Parvovirus B19, a member of the Parvoviridae family, is a human pathogenic virus. It can be transmitted by respiratory secretions, hand-to-mouth contact, blood transfusion, or transplacental transmission. Most patients are asymptomatic or present with mild symptoms such as erythema infectiosum, especially in children. In rare cases, moderate-to-severe symptoms may occur, affecting blood cells and other systems, resulting in anemia, thrombocytopenia, and neutropenia. Non-immune pregnant women are at risk for fetal infection by parvovirus B19, with greater complications if transmission occurs in the first or second trimester. Infected fetuses may not show any abnormalities in most cases, but in more severe cases, there may be severe fetal anemia, hydrops, and even pregnancy loss.
1. Maternal Infection—Clinical Presentation
Parvovirus B19 infection may be asymptomatic or may present with prodromal symptoms only. In some cases, the prodrome is followed by a subsequent phase with more specific symptoms, while in other cases, as in immunosuppressed or high-risk individuals, the infection may progress to a chronic form associated with long-term complications and sequelae [
19,
20]. However, parvovirus infection can be asymptomatic in more than 50% of non-pregnant women and almost 30–50% of pregnant women, respectively [
21].
The incubation period varies from 4 to 14 days after exposure but can last up to 3 weeks. EI is the most classic sign of the disease and is more common in children. It is characterized by a “slapped face” appearance with a maculopapular rash on the face and/or trunk and extremities, which may present as a reticular rash [
19,
20].
The clinical course and immune response to parvovirus B19 is biphasic, with a second phase of symptoms presenting with rash, pruritus, or arthralgia approximately 17 to 18 days after vaccination [
22,
23]. Peripheral polyarthropathy of the hands, wrists, and knees is also characteristic and may be the only manifestation in pregnant women [
24]. Polyarthropathy affects up to 50% of pregnant women and can last for several weeks to months [
25]. More severe cases may result in aplastic crisis, this condition usually being self-limiting, and it is common in individuals with underlying chronic anemia such as sickle cell disease, HIV infection, and other inherited or acquired immunodeficiencies [
26,
27]. Parvovirus B19 IgG-positive individuals are generally considered immune to recurrent infection, but reinfection is possible [
17].
Aplastic crisis is defined as a reticulocyte count below 50% of the baseline for at least two consecutive weeks. This event, although rare, is more common in patients who already have some form of chronic anemia (sickle cell, thalassemia, etc.). The main hypothesis for this outcome is that parvovirus particles are cytotoxic to erythrocyte precursor cells in the bone marrow. In addition, in patients with chronic anemia, the number of erythrocyte progenitor cells in the bone marrow is higher, which may facilitate the replication of B19 and explain the higher viremia observed in these patients during the acute phase of aplastic crisis. Aplastic crisis does not seem to be associated with gender or the presence of a rash [
20].
2. Intrauterine Infection
2.1. Transmission
The rate of transmission of maternal parvovirus B19 infection to the fetus ranges from 17% to 33% [
28], with an increased risk of transmission between 9 and 20 weeks of gestation, and most fetuses show spontaneous resolution of the infection without adverse perinatal outcomes [
29,
30]. Only acute parvovirus B19 infection may place the fetus at risk for anemia and hydrops [
31].
2.2. Pathophysiology
Parvovirus B19 is not teratogenic, unlike viruses like rubella. However, fetal tissues—including hematopoietic cells in the liver, myocardium, endothelial cells, platelets, megakaryocytes, and fibroblasts—express the viral P antigen receptor, explaining the variety of fetal signs, especially anemia and hydrops [
32].
The fetal liver is the primary hematopoietic organ from 9 to 24 weeks of gestation. The second trimester also sees the most rapid increase in the mass of fetal red blood cells, which increases more than 30-fold in number. However, the half-life of fetal red blood cells produced in this period is relatively short, approximately 45–70 days [
33]. Therefore, the fetus is extremely vulnerable to any pause in red blood cell production during the second trimester and is more susceptible to the changes caused by parvovirus B19 [
34]. This risk is greatly reduced in the third trimester when fetal hematopoiesis migrates to the bone marrow, and red blood cell lifespan increases.
2.3. Effects of Infection on Pregnancy
Pregnancy does not appear to affect the course of the parvovirus B19 infection, but the infection can affect the pregnancy and especially the fetus, as described below:
- (1)
-
Spontaneous abortion: The rate of spontaneous abortion decreases with gestational age at diagnosis, with a rate of 13% before 20 weeks’ gestation and 0.5% after 20 weeks’ gestation [
28,
30]. The reason for this difference remains unclear, but the largest study suggests that it may be related to multiple organ damage, which can occur in the absence of anemia or hydrops, the most classic findings associated with fetal infection [
6].
