Since the beginning of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, pharmaceutical companies and research institutions have been actively working to develop vaccines, and the mass roll-out of vaccinations against COVID-19 began in January 2021. At the same time, during lockdowns, the consumption of alcoholic beverages increased. During the peak of vaccination, consumption remained at high levels around the world, despite the gradual relaxation of quarantine restrictions. Two of the popular queries on search engines were whether it is safe to drink alcohol after vaccination and whether this will affect the effectiveness of vaccines. MOver the past two years, many studies have been published suggesting that excessive drinking not only worsens the course of an acute respiratory distress syndrome caused by the SARS-CoV-2 virus but can also exacerbate post-COVID-19 syndrome. Despite all sorts of online speculation, there is no specific scientific data on alcohol-induced complications after vaccination in the literature. Most of the published vaccine clinical trials do not include groups of patients with a history of alcohol-use disorders.
- COVID-19
- vaccines
- alcohol
1. Introduction
2. The Impacts of Alcohol Consumption on the Immune System
Alcohol modulates both innate and adaptive immunity. Several lines of evidence suggest that epithelial cells, macrophages, and dendritic cells, as the first lines of immune defense, are the most susceptible to high doses of alcohol. Ethanol weakens the ability of leucocytes to migrate to sites of infection; induces functional abnormalities in T and B lymphocytes, natural killer cells, and macrophages; and alters cytokine expression [21][22]. Elevated serum levels of tumor necrosis factor α (TNFα) and interleukin (IL-6), together with decreased IL-10, interferon γ (IFN-γ), and IL-2 levels, are the usual parameters of patients with chronic alcoholic liver disease [22][23][23,24]. Many published articles suggest that alcohol consumption has a dose-dependent effect on the response to infection. Those with alcohol disorders are 3–7 times more susceptible to bacterial pneumonia and tuberculosis, and they are prone to the progression of chronic viral infections, such as human immunodeficiency virus (HIV) and hepatitis C [7]. Alcohol metabolism varies from person to person. It depends not only on the sex and constitution of the person but also on the content of metabolizing enzymes in the liver [24][25]. The liver, an important component of the innate immune system, when damaged due to chronic alcohol abuse, results in the decreased production of antibacterial proteins, thereby increasing the susceptibility to bacterial or viral infection. Patients with alcohol disorders also have an increased susceptibility to respiratory pathogens and an increased risk of acute respiratory distress syndrome (ARDS) [25][26]. Not only chronic alcohol use can lead to negative effects on the immune system [2]. In fact, studies show that heavy drinking also affects the immune system. It has been reported that patients with acute alcohol intoxication are more prone to peritonitis development following penetrating abdominal trauma [26][28]. In experimental models, acute alcohol intoxication has been demonstrated to impair the mucociliary defense of airways against invading pathogens [27][29]. However, some animal and clinical studies suggest that moderate alcohol consumption reinforces the immune response to infection and vaccination. In a clinical study that included 391 patients with a cold who were exposed to different respiratory viruses, Co-hen et al., found that consuming a large number of alcoholic drinks (3–4/day) decreased the risk of developing colds that were confirmed by clinical symptoms and specific antibody titers [28][30]. Some of the health benefits of moderate beer consumption may be due to its ability to interfere with pro-inflammatory cytokine cascades [29][31]. It should be remembered that the severity of the effects of the immune status in people with alcohol-use disorders depends not only on the time of consumption and the amount of alcohol but also on age, sex, body composition, environmental factors, and even the type of alcoholic beverage [30][32]. Antioxidants and polyphenols found in red wine and phytoestrogens and vitamins found in beer could be protectors against immune cell damage and cytokine overexpression [31][32][33][33,34,35]. Ethanol can harm immune cells due to the formation of free radicals during metabolism, but antioxidants should provide protection against this [34][36]. Interestingly, the degree of a hangover the day after alcohol consumption does not affect alcohol-induced immune changes [35][37].3. “Spike Effect” of COVID-19 Vaccines and Alcohol
