Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Rita Xu and Version 3 by Rita Xu.
Systems engineering captures the desires and needs of the customer to conceptualize a system from the overall goal down to the small details prior to any physical development. While many systems projects tend to be large and complicated (i.e., cloud-based infrastructure, long-term space travel shuttles, missile defense systems), systems engineering can also be applied to smaller, complex systems. The system of interest is the endoscope, a standard biomedical screening device used in laparoscopic surgery, screening of upper and lower gastrointestinal tracts, and inspection of the upper airway.
- endoscopy
- system architecture
- system lifecycle
- hyperspectral
- subsystem trends
- model-based systems engineering (MBSE)
1. Introduction
Systems engineering (SE) is a holistic engineering skillset and mindset structured to decompose large, complex systems down to nuts and bolts and ones and zeros prior to “breaking ground” on design and fabrication. The documentation produced from SE procedures is comparable to an instruction manual that traces those bolts and bytes into components, assays, and subsystems culminating to the final system. Simultaneously, the “manual” provides parameters and verification metrics that should be met at every level of decomposition to ensure the end product’s output is productive, safe, and correct for all stakeholders involved. A note of importance in the SE process is that the documentation produced should maintain a level of abstraction to allow for creative, inventive, and cost-effective design when producing physical aspects of the system. For example, a future smart city system needs to dynamically transmit data to the populous of autonomous vehicles on the street at X Mb/s. The requirement does not dictate that it should be Bluetooth or 5G link; it could be a new method of data transfer.
Systems engineering also tracks a system throughout its lifecycle, from conception to retirement and disposal. Researchers coin a new term called “system lifetime”, which considers many different lifecycles of a system throughout history, in other words, many generations of development of a system. Noteworthy models for lifecycle processes are the waterfall and spiral model [1]. These models are primarily used for software systems, but are also exemplary models for the iterative process of producing a physical system to meet the requirements set forth in the conceptual phase. These models have been beneficial to the structuring of this work considering the lifetime of a system. Considering the waterfall or spiral in a three-dimensional space with lengths of time between new waterfalls or spirals provided a unique concept to organize the many lifecycles of system development over the course of the system lifetime. Furthermore, Hossain and colleagues have recently detailed a review of systems thinking topics through a bibliometric analysis to highlight past trends and determine current gaps in knowledge of systems thinking [2], and researchers made use of some of the approaches presented in this review to analyze the development of endoscope systems and potential future directions. While SE is beneficial for new, large, complicated systems such as smart cities, green energy infrastructure, and digital medical recording techniques, it can also be utilized to review and optimize smaller, complex, existing technology such as the endoscope.
Endoscopy is a medical screening process by which internal (normally hollow) organs are imaged by the insertion of a scope with illumination and imaging capabilities. Through visualization, clinicians can optically diagnose infection, inflammation, or lesion growth and resect portions of tissue for pathological diagnostics. There are four major endoscopic techniques widely used today: white light endoscopy (WLE), narrow-band imaging (NBI), Fujifilm flexible spectral imaging color enhancement (FICE), and virtual endoscopy (VE). WLE is the gold standard technique used for decades to capture a typical RGB (red–green–blue) image providing reflectance-based images of the luminal wall [3][4][5]. NBI illuminates body cavities with blue and green light to harness the light absorption of the vasculature at these wavelengths providing additional contrast to the image [6][7]. FICE is a post-acquisition process that divides the RGB image into the respective three colors and digitally alters wavelengths to enhance the contrast [8][9]. VE uses coherent tomography scanning (CT scan) or magnetic resonance imaging (MRI) to render a 2D or 3D model of the hollow cavities traditionally imaged with an endoscope [10]. These techniques are detailed further for their strengths and weaknesses in Section 3. Pathologies of the gastrointestinal (GI) tract can at times be difficult to differentiate from the surrounding mucosa [4][11][12][13]. While current techniques provide several complementary modes for visualizing internal body cavities, the contrast and definition between healthy and afflicted tissue is limited, especially in early-stage cancer. The limited contrast between some cancers and the surrounding mucosa can have downstream consequences on detection accuracy and patient outcomes, for example in colorectal cancer, which is the third-ranking cancer in the United States for incidence and mortality rates [14][15][16][17]. Neoplasia (abnormal cellular growth) can be difficult to observe within the mucosal lining. If missed, neoplasia can become invasive and malignant (cancerous); in essence, researchers have let a cellular vehicle run a red light without getting ticketed. Tumor growth (1) can approximately double in volume annually [18][19], and (2) the standard of care for interval routine endoscopic screenings is 5 years [5]. Further, (3) a missed colorectal tumor could approximate a minimum 32× volume increase (assuming a constant exponential growth rate) before being detected at a subsequent colonoscopy. Therefore, it is important to develop improved technologies that provide high contrast and the ability to visualize neoplasia or early-stage cancer when viewing the hollow organs endoscopically.