- (2)
-
Non-immune hydrops: The most obvious manifestation of congenital parvovirus B19 infection is fetal hydrops. The risk of hydrops is directly related to the gestational age when maternal infection occurs. If the infection occurs in the first trimester, the risk of hydrops varies from less than 5% to about 10%. If the infection occurs between 13 and 20 weeks, the risk of hydrops drops to 5% or less. If the infection occurs after 20 weeks’ gestation, the risk of fetal hydrops is 1% or less [
8,
18,
25].
Fetal ultrasound signs associated with hydrops include ascites, skin edema, pleural and pericardial effusions, and placental edema. Possible mechanisms for the development of hydrops are (1) fetal anemia due to the virus crossing the placenta and infecting erythrocyte precursors in the fetal bone marrow, associated with a shorter fetal erythrocyte half-life (especially during the hepatic stage of hematopoiesis), contributing to severe anemia, hypoxia, and high-output heart failure; (2) fetal viral myocarditis resulting in heart failure and impaired liver function due to direct damage to hepatocytes and indirect damage from hemosiderin deposition [
25,
28,
30]. Spontaneous improvement of fetal hydrops may occur in approximately 34% of cases by the time of delivery [
35].
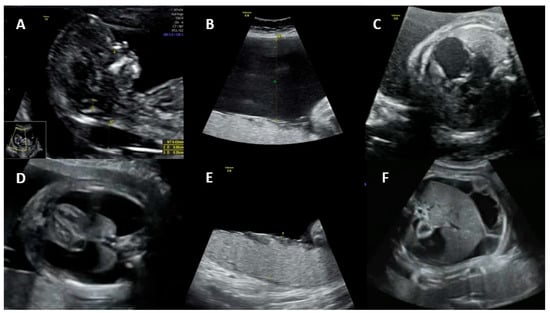
Figure 1 shows the main ultrasonographic findings of intrauterine parvovirus B19 infection.
Figure 1. Main ultrasonographic findings of intrauterine parvovirus B19 infection: (A) increased nuchal translucency, (B) polyhydramnios, (C) cardiomegaly, (D) pleural effusion, (E) placentomegaly, and (F) ascites.
Thrombocytopenia has been reported in up to 97% of transfused hydropic fetuses, with an incidence of severe thrombocytopenia (<50 × 10
9 platelets/L) of up to 46% [
6,
35].
3. Maternal Diagnosis
Systematic screening for parvovirus B19 infection is not recommended, and diagnostic testing is reserved for women with high suspicion of acute infection or known exposure [
38,
39]. Laboratory diagnosis of parvovirus B19 infection during pregnancy is mainly based on IgG and IgM antibody detection tests. The detection rate of infection remains around 80–90% when using radioimmunoassay (RIA) tests to capture antibodies or enzyme-linked immunosorbent assay (ELISA) [
40].
IgM antibodies are detected early, by the end of the first week of infection [
41], and can persist for approximately 140 days. IgG antibodies, as markers of past infections, can become positive a few days after IgM and remain positive for years [
27]. Patients with IgG-positive, IgM-negative serologic test results indicate previous viral exposure and possibly immunity, suggesting that they will unlikely contract the disease in future. [
27,
39,
42]. Caution should be exercised in interpreting the absence of positive IgM from 8 to 12 weeks after acute infection because of the possibility of rapid IgM clearance and false-negative results.
In cases where both parvovirus B19 IgM and IgG serologies are negative, it is assumed that the pregnant woman has not been exposed to the virus and is therefore susceptible to infection. In non-immune pregnant women recently exposed to the virus, the viral incubation period should be considered, and serology should be repeated two to four months after exposure, also considering polymerase chain reaction (PCR) [
38,
39,
42,
43].
Both positive IgG and IgM serologies may represent a recent infection or a late infection of up to 6 months. To differentiate between the two hypotheses, it is recommended to repeat the serology and compare the IgG titers, since they will be increasing in case of a recent infection [
39,
43]. Another possibility is IgM positivity only, suggesting a very recent infection, or even a false-positive result. IgG positivity on repeated serology one to two weeks after the initial test confirms a recent infection [
39,
42].
PCR assays for parvovirus B19 have high specificity for acute primary infection but have a short window of positivity, which limits their use in practice. Viremia occurs between 5 and 10 days after exposure and usually persists for about 7 days, a period that often precedes the onset of symptoms and serologic positivity [
39]. In asymptomatic patients, because the day of infection is unknown, this test cannot be used as a gold standard [
41]. The use of these tests may be useful in certain situations, for example to achieve maximum diagnostic sensitivity in patients with a history of recent exposure to parvovirus B19 and negative initial serologies [
39]. Although not necessary to detect acute maternal infection, other techniques such as electron microscopy, viral DNA detection, and nucleic acid probe hybridization assays are available. It is not possible to culture the virus in regular culture media, and therefore, culture for parvovirus B19 is not used as a diagnostic test [
42].