The SARS-CoV-2 spike protein (S protein, SP) is a clove-shaped transmembrane structural glycoprotein that is localized on the surface of the SARS-CoV-2 virus [36][38]. This unit is responsible for the recognition of and the binding to the host cell angiotensin-converting enzyme 2 receptor (ACE2), thus making the S protein the main target of neutralizing antibodies [37][39]. The large ectodomain of coronavirus S proteins includes two subunits, subunit 1 (S1), containing a receptor-binding domain (RBD), and the membrane-fusion subunit 2 (S2). The S protein is an ideal target for vaccine development on different platforms because it has a high antigenicity and the ability to induce a robust immune response [38][40]. Almost all types of COVID-19 vaccines run the endogenous synthesis of the SARS-CoV-2 spike protein. Synthetized S proteins move via blood circulation, interacting with ACE2 receptors and demonstrating the pathological features of SARS-CoV-2 [39][41]. A maximum concentration (14.6 μg/mL) of S proteins in blood serum was detected 24 h after vaccination and was reduced within 10 days [40][42]. Suggestions have been published that the spike protein may be responsible for the long-term effects of COVID-19, such as rare neurological complications, including Guillain–Barre syndrome and Bell’s palsy [41][43]. A growing body of research points to the potential dangers of the spike protein, even in the absence of the intact virus. The S protein has been reported to mediate pro-inflammatory and/or damaging (of various etiologies) responses in various human cell types [42][43][44,45]. Systemic inflammation, induced by the spike protein, may proceed through the TLR2-dependent activation of the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway [44][46]. There are several in vitro studies suggesting the negative impact of the S protein on endothelial barrier function [45][46][47][47,48,49]. Other reports indicate that the S protein induces an inflammatory response in human corneal epithelial cells and binds to lipopolysaccharide (LPS), enhancing its pro-inflammatory activity [48][49][50,51]. Several publications have reported that the spike protein leads to hemagglutination, blood coagulation, and thrombosis [50][51][52,53]. Boschi et al. showed that the Wuhan, Alpha, Delta, and Omicron B.1.1.529 variants of the SARS-CoV-2 spike protein mixed with human erythrocytes led to hemagglutination [52][54]. There is evidence to suggest that alcohol consumption may cause the activation of the ACE2 receptor and, consequently, enhance the negative effect of the spike protein (Figure 1). Balasubramanian et al., observed an increase in ACE2 in brain expression in both chronic alcohol exposure and abrupt withdrawal from alcohol [53][55]. Reportedly, alcohol consumption induced the intracellular accumulation of reactive oxygen species (ROS), which leads to the activation of NF-κB and an increase in vascular endothelial growth factor (VEGF) and monocyte chemoattractant protein-1 (MCP-1) [54][56]. Moreover, alcohol could be an independent cause of syndromes, similar to COVID-19-vaccine-related side effects. A few recent clinical cases discussed the possibility that heavy alcohol consumption may play a role in the pathogenesis of Guillain–Barré syndrome [55][56][57,58]. Another study demonstrated that alcohol abuse was negatively associated with Bell’s palsy occurrence [57][59]. Thus, it can be assumed that alcohol consumption may provoke or enhance the “spike effect” of COVID-19 vaccines.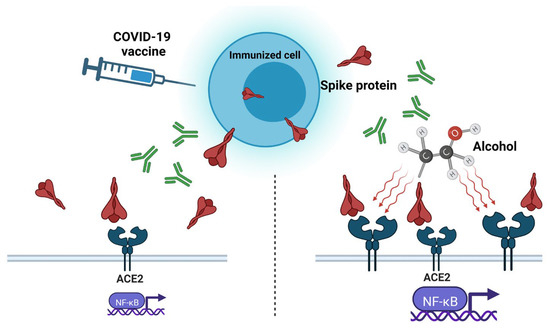
4. Protein Subunit Vaccines and Alcohol
5. Inactivated Whole-Virus Vaccines and Alcohol