2. Presenting, the Endoscope
Current state-of-the-art endoscope systems utilize a combination of broadband light sources (xenon arc lamps, halogens, or LEDs), bandwidth filtering, and digital analyses to produce WLE (gold standard), NBI, or FICE. One limitation of WLE is that small and subtle changes within the lumen may not generate sufficient contrast to be detected. In addition, abnormal, irritated, inflamed, or neoplastic tissue may appear very similar to normal tissue, resulting in difficulty determining potential areas of risk, especially for patients with underlying inflammatory conditions. To improve detection sensitivity and specificity, a range of correlating factors are often considered, such as: irregular mucosal patterns, condensed vasculature, and definitive redness. Introduced briefly before, NBI and FICE are two complementary modalities to WLE that can provide enhanced contrast of tissue structures between mucosa and lesions. NBI filters utilize narrow spectral bands in the blue and green regions to illuminate the tissue, harnessing the absorption of blood at those wavelengths and creating an image that contrasts vasculature as brown [6]. Condensed vasculature has been associated with lesional tissue due to its invasive, nutrient-draining nature. FICE is an image algorithm that uses the RGB image acquired through normal screenings and processes individual color channels into unique wavelengths (within the respective color range) that accentuates tissue differences greater than the original colored image [8]. This method has defined mucosal irregularities and tissue irritation more effectively than traditional WLE due to post-imaging processing. These techniques are included in aspects of the current architecture (Figure 1).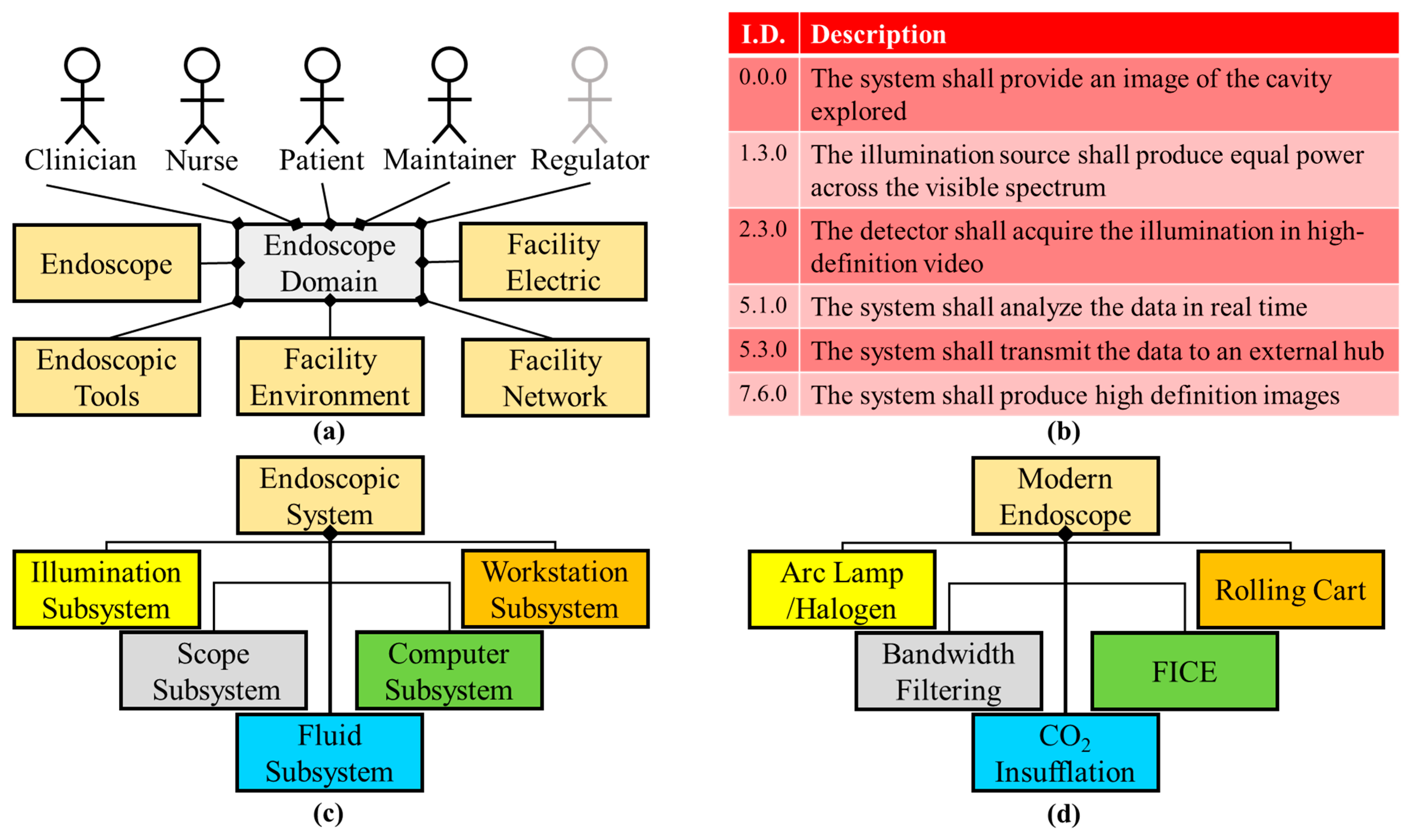
Figure 1. Current endoscope condensed system architecture. (a) The facility network external system was added to the domain diagram of the current system, compared to that of the imaging milestone domain, because of the use of the internet and cloud storage. (b) High-definition and spectral aspects are stated in the requirements for the current system. (c) The logical diagram remains the same as the previous milestone. (d) Physical components and software are bandwidth filters and FICE software for this architecture milestone.
