Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Manoj K. Pandey and Version 3 by Camila Xu.
Multiple myeloma (MM) is caused by aberrant plasma cells (PCs) in the bone marrow (BM), representing 1% of neoplastic diseases and 13% of hematological neoplasms. MM is a challenging cancer to diagnose and treat.
- multiple myeloma (MM)
- autophagy
- apoptosis
1. Introduction
Lymphoma, leukemia, and myeloma are the three main classifications for cancers of the hematopoietic system. Multiple myeloma (MM) is caused by aberrant plasma cells (PCs) in the bone marrow (BM), representing 1% of neoplastic diseases and 13% of hematological neoplasms [1]. MM is a challenging cancer to diagnose and treat. Patients go through two early stages of the disease before acquiring aggressive myeloma. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) are the precursor stages with no clinical symptoms defined (Figure 1). Depending on the stage of the disease, the number of abnormal PCs, levels of monoclonal immunoglobulin (Ig), and cytogenetic abnormalities begin to rise, and ultimately patients become symptomatic (hypercalcemia, anemia, renal insufficiency, bone lesions, and multiple infections), and referred as MM. The American Cancer Society estimates that by the year 2022, approximately 34,470 new cases of MM will be diagnosed and 12,640 deaths from MM in the United States will occur [2].
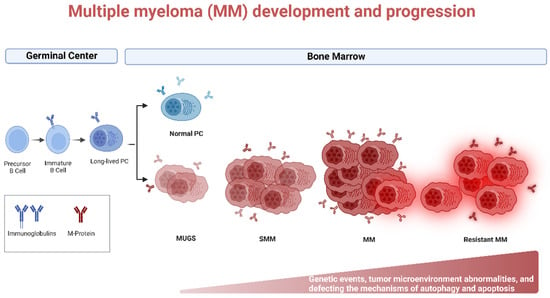
Figure 1. Biology of Multiple myeloma (MM) development and progression. MM is the end stage of a multistep neoplastic transformation of PCs. MGUS and SMM are the precursor stages of MM. Increase in aberrant PCs, Igs, and cytogenetic and tumor microenvironment abnormalities precede the onset of symptoms of MM. Relapsed/refractory (R/R) patients often present with a more aggressive phenotype. Genetic events, tumor microenvironment abnormalities, and defective autophagy and apoptosis may occur during MM progression. Created using Biorender.com (accessed on 1 November 2022).
The interaction of myeloma cells to bone marrow microenvironment (BMM) is the hallmark of MM [3]. Although treatment options for MM have improved remarkably over the last several decades, the survival rate remains extremely low, and all patients experience relapse or become refractory. Unsurprisingly, refractory and relapsed (R/R) patients often present with a more aggressive phenotype upon recurrence. It has been established that cytogenetic and epigenetic abnormalities play critical role in MM progression and resistance to available drugs. However, defective mechanisms of autophagy, apoptosis, tumor microenvironment, and cell survival signaling contribute in MM progression and drug resistance. Table 1 illustrates the common drugs that have been used to treat MM patients, its mechanism of action, and underlying mechanisms of drug resistance.
Table 1.
Mechanism of action and underlying drug resistance mechanisms of the common chemotherapeutic agents.