Vaccines based on inactivated pathogens have been used for over a hundred years as a protective agent against bacteria and viruses. Inactivated viral vaccines are first cultivated on a substrate (primary and continuous cell lines, tissues, fertilized eggs, and even whole organisms) to produce large amounts of antigens [64][66]. The multiplied virus in the substrate is purified, concentrated, and inactivated by various chemical agents (ascorbic acid, hydrogen peroxide, etc.) or by using physical methods (heat, ultraviolet exposure, gamma irradiation, etc.). In recent decades, only formaldehyde and β-Propiolactone have been used as inactivated agents for human viral vaccines [65][67]. Adjuvants are important components of many inactivated vaccines due to their ability to induce more robust and long-lasting specific immune responses [66][68]. Aluminum salts, such as aluminum hydroxide, phosphate, and potassium sulfate, have been widely used in vaccines for a long time [67][69]. Developed in China, the inactivated whole-virus vaccine Sinopharm (Beijing, China) BBIBP-CorV, containing an aluminum hydroxide adjuvant, has been approved by the WHO for emergency use, and it has been distributed in more than 40 countries [68][70]. Another Chinese vaccine approved by the WHO is CoronaVac (Sinovac (Beijing, China)), an inactivated SARS-CoV-2 aluminum-hydroxide-adjuvanted vaccine created from African green monkey kidney cells (Vero cells) that have been inoculated with SARS-CoV-2 [69][70][71,72]. In both BBIBP-CorV and CoronaVac clinical trials, alcohol addiction was one of the exclusion criteria [71][73]. No serious adverse reactions to vaccines, which could be aggravated by alcohol consumption, have been reported. A clinical study carried out by Jingwen Ai et al., demonstrated the safety of inactivated whole-virion SARS-CoV-2 vaccines in patients with alcoholic liver disease; however, those patients demonstrated a lower immunologic response to the vaccines than healthy patients [72][74].6. Viral-Vector-Based COVID-19 Vaccines and Alcohol
On 29 January 2020, the European Commission granted conditional marketing authorization for the Oxford/AstraZeneca COVID-19 vaccine (Covishield, Vaxzevria (Oxford, UK)), a monovalent vaccine composed of a single recombinant, replication-deficient chimpanzee adenovirus (ChAdOx1) vector encoding the S glycoprotein of SARS-CoV-2. However, five countries in the European Union have since placed age limitations on the vaccine, which has given rise to a certain distrust in it [73][79]. One of the rare but most severe side effects of this vaccine is a syndrome named vaccine-associated immune thrombosis and thrombocytopenia (VITT) [74][80]. Usually, the administration of a viral-vector-based COVID-19 vaccine induces the production of antibodies to the SARS-CoV-2 S protein. In very rare cases, VITT antibodies are generated that can bind to platelet factor 4 (PF4) and construct immune complexes that lead to a coagulation cascade and reduce the number of platelets [75][81]. As of April 2021, there had been 222 registered cases of VITT in Europe [74][80]. The Victorian Department of Health (Australia) equated this to eight cases of thrombopenia per million doses for the AstraZeneca vaccine [76][82]. Based on several reported cases, young women, especially those taking hormonal contraceptives, are at the highest risk of developing this vaccine-related adverse reaction [74][80]. Consequently, the AstraZeneca vaccine has not been authorized for use in the U.S. There have been no reports of Oxford/AstraZeneca-vaccine-related thrombosis and thrombocytopenia complications after alcohol consumption. However, binge alcohol consumption can lead to endothelial dysfunction, which, in combination with stasis and hypercoagulability, could increase venous thromboembolism (VTE) formation [77][83]. Liver dysfunction, caused by chronic alcohol intoxication, decreases the synthesis of anticoagulant thrombotic factors [78][84]. Nonetheless, there are also studies suggesting that low or moderate alcohol consumption could decrease the risk of deep venous thrombosis and pulmonary embolism in older people [79][85]. The ethanol treatment of human whole blood led to a decrease in PF4 release in response to a-thrombin [80][86]. According to Abolmaali’s study, AstraZeneca is the vaccine most reported to be associated with Guillain–Barré syndrome [81][87]. Summarizing the above facts, itwe can say that young people who drink alcohol, as well as those who chronically drink alcohol, have an increased risk of complications after immunization with the Oxford/AstraZeneca vaccine (Figure 2).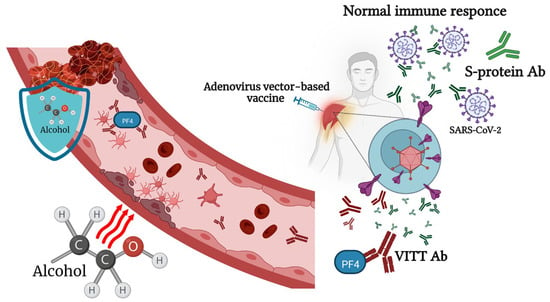