2.1. What’s Trending
Systematic decomposition of previous and existing endoscopic systems highlights the improvements of subsystems and elements within the system, as well as areas for potential upgrades. Here, the current milestone logical architecture is highlighted and the trends in technology are shown for particular subsystems (Figure 2). A primary advancement is the illumination source from candles to incandescent bulbs to LEDs (Figure 2a). Light sources have shown a substantial improvement in luminosity, decreased power consumption, and increased component longevity. Some literature theorizes that illumination technology is reaching maximum potential in white light luminous efficacy [23]. With regard to the computational subsystem, researchers examined the trend in the literature of endoscope-related computer science publications. Researchers searched the Scopus database for publications in the field of computer science using the keywords “gastroenterology” or “endoscopy” and a date range of 1990–2019, divided into five-year increments (Figure 2b). Results indicated that the last two decades have shown a 50X increase in the number of publications fitting these parameters. Examples of the increased computational demand of such components begin with the image sensor digital signal processor (DSP) to convert photons to digital signals [24] and expand to three-dimensional (VE and optical coherence tomography—OCT) [25] and wireless or self-contained (capsule endoscopy) or enhanced channel contrast (FICE). The optical light path which carries illumination to the patient cavity and the image back to the user or imager has also been optimized through the years (Figure 2c). The Lichtleiter with a length of ~10 cm increased to the current colonoscopes with a length over 1.5 m, capable of spanning the entire large intestine and a portion of the small intestine. These depths would not be possible if fiber optics were not introduced, creating flexible endoscopes. Furthermore, a smaller fiber optic bundle and overall endoscopic diameter allowed for the development of smaller systems such as bronchoscopes, cystoscopes, laparoscopes, and ureteroscopes for lungs, bladder, small surgical openings, and ureter, respectively [26]. Flexible endoscopy has not extended the working length further into the small intestine due to the tortuous and compact nature of the organ [27]. Maneuvering a flexible scope through the small intestine could perforate the mucosal lining or damage the fiber optics of the endoscope. Furthermore, the amount of articulation and force that could be applied to the endoscope tip decreases with increased length and depth into the lower GI. Smaller endoscopes are limited in illumination and detection due to size constraints. Therefore, the output of these smaller systems has lower spatial resolution and potentially lower contrast between normal and abnormal tissue.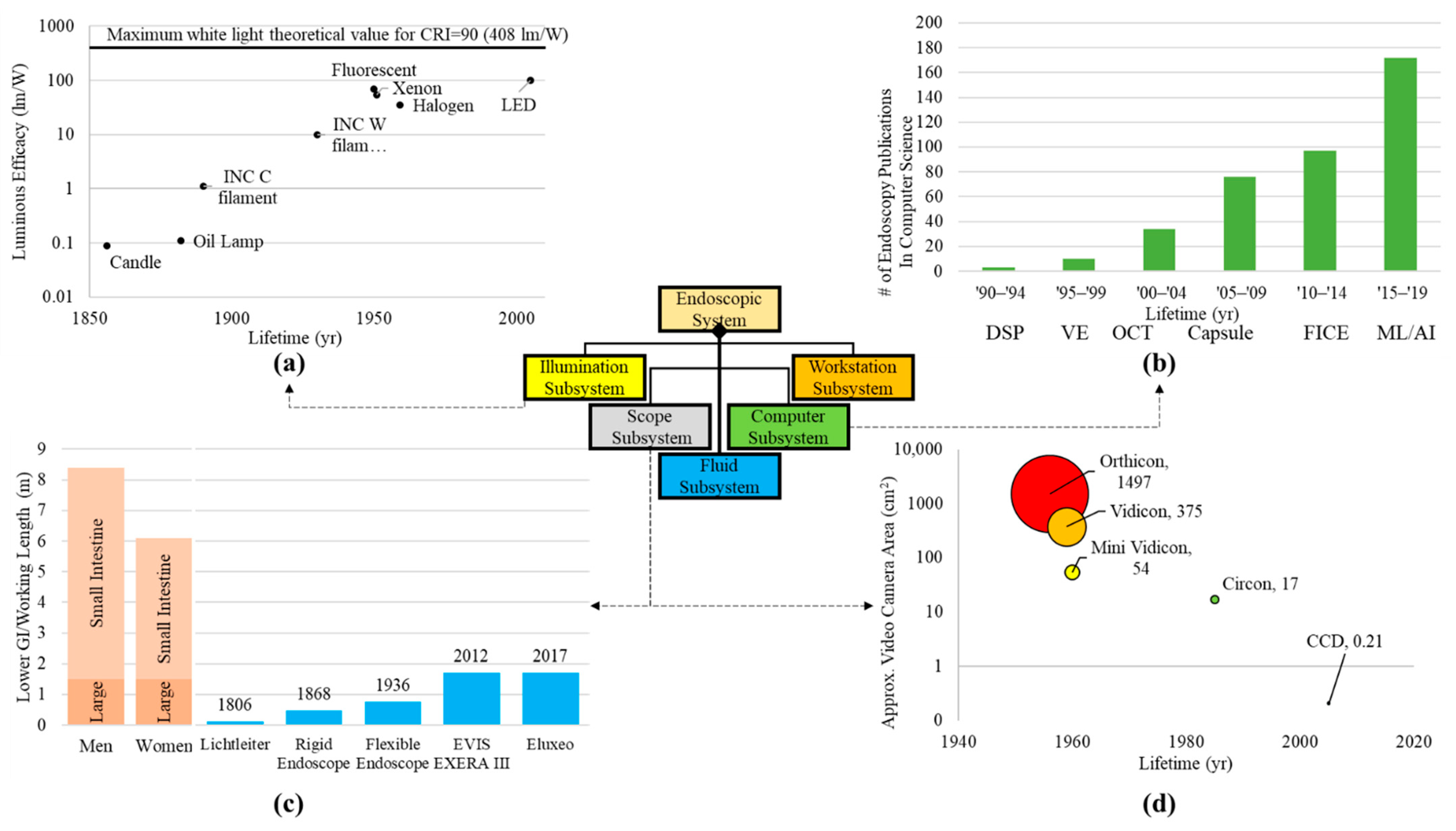
Figure 2. Trends for components within subsystems. (a) Light sources in the illumination subsystem presenting the luminous efficacy from the candle to arc lamps and LEDs. Illumination data were extracted from Azevedo et al.’s paper on solid state lighting [23]. (b) Advancements in computational aspects of endoscope systems were visualized by plotting the increase in endoscope-related publications within the computer science field (publication search for “endoscopy” in the computer science category per quinquennium—Source: http://www.scopus.com, accessed on 28 July 2022) [28]. Some examples of imaging processing technologies that were found include: digital signal processing (DSP), virtual endoscopy (VE), optical coherence tomography (OCT), capsule endoscopy (Capsule), Fujinon’s flexible spectral imaging color enhancement (FICE), and machine learning (ML) [29]. (c) Optical pathway (working length) [30][31][32] for the scope subsystem showing the depth the endoscope has traversed throughout the milestones compared to the length of human body intestinal tract [33]. (d) Approximate camera/detector area for various cameras (both film and digital) throughout imaging in endoscopy. Camera and detector areas were assumed from dimensions given in literature [30][34][35][36][37].