| Class | Drugs | Mechanism of Action | Type of Resistance | Mechanism of Resistance | |||
|---|---|---|---|---|---|---|---|
| Alkalyting agents Anthracyclines |
Melphalan Cyclophosphamide Doxorubicin |
Impairment of DNA synthesis and cell replication, immunostimulatory activity by inhibiting interleukin-6 (IL6), interaction with dendritic cells, and immunogenic effects in the tumor microenvironment [4][5][4,5]. Topoisomerase II inhibition (Doxorubicin). | Alters autophagy and apoptosis signaling pathways Cancer stem cells and bone marrow microenvironment |
Upregulation of anti-apoptotic proteins (Mcl-1, Bcl-2, Bcl-xL) [6][7][6,7]. Stem cell-like phenotype with triggering of ALDH1A1 enzymatic activity and upregulation of BTK [8][9][8,9]. Increase of cell adhesion molecules (VLA4) [10]. |
|||
| Proteasome inhibitors | Bortezomib Carfilzomib Ixazomib |
Inhibition of proteasome activity; inhibition of NF-κβ activity; induction of apoptosis by activation of caspase-8 and -9; upregulation of pro-apoptotic protein Noxa; downregulation of adhesion molecules on myeloma cells [4][11][12][13][14][15][16][17][18][4,11,12,13,14,15,16,17,18]. | Alters autophagy and apoptosis signaling pathways Cancer stem cells and bone marrow microenvironment |
Upregulation of the proteasomal system; Upregulation of anti-apoptotic proteins (Mcl-1, Bcl-2, Bcl-xL); activation of autophagy pathway; induction of NF-κβ; unfolded protein response (UPR) transcription factor XBP1 suppression; overexpression of heat shock proteins [3][19][20][21][22][3,19,20,21,22]. Stem cell-like phenotype with triggering of ALDH1A1 enzymatic activity and upregulation of BTK [8][9][8,9]. Secreting a group of extracellular signaling cues including IL-6, growth factors such as vascular endothelial growth factor (VEGF), and Insulin-like growth factor 1 (IGF-1); trigger and modulate multiple keys of the transcriptional pathway including Ras/MAPK, JAK/STAT3, and PI3/Akt; Increase of pro-inflammatory TNF-α; Increase of different cell adhesion molecules; overexpression of CXCR4; overexpression of MARCKS [22][23][24][25]][22,23[,2426],25[27],26[,2728,28]. |
|||
| Immunomodulatory agents | Thalidomide Lenalidomide Pomalidomide |
Induction of apoptosis by activation of cspase-8 and -9; interaction with BMM and downregulation of adhesion molecules; affecting cereblon (CRBN) and downstream targets; regulation of T and natural killer (NK) cells activity; anti-angiogenic activity [29][30][29,30]. | Cancer stem cells and bone marrow microenvironment | Stem cell-like phenotype with triggering of ALDH1A1 enzymatic activity and upregulation of BTK [8][9][8,9]. Downregulation of CRBN expression and deregulation of IRF4 expression; increased IL-6 expression and constitutive STAT3 activation [31]. | |||
| Histone deacetylase inhibitors | Panobinostat Vorinostat |
Increasing chromatin structure opening, end with activation of tumor suppressor genes [32][33][32[34],33,34]. | Preclinical Bone marrow microenvironment and disruption intracellular signaling pathways | [Regulation of actin cytoskeleton and protein processing in endoplasmic reticulum (triggering of MEK/ERK, PI3K, and FAK pathways) [35]. | |||
| 65 | ] | [93] | Monoclonal antibodies | Daratumumab Elotuzumab Isatuximab |
Antibody-dependent cellular cytotoxicity (ADCC); complement-dependent cytotoxicity (CDC); modulation of target antigen enzymatic activity; macrophage-mediated pagocytosis; apoptosis via Fcγ receptor-mediated crosslinking; stimulation of immune cells activity, particularly T and NK cells [36][37][38][39][40][41][36,37,38,39,40,41]. | Bone marrow microenvironment | Competition by the soluble extracellular forms of CD38 and SLAM7 [42]. |
| Selective Exportin 1 (XPO1) inhibitor | Selinexor | Induces apoptosis through nuclear retention and functional activation of tumor suppressor proteins (TSPs), inhibits NF-κβ, and the translation of oncoprotein mRNAs [43][44][45][43,44,45]. | - | - | |||
| Corticosteroids | Dexamethasone Prednisolone Methylprednisolone |
Induction of apoptosis [46]. | Bone marrow microenvironment | Increased secretion of pro-survival cytokines bone marrow microenvironment [4][47][4,47]. |
2. Autoghagy in MM
Among the many essential biological functions of autophagy, it plays a critical role in innate and adaptive immunity. Autophagy helps eliminate various microorganisms, controls pro-inflammatory signaling and secretion of immune mediators, and controls homeostasis of lymphocyte and antigen presentation [48][76]. B lymphocytes include two distinct populations known as B1 and B2 cells, which vary distinctively in function and development. The B1 cells are involved in the innate immune system as opposed to the B2 cells, which are considered part of the adaptive immune system [49][77]. Autophagy is not necessary for B1 and B2 cell development but is required for B1 self-renewal in the periphery. Moreover, autophagy plays a vital role in the B2 cell’s Toll-like receptor (TLR) activation [50][78]. Pengo et al. demonstrated thatPCs have high autophagic activities and suggested that autophagy has a general role in PC oncogenesis. They also showed the viability of PCs as well as the importance of autophagy in sustaining antibody responses and its necessity in long-lived BM PCs [51][79]. Furthermore, Halliley et al. were able to demonstrate the importance of autophagy as a mechanism of survival in human long-lived PCs [52][80].