7. mRNA-Based Vaccines and Alcohol Consumption
The first report of protein production following reporter gene mRNA in mice was published by Wolff at al. in 1990 [94][100]. During that period, pharmaceutical companies did not consider mRNA a prospective technology because of doubts about its stability and its low efficacy [95][101]. Despite mRNA vaccines representing only 11% of all the developed COVID-19 vaccines, two mRNA vaccines, mRNA-1273 and BNT162b, were the first vaccines approved by the FDA and EUA for COVID-19 [96][102]. Both new mRNA vaccines, BNT162b2, manufactured by Pfizer/BioNTech, and mRNA-1273, produced by Moderna, contain molecules of RNA, modified with pseudo-uridine and encapsulated in a lipid nanoparticle vehicle. The Pfizer–BioNTech and Moderna vaccine constructs do not contain an S-protein S1/S2 furin cleavage site. Ribonucleic acid is endowed to be rapidly translated into nonactive SARS-CoV-2 S proteins in a stable closed structure in order to induce the immune response without causing cell damage due to its interaction with the ACE2 receptor [97][103]. However, these two vaccines were the most feared among people at the initial stage of vaccination due to the lack of data on their long-term side effects.
The S protein encoded by the vaccine is stabilized in its pre-fusion form; thus, it is possible that, if it enters the bloodstream and is distributed systemically throughout the human body, it may contribute to adverse effects [98][104]. Ndeupen et al., reported that the mRNA platform’s lipid nanoparticle (LNP) component used in preclinical vaccine studies causes a highly inflammatory response in mice. LNPs administrated intra-dermally, intramuscularly, or intranasally at a dose of 10 μg/mouse led to severe neutrophil infiltration, the activation of inflammatory pathways, and cytokine and chemokine production [99][105]. Such a reaction, in combination with the spike effect, can increase the negative consequences of vaccination in the body. Among Japanese healthcare workers who were vaccinated with the BNT162b2 mRNA vaccine, alcohol consumption, along with other factors, was identified as a factor predicting lower IgG antibody titers after vaccination [100][106]. Wang et al., in their study of vaccinated patients with substance use disorders (SUDs), including alcohol disorders, demonstrated that patients with SUDs remain vulnerable to COVID-19 breakthrough infection, even after full vaccination. The risk was higher in patients who received the Pfizer-BioNTech vaccine than in those who received the Moderna vaccine [18][19]. Several cases of myocarditis have been reported following the administration of COVID-19 mRNA vaccines [101][107]. After the self-controlled case series, studies found that myocarditis after vaccination is higher in men younger than 40 years old, particularly after the second dose of the mRNA-1273 vaccine [102][108]. Excessive alcohol consumption can cause non-ischemic dilated cardiomyopathy and chronic heart disease, characterized by dilation and the impaired contraction of myocardial ventricles [103][109]. Of all alcohol-related myocardiopathy cases, 30% were myocarditis with a lymphocytic infiltrate in association with myocyte degeneration or focal necrosis [104][110]. Most people who heavily drink alcohol do not have any symptoms in the earlier stages of the disease, and many never develop clinical heart failure [105][111]. A case of vasospastic angina (VSA) caused by alcohol consumption following Pfizer/BioNTech vaccination has been reported [106][112]. Thus, a patient who chronically drinks alcohol, unaware of the presence of heart problems, could exacerbate them with an injection of the mRNA COVID-19 vaccine. Mark J. Mulligan et al., reported that up to 50% of patients demonstrated a decrease in lymphocytes after the first dose of the BNT162b1 vaccine [107][113], which, combined with the negative effect of alcohol on these cells, can have severe consequences for the immune system. There is no data suggesting that other alcohol-associated chronic illnesses reduce the effectiveness of mRNA vaccines. Patients with compensated and decompensated cirrhosis demonstrated a 100% reduction in COVID-19-related hospitalization or death following the first dose of either the BNT162b2 or the mRNA-1273 vaccines [108][114].