2.2. Endoscopy: The Next Generation
Using systems engineering architecture as a tool for review, researchers can exhaustively survey the needs of the range of subsystems and components, as well as environmental constraints and current technologies. Researchers can predict which technologies may need to evolve and what a next generation endoscope would provide. Based on Figure 2, illumination is at a current maximum, digital sensors can accommodate any endoscope diameter with the caveat of limited resolution for smaller sensor sizes, the working length of the scope cannot get any longer due to highly condensed and tortuous nature of the small intestine and there is a high interest in the computational capabilities of the endoscopic technologies. Reviewing past inventions that were implemented into endoscopy, Figure 3 shows the importance of looking at off-the-shelf components and technology.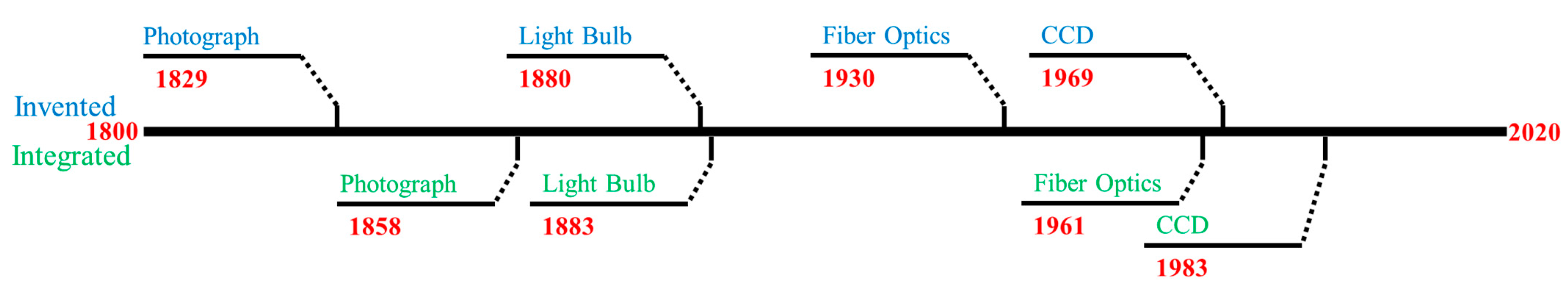
Figure 3. Timeline comparing technology invention dates to the time it was integrated into endoscopy. Blue text denotes invention and green for integration.
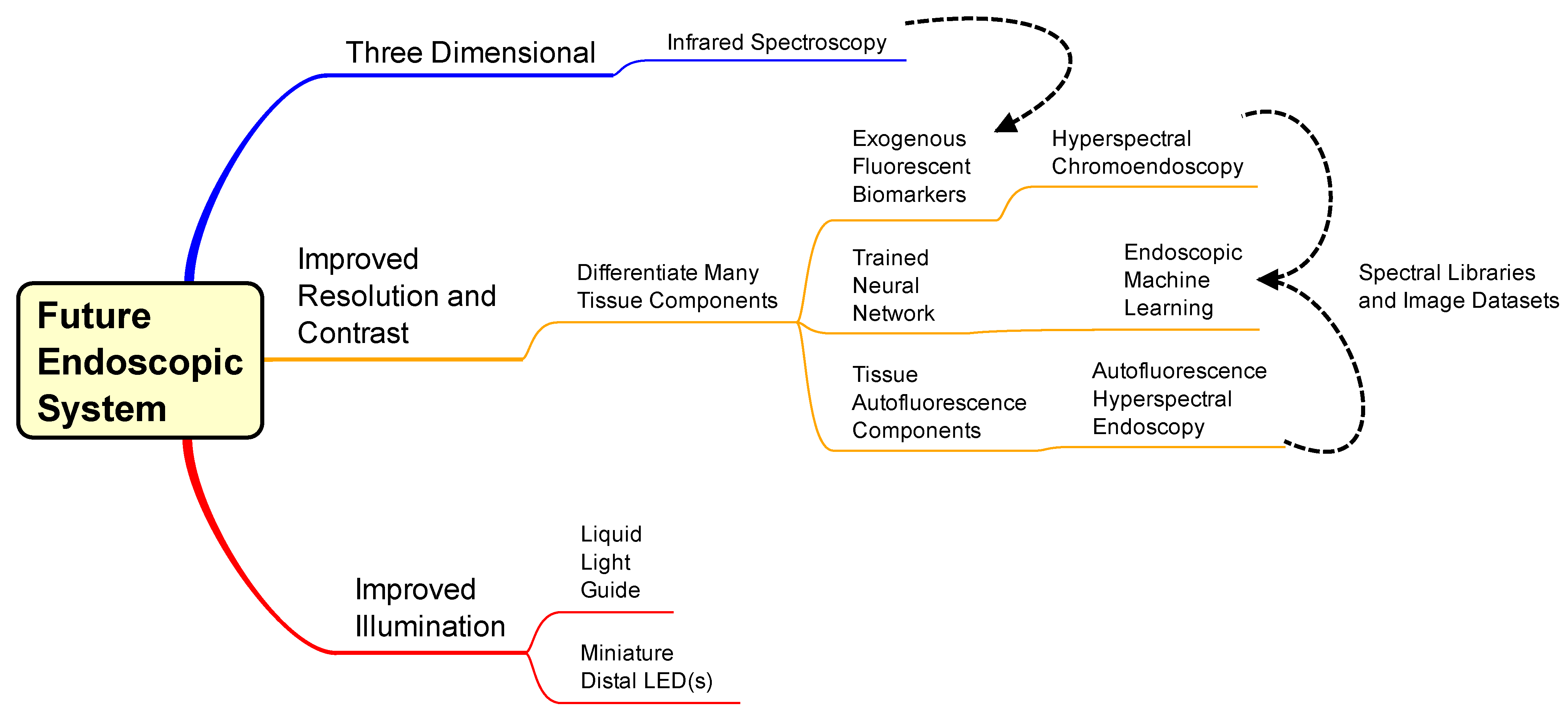
Figure 4. Mind map for design of a next-generation endoscopic system. The middle and top pathways are considerations of techniques to implement, and the bottom pathway is component upgrades of the current endoscope system. Dashed lines convey interconnectivity between topics: Infrared analysis could implement with exogenous fluorescent biomarkers and hyperspectral chromoendoscopy and autofluorescence hyperspectral endoscopy could be analyzed and displayed via machine learning algorithms.
