they are capable to predict time to first treatment (TTFT), which is not influenced by the choice of therapy [22,23,24,25,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65]. The mutational status of immunoglobulin heavy chain variable region (IGHV) gene, cytogenetic abnormalities detected by FISH, CD49d expression and TP53 mutations are the biomarkers that have been consolidated as the most powerful ones and are supported by the best scientific evidence [50,66]. Others such as ZAP-70 and CD-38 have lost their strength, although their prognostic value is unquestionable. These flow cytometry biomarkers may be useful if IGHV mutation status is not available, as they act as surrogate markers. Among B-cell receptor biomarkers, a selective usage of IGHV genes in CLL has been described, with an overuse of certain genes. Some of these gene usages have been associated with clinical outcome such as VH1-69, VH3-21 (bad outcome) or VH 4-34 (good outcome) [67,68,69,70]. In addition, almost a third of CLL patients express stereotyped B cell receptor immunoglobulins (BcR IG). Some of these subsets also harbor prognostic value highlighting subsets #1, #2, #8 (bad prognosis) and #4 (good prognosis) [63,71]. Recently, a single point mutation in IGLV3-21 (R110-mutated IGLV3-21) has been studied, identifying an aggressive biological subtype of CLL [72].
Recurrent gene mutations identified by next generation whole exome or whole genome sequencing carry important prognostic information [61,73,74]. However, its implementation in routine practice has not been fully recommended to date, with the exception of TP53 mutation [1]. A great variety of mutations have been identified, but only a few occur in more than ~5% of the patients. Among them stand out NOTCH1, SF3B1, ATM, BIRC3, POT1 and MYD88. All but MYD88 have been associated with adverse outcome and other poor prognostic biomarkers [75]. Some patient-related and tumor-load variables such as age, comorbidities, beta-2-microglobulin levels (B2M), lymphocytosis or lymphocyte doubling time (LDT) are available in virtually all patients and remain valid in predicting TTFT [76,77]. Novel markers such as complex karyotype (CK), stereotyped subsets, micro-RNAs or epigenetic subsets need more evidence to be used in the routine setting. Finally, minimal residual disease (MRD) is one of the strongest predictors of PFS and OS in CLL patients treated with CIT [78]. Indeed, undetectable MRD (uMRD) is considered a surrogate marker for PFS in the context of clinical trials. Regarding targeted treatments, BTKi or PI3Ki obtain very long PFS despite their low rates of complete responses (CR) and uMRD. Therefore, uMRD is not a valid prognostic biomarker for patients treated with BTK or PI3K inhibitors [5,6,11,12,13]. Conversely, venetoclax-based regimens induce high rates of uMRD enabling a fixed-duration treatment which has established uMRD as a therapeutic goal for these combinations. Moreover, the prognostic value of achieving uMRD with venetoclax has been demonstrated, not only in the relapsed/refractory (R/R) setting but also as a frontline treatment (Murano and CLL14 phase 3 trials) [10,31]. Combos of novel agents (TA) between them +/− anti-CD20 monoclonal antibodies or, less frequently, with CIT is what immediate future holds. Preliminary results of trials using these combinations are impressive with the highest rates of uMRD ever seen (>50–70%), which might turn uMRD as the most powerful biomarker to predict prognosis in CLL patients that require treatment [79,80,81,82,83]. In fact, it could be used to guide treatment decisions in the near future by helping to decide when to stop or intensify therapy. Nevertheless, questions such as how to proceed with MRD results after a fixed duration schedule (stop, continue or change treatment) remain open. In summary, despite this large amount of biomarkers, not all have been externally and prospectively validated and, furthermore, few are valuable for clinical decision-making.
(References would be added automatically after the entry is online)
This entry is adapted from the peer-reviewed paper 10.3390/cancers13081782
