Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Chaiyavat Chaiyasut and Version 2 by Sirius Huang.
Hair health is associated with personal distress and psychological well-being. Even though hair loss (alopecia) does not affect humans’ biological health, it affects an individual’s social well-being. So, treatment for hair problems and improving hair health are obligatory.
- hair loss
- alopecia
- phytochemicals
- hair health
- hair growth stimulation
1. Introduction
The history of alopecia areata (AA) starts approximately 1500 before the common era (BCE), but scientific studies on hair loss have accelerated in recent decades in terms of publications [1]. Even though hair is not important for humans in terms of biological protection, hair loss has significant social, psychological, and emotional impacts on everyone. Therefore, treatment for hair loss and improving hair health is obligatory.
Humans have ~100,000 scalp hair shafts with varying degrees of hair growth, and the average life cycle of a hair shaft is ~3.5 years, with a growth rate of 0.05 inches per month. The hair has three regions, such as medulla (innermost layer, developed from transparent cells and varies among hair types), cortex (middle layer, which provides strength to the hair shaft, composed of keratin protein), and cuticle (outer layer). The hair follicle can be divided into the lower, middle (isthmus), and upper (infundibulum) segments. The lower segment includes the bulb and suprabulb regions. The middle segment of the hair follicle includes the region covering the arrector pili muscle insertion to the opening of the sebaceous gland duct. The upper segment of the follicle includes the region between the opening of the sebaceous gland duct and the follicular orifice [2].
Anagen (growth phase, lasts for 2 to 7 years), catagen (exponentiation, lasts for 2 to 4 weeks), and telogen (resting phase, lasts for 3 months) are three major phases of the hair growth cycle. The amount of scalp hairs may change based on the anagen (85 to 90.6%), telogen (10 to 15%), and catagen (1 to 2%) phases. Pigmented hair shafts are produced in the anagen phase, and the follicle achieves its maximum length and volume. During the catagen phase, the epithelium of the lower follicle breaks and grows up with the papilla until it lays below the bulge zone, establishing the club hair. Telogen is a quiescence phase of the hair cycle, characterized by the reduction of proliferation and biological activity of hair follicles [2][3][4][2,3,4].
Hair color, density, hair fiber curvature, and diameter are affected by the aging of hair, which overall contribute to the appearance and manageability of hair [5][6][5,6]. Numerous factors affect hair health and the hair growth cycle. Heavy metals (thallium, mercury, arsenic), toxins (Botulinum, Podostroma cornu-damae), drugs, medications, genetics, stress, smoking, menopause, lifestyle, and diet are some of the major factors associated with hair health [7][8][9][10][11][12][13][14][7,8,9,10,11,12,13,14].
Various drugs and treatment strategies were used to treat hair loss. Minoxidil was the first drug approved by the FDA to treat hair loss [15][16][15,16]. 5α reductase inhibitors (e.g., Finasteride, Dutasteride) are also used to treat male androgenetic alopecia [17][18][17,18]. The combination of finasteride and minoxidil treatment significantly improved hair health, and the combination therapy is more effective than a single treatment procedure. Furthermore, hair transplantation [19] and cell therapy [20] are effective treatments for hair loss.
Many phytochemicals include epigallocatechin gallate (EGCG), caffeine, capsaicin, procyanidin, onion juice, pumpkin seed oil, rosemary oil, saw palmetto [21][22][21,22], red ginseng extract [22], curcumin, garlic gel, and other natural products such as amino acids, marine proteins, melatonin, vitamins, and zinc [21], were reported to have hair growth-stimulating property [21][22][21,22]. Recently, researchers have been interested in herbal-based nanomedicine for hair health [23]. Furthermore, several mechanisms have been proposed and proved for the hair growth-promoting properties of phytochemicals [24][25][26][27][28][29][30][24,25,26,27,28,29,30].