Table 1. Pugh matrix ranking alternative technologies compared to the gold standard (WLE). Metrics for scoring include safety, training, implementation, and added information. The scores are totaled for comparison.
| Safety | Invasive | Patient Comfort | Operational Training |
Example Image Training | Implementation * | Cost to Implement | Additional Image Data |
Higher Contrast | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Current Endoscopy | 4.3 ± 0.7 | 3.0 ± 1.6 | 4.0 ± 1.2 | 4.2 ± 0.7 | 3.7 ± 0.7 | 3.3 ± 1.4 | 2.8 ± 1.5 | 3.5 ± 1.4 | 3.0 ± 1.3 | 17.8 |
| Virtual Endoscopy | 4.7 ± 0.5 | 2.5 ± 1.5 | 4.5 ± 0.5 | 4.0 ± 0.8 | 4.2 ± 0.7 | 3.5 ± 0.8 | 3.5 ± 1.4 | 3.3 ± 1.1 | 3.0 ± 1.5 | 17.8 |
| Capsule Endoscopy | 4.2 ± 0.7 | 2.8 ± 1.2 | 4.0 ± 0.6 | 3.8 ± 0.7 | 4.2 ± 0.7 | 3.2 ± 1.3 | 3.5 ± 0.8 | 3.3 ± 1.1 | 2.8 ± 1.3 | 16.8 |
| Infrared Imaging Endoscopy |
3.7 ± 0.9 | 3.3 ± 1.2 | 4.0 ± 0.8 | 4.2 ± 0.4 | 4.2 ± 0.7 | 4.0 ± 0.8 | 3.8 ± 0.7 | 3.8 ± 0.7 | 3.2 ± 1.2 | 15.2 |
| Autofluorescence Hyperspectral Endoscopy |
4.0 ± 0.8 | 3.3 ± 1.2 | 4.0 ± 0.8 | 4.3 ± 0.7 | 4.7 ± 0.5 | 4.5 ± 0.8 | 3.7 ± 1.5 | 4.2 ± 0.9 | 4.0 ± 1.4 | 15.7 |
| Hyperspectral Chromoendoscopy |
3.8 ± 0.7 | 3.3 ± 1.2 | 4.2 ± 0.9 | 4.5 ± 0.8 | 4.7 ± 0.5 | 4.3 ± 0.7 | 3.8 ± 1.5 | 4.5 ± 0.8 | 4.3 ± 1.1 | 16.2 |
| Neural Network Endoscopy |
4.2 ± 0.9 | 3.5 ± 1.4 | 4.3 ± 0.9 | 4.7 ± 0.5 | 4.2 ± 0.9 | 4.2 ± 1.1 | 3.7 ± 1.9 | 4.2 ± 1.2 | 4.2 ± 1.2 | 16.7 |
References
- Boehm, B.W. A Spiral Model of Software Development and Enhancement. Computer 1988, 21, 61–72.