4. Fetal Diagnosis
4.1. Diagnosis of Infection
Fetal hydrops associated with or without moderate/severe anemia in absence of a relevant cause should prompt amniocentesis followed by PCR to detect parvovirus B19 [
44]. In these cases, maternal serology is useful only if both IgG and IgM are negative, ruling out maternal and therefore fetal infection. In all other cases, maternal serology is compatible with possible fetal infection, including positive IgG and negative IgM [
39].
All diagnostic methods have limitations. The use of PCR is only useful in the viremic period, when viral particles can be traced [
45]. On the other hand, the immune response of fetal IgG and IgM is unpredictable due to the immaturity of the fetal immune system, so fetal serology is rarely used and less useful for diagnosis [
39,
43]. PCR for parvovirus B19 can be performed on fetal blood samples obtained by cordocentesis, but this technique has a fetal loss rate of approximately 1%. Amniotic fluid sampling has a higher detection rate with less chance of complications and is therefore preferred for diagnosis [
39,
42]. In postmortem samples, electron microscopy can detect intranuclear inclusions or viral particles, orienting the diagnosis [
45].
4.2. Diagnosis of Fetal Anemia
In pregnant women who have recently been infected with parvovirus B19, and the infection has been demonstrated, the risk of maternal–fetal transmission is high, and a close US follow-up with a specialist obstetrician must be planned. The fetus must be closely monitored to detect fetal anemia early, which may arise from 8 to 12 weeks after infection, and then every one to two weeks [
39,
42].
Fetal anemia is initially monitored non-invasively by assessing peak systolic velocity of the middle cerebral artery (PSV-MCA) using Doppler ultrasound. Moderate/severe fetal anemia is highly indicative of the presence of a PSV-MCA greater than 1.5 times the median (MoM) at 18 weeks of gestation or later [
46,
47,
48,
49].
Parvovirus B19 infection is unlikely the cause of fetal anemia in the absence of ultrasound changes suggestive of fetal sequelae 8 to 12 weeks after possible exposure. Cordocentesis with fetal blood sampling to determine fetal hematocrit and intrauterine transfusion may be required in cases of fetal hydrops or severe fetal anemia [
46,
47,
48,
49]. Other signs of fetal parvovirus B19 infection include fetal ascites and cardiomegaly. Generalized edema and pericardial effusion occur in more advanced stages of the disease. Hyperechogenic bowel, meconium peritonitis, increased nuchal translucency in the first trimester, and amniotic fluid abnormalities have also been reported as US anomalies [
50,
51,
52].
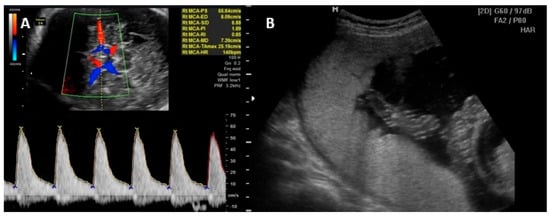
Figure 2 illustrates the PVS-MCA measurement and the intrauterine transfusion.
Figure 2. (A) Peak of systolic velocity of the middle cerebral artery Doppler measurement technique. (B) Intrauterine transfusion with the needle in the vein at level of umbilical cord insertion on placenta.
5. Prognosis
Although parvovirus B19 infection contributes little to the overall increase in the rate of fetal demise, infection has been found to increase the risk of fetal death, spontaneous abortion, and stillbirth compared with uninfected women [
53,
54]. The most important determinant of mortality and adverse perinatal outcomes is the presence of fetal hydrops, with a mortality rate of approximately 29%. Spontaneous resolution of anemia occurs in approximately 5.2% of fetuses with hydrops compared to approximately 49.6% of non-hydropic fetuses [
34].
Mortality in parvovirus B19 infection can be dependent on the gestational age. Pregnant women diagnosed with the infection in the first trimester had an abortion rate of about 13% compared to 9% in patients diagnosed between 13 and 20 weeks of gestation. The majority of fetal deaths (80%) occurred up to 4 weeks after infection [
55].
Parvovirus B19 infection itself, in the absence of hydrops or significant fetal anemia, does not appear to cause long-term neurologic morbidity, but further studies are needed [
6,
26]. However, severe anemia or hydrops may be an independent long-term risk factor for neurologic sequelae. In reported cases of survivors of fetal hydrops, neurological complications include ventriculomegaly, polymicrogyria, cerebral heterotopia, and other anomalies of the central nervous system [
56,
57]. The prevalence of anomalies in brain imaging scans is around 9.8%. The risk of neurodevelopmental abnormalities is almost 10% in children with a history of fetal hydrops due to parvovirus B19 infection [
34]. Neurodevelopmental disorders, although rare, can also occur after intrauterine transfusion in up to 12% of children, and these disorders can range from mild cognitive delay, mild fine motor impairment to severe developmental delay with neurological abnormalities such as ataxia, hypertonia, and cerebral palsy [
58].
This entry is adapted from the peer-reviewed paper 10.3390/jpm14020139