MM has similarities with the original plasma cell clone, such as an enlarged ER and cytoplasm, as well as immunoglobulin (Ig) secretion. MM cells produce a considerable amount of Ig, inevitably producing misfolded or unfolded proteins that can be toxic to the cells. MM uses various molecular pathways to protect the cells from damage and promote cell survival, including processes such as proteasomal degradation, UPR, and autophagy. In cases where there is excessive production of misfolded protein and the inability of the proteasomal system or UPR to deal with this stress, autophagy could be induced to help alleviate the stress. If all these survival mechanisms fail, apoptosis is engaged, and the cells get destroyed [53][54][55][81,82,83].
Autophagy in myeloma cells not only works in tandem with the ubiquitin-proteasome system (UPS) to remove ubiquitinated proteins [56][84], but it also plays a role in determining the susceptibility to proteasome inhibitors [57][85]. According to recent research on MM, greater immunoreactivity against autophagic markers including Beclin1 and LC3 corresponds with longer patient survival [58][86]. Furthermore, it has been shown that the imbalance between Beclin1 and p62 proteins expression promotes the proliferation of MM cells through autophagy regulation [59][87].
Aberrant DNA repair mechanisms contribute to illness development, initial translocations, and progression in MM. Melphalan (an alkylating agent) and bortezomib (a proteasome inhibitor) are two of the most common medications used to treat MM, they both work by inhibiting several steps in the DNA repair process that play a role in both the body’s response to therapy and any subsequent resistance [60][88]. DNA damage leads to the activation of autophagy, which plays a role in DNA damage response (DDR) and assists in cytokine secretion, senescence, cell death, and repairing DNA lesions [61][89]. DNA damage leads to the activation of ataxia-telangiectasia mutated (ATM) within the Mre11-Rad50-Nbs1 complex (MRN) that binds double-strand breaks. ATM is then able to activate AMPK that targets a TOR-Autophagy Spatial Coupling Compartment (TORC1) inhibitor known as tumor necrosis factor receptor (TNFR)-associated factor interacting protein 2 (TSC2). TORC1 acts as a negative regulator of the ULK complex; therefore, its inhibition allows autophagosome formation. ATM also regulates p53 and stabilizes it, and in turn, p53 regulates other autophagic pathways, including AMPK, PTEN, and damage-associated molecular pattern (DAPK). Furthermore, p53 modulates Sestrin, a protein that regulates TORC1 activity in an AMPK-independent manner through the GATOR2-GATOR1-RAGB/A (GTPase-activating protein activity toward RAGs) signaling pathway as well as via AMPK-dependent manner like how it affects TSC2. ATM activates Che-1, an RNA polymerase II-binding protein that increases the transcription of Deptor and Redd1 as well as inhibiting mTOR. ATM also modulates Beclin1 through the activation of the NF-ϰB essential modulator (NEMO)-dependent transforming growth factor (TAK1)-ATM-NEMO-NFϰB pathway. TAK1 can activate c-Jun N-terminal kinases (JNK), allowing Beclin1 to be released from antiapoptotic proteins. Autophagy also induced DNA damage by decreasing the transcription of MKP-1, a JNK phosphatase; thus, JNK induces autophagy. Moreover, DNA damage triggers an enzyme called PARP1, which in turn decreases cellular ATP and NAD+ levels, activating AMPK and initiating autophagy [61][89].
Cancer stem cells (CSC) could form cancers and self-renew, which is essential in resistance to anti-cancer agents. Autophagy is associated with the maintenance of CSC pluripotency and increases resistance to cancer drugs [62][90]. One of the prominent drugs used to treat MM patients is proteasome inhibitors (PIs). PIs cause an increase in the amount of misfolded or unfolded proteins, which increases ER stress. The cells adapt to this stress with the help of multiple pathways, including autophagy, which allows the cells to mitigate stressful environments and survive. Therefore, inducing autophagic cell death may potentially be an additional viable approach to dealing with MM. However, it has been shown that uncontrollable autophagy also promotes drug resistance in myeloma cells, and that blocking autophagy may restore sensitivity to medicines [63][64][91,92]. The most potent preclinical studies and clinical trials in MM involving autophagy inhibitor or inducer alone or in combination with bortezomib are summarized in Table 23.
Table 23.
Preclinical studies and clinical trials of autophagy inhibitor or inducer alone or in combination with bortezomib in MM.
| Drug | Study Design | Clinical Trial Status |
|---|---|---|
| Autophagy inhibitors | ||
| Chloroquine (CQ) | In combination with bortezomib and cyclophosphamide in R/R MM patients | Phase II (NCT01438177) |
| Hydroxychloroquine (HCQ) | In combination with bortezomib and in R/R MM patients | Phase I/II (NCT00568880) |
| 3-Methyladenine (3-MA) | Human MM cell lines (U266, MM.1S, RPMI8226, and ARH 77) | |
| Bafilomycin A1 | In combination with bortezomib in U266 MM cell line | Preclinical [66][94] |
| Elaiophylin | Human MM cell lines (U266, RPMI8226, KMS11, and H929) | Preclinical [67][95] |
| Autophagy inducers | ||
| Metformin | Human MM cell lines (RPMI8226 and U266) and in vivo NOD-SCID murine xenograft MM model | Preclinical [68][96] |
3. Apoptotic Pathways in MM
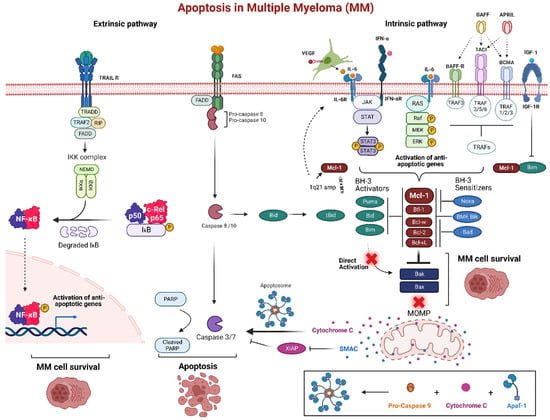
Anti-apoptotic proteins play a major role in the pathogenesis of MM. MM cells exhibit imbalances in their anti-apoptotic protein’s expression levels, especially Mcl-1, that leads to prevent apoptosis and allow continued cell growth by inhibiting and forming heterodimer interaction with Bax and Bak proteins. Mcl-1 is known to be overexpressed in MM and plays a crucial role in MM initiation, progression, and chemoresistance [3]. Remarkably, 52% of newly diagnosed and 81% of relapsed MM patients have shown an increase in Mcl-1 protein expression, which correlates with disease progression and a poor patient survival rate [19]. Furthermore, the most common change in gene expression of MM is Mcl-1 overexpression. Approximately 40% of MM patients have increased expression of Mcl-1 and IL-6 receptors due to a gain or amplification in 1q21 [69][111]. Many studies currently are focused on advancing treatment therapies for MM and overcoming resistance challenges through inhibition of Mcl-1. Importantly, it has been established that Bcl-2 and Bcl-xL inhibitors such as venetoclax (ABT-199), ABT-737 and navitoclax (ABT-263), which mimics the BH3 domain of Bad and binds Bcl-2 and Bcl-xL, result in upregulation of Mcl-1 and develop resistance. Thus, inhibiting Mcl-1 represent a promising strategy in MM-sensitive and -resistance cells. Another promising avenue for targeting chemotherapeutic resistance via Mcl-1 is through Noxa. Proteasome inhibitors such as bortezomib increase expression of Noxa which selectively targets Mcl-1 for proteasomal degradation [70][112].