2. Types of Alopecia
Alopecia can be classified based on the cause and appearance and rarely by gender. Androgenetic alopecia (AGA), telogen effluvium (TE), alopecia areata (AA), and scarring alopecia (SA) are the common types of hair loss [31]. AGA is an androgen-dependent hair loss. About 58% of men may be affected by AGA. Hair loss starts with bitemporal hairline decline and thinning at the vertex and frontal-parietal regions. About 33% of Caucasian women aged 70 or older may be affected by AGA. Postmenopausal and genetically susceptible women are mainly more sensitive to AGA [31]. TE is a nonscarring form of hair loss, a scalp disorder exemplified by excessive hair shedding [32]. The changes in the hair cycle could cause TE, which could be acute or chronic hair loss. Older women are more susceptible to acute TE attributed to drugs, childbirth, and thyroid-related diseases [33], even though age’s influence on TE is unclear. The incidence of TE in children was about 2.7% in Southeast Nigeria [34]. Telogen gravidarum, nutrition, zinc, iron deficiency, genetics, chronic renal and hepatic failure, syphilis, early AGA, infection, stress, and malignancy are some factors that cause TE [33]. There are five types of TE based on the hair follicle cycle: immediate and delayed anagen release, immediate and delayed telogen release, and short anagen syndrome [35]. High fever, surgical trauma, starvation, and hemorrhage are the triggers for acute TE. The hair loss may occur after two to three months of the triggering event. Not all cases have the triggering event in their life. So, the cause of TE is still not yet understood completely [33][35][33,35]. The diagnosis of acute TE can be conducted by history and examination. Acute TE is a self-limiting biological event, so if the hair loss stops spontaneously, no further treatments are needed. Nevertheless, if hair loss continues (Chronic TE), medical evaluations are needed to find the cause and proper treatment [31]. AA is a nonscarring and defined hair loss due to the premature conversion of the anagen to telogen phase in hairs. Family history and autoimmune conditions are the major cause of AA; other than that, no specific cause of AA has been defined yet [36]. A higher incidence of AA has been observed in the female population. The etiology of AA is elucidated completely. The activation of immune cell androgen and estrogen receptors during pregnancy, X chromosome-mediated innate immune response and immune tolerance, and maternal micro-chimerism of fetal immune cell lines are associated with the etiology of AA. The average age of disease inception varied based on ethnicity and gender. Female patients with autoimmune diseases are reported for the incidence and progress of AA compared to their male equivalents [37]. SA is irreversible hair loss and is commonly found in European Caucasian women. SA is divided into two subgroups such as primary SA and secondary SA. In primary SA, hair follicles have microscopic inflammation and damage the follicular epithelium without affecting the interfollicular reticular dermis. Primary SA is associated with chronic cutaneous lupus erythematous (an autoimmune condition), pseudopelade of Brocq, lichen planopilaris (inflammation in hair follicles), folliculitis decalvans (chronic inflammation of hair follicles and scalp), and dissecting folliculitis. The underlying disease that causes primary SA could be predicted by knowing the type of inflammatory infiltrates around hair follicles. In secondary SA, hair follicle damage is related to a non-follicle-directed cause [38]. Exogenous factors such as trauma, endogenous infiltrative, and inflammation cause secondary SA [39]. Central centrifugal cicatricial alopecia (CCCA) caused by hair treatments using chemicals and irons is also considered secondary SA [31], and its incidence is associated with diabetes mellitus [40].3. Factors Affecting Hair Health
Several factors affect hair health, including genetics, chemical exposure, lifestyle, smoking, drugs, stress, infection, and menopause. Evidence for some of the influencing factors of hair health has been detailed in this section (Figure 1).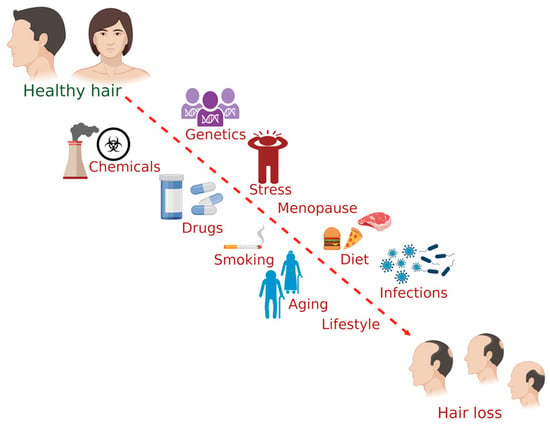
Figure 1.
The common factors influencing hair health in humans. (The figure was created using
; accessed on 17 November 2022).