- Hossain, N.U.I.; Dayarathna, V.L.; Nagahi, M.; Jaradat, R. Systems Thinking: A Review and Bibliometric Analysis. Systems 2020, 8, 23.
- Lieberman, D.A.; Garewal, H. Use of Colonoscopy to Screen Asymptomatic Adults for Colorectal Cancer. N. Engl. J. Med. 2000, 343, 162–168.
- Kaltenbach, T.; Friedland, S.; Soetikno, R. A Randomised Tandem Colonoscopy Trial of Narrow Band Imaging versus White Light Examination to Compare Neoplasia Miss Rates. Gut 2008, 57, 1406.
- Levin, B.; Murphy, G.P. Revision in American Cancer Society Recommendations for the Earlydetection of Colorectal Cancer. CA Cancer J. Clin. 1992, 42, 296–299.
- Chiu, H.-M.; Chang, C.-Y.; Chen, C.-C.; Lee, Y.-C.; Wu, M.-S.; Lin, J.-T.; Shun, C.-T.; Wang, H.-P. A Prospective Comparative Study of Narrow-Band Imaging, Chromoendoscopy, and Conventional Colonoscopy in the Diagnosis of Colorectal Neoplasia. Gut 2007, 56, 373–379.
- Cho, J.-H. Advanced Imaging Technology Other than Narrow Band Imaging. Clin. Endosc. 2015, 48, 503.
- Negreanu, L.; Preda, C.; Ionescu, D.; Ferechide, D. Progress in Digestive Endoscopy: Flexible Spectral Imaging Colour Enhancement (FICE)-Technical Review. J. Med. Life 2015, 8, 416–422.
- Yung, D.E.; Carvalho, P.B.; Giannakou, A.; Kopylov, U.; Rosa, B.; Rondonotti, E.; Toth, E.; Plevris, J.N.; Koulaouzidis, A. Clinical Validity of Flexible Spectral Imaging Color Enhancement (FICE) in Small-Bowel Capsule Endoscopy: A Systematic Review and Meta-Analysis. Endoscopy 2017, 49, 258–269.
- Blachar, A.; Sosna, J. CT Colonography (Virtual Colonoscopy): Technique, Indications and Performance. Digestion 2007, 76, 34–41.
- Bressler, B.; Paszat, L.F.; Chen, Z.; Rothwell, D.M.; Vinden, C.; Rabeneck, L. Rates of New or Missed Colorectal Cancers After Colonoscopy and Their Risk Factors: A Population-Based Analysis. Gastroenterology 2007, 132, 96–102.
- Chung, S.J.; Kim, D.; Song, J.H.; Kang, H.Y.; Chung, G.E.; Choi, J.; Kim, Y.S.; Park, M.J.; Kim, J.S. Comparison of Detection and Miss Rates of Narrow Band Imaging, Flexible Spectral Imaging Chromoendoscopy and White Light at Screening Colonoscopy: A Randomised Controlled Back-to-Back Study. Gut 2014, 63, 785–791.
- Kim, N.H.; Jung, Y.S.; Jeong, W.S.; Yang, H.-J.; Park, S.-K.; Choi, K.; Park, D.I. Miss Rate of Colorectal Neoplastic Polyps and Risk Factors for Missed Polyps in Consecutive Colonoscopies. Intest. Res. 2017, 15, 411–418.
- Siegel, R.; Desantis, C.; Jemal