MM cells receive critical signals from the BMM that help them avoid apoptosis and preserve long-term survival (Figure 23). By secreting a set of signaling signals, BM stromal cells (BMSCs) control the expression of anti-apoptotic Bcl-2 family proteins particularly Mcl-1. Transcription of Mcl-1 is regulated via growth factors (e.g., VEGF, EGF), cytokines (e.g., IL-6, IL-5, IL-3), as well as cytotoxic stimuli. MM cells create an IL-6/VEGF loop to interact with BMM. Secretion of IL-6 from MM cells triggers IL-6 release in the BMSCs, inducing more VEGF secretion from the malignant cells and increasing proliferation [71][113]. In the BMM, MM plasma cells are activated by several factors such as IL-6, JAK/STAT, rat sarcoma/mitogen activated protein kinase (Ras/MAPK), phosphatidylinositol-3 kinase (PI3-K)/Akt, and TNF family including B cell activating factor (BAFF), and a proliferation inducing ligand (APRIL). Additionally, IGF-1 can play a role in the survival of MM cells, which can activate NF-κB and Akt, as well as increase expression of FLIP and cIAP-2 which inhibit caspase-8 [72][114]. IGF-1 can also downregulate the expression of Bim, resulting in less antagonism of anti-apoptotic proteins [73][115]. Upregulation of IGF-1 and IL-6 have also been associated as a phenotype of resistance in bortezomib resistant cells [74][75][116,117].
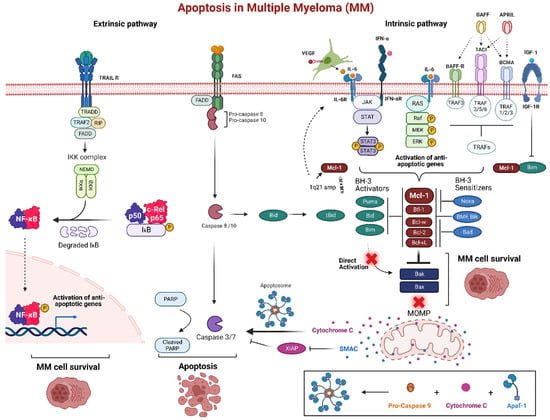
Figure 23. Apoptosis pathway in multiple myeloma (MM). The bone marrow microenvironment (BMM) is an important pathogenic factor for the long-term survival of MM. The intrinsic pathway of programmed cell death is promoted by signaling molecules from the BMM such as IL-6 and IFN-α that trigger various receptors in MM cells. These receptors, including tumor necrosis factor receptor-associated factors (TRAFs) through BAFF-R, BCMA, and TACI, as well as JAK/STAT or Ras/MAPK pathway activate anti-apoptotic proteins, particularly Mcl-1. Many MM patients develop increased expression of Mcl-1 and IL-6 via a gain or amplification of 1q21. This can create an IL-6/VEGF loop, as well as act as a mechanism of resistance through the upregulation of Mcl-1. Overexpression of anti-apoptotic proteins inhibits the BH3-only pro-apoptotic proteins and start competing for Bak and Bax binding site resulting MOMP inhibition. Normally, MOMP stimulation would release cytochrome c, forming the apoptosome after a conjunction with active caspase 9 and Apaf-1, to induce the executioner caspases 3 and 7 for apoptosis. The extrinsic pathway is triggered via the death receptors Fas and TRAIL. These receptors recruit FADD and pro-caspase-8 and 10 and can either directly activate caspase-8 and 10 to induce the downstream executioner caspases or activate Bid to induce MOMP. TRAIL receptor activation also activates anti-apoptotic genes via NF-κB complex. Created using Biorender.com (accessed on 12 December 2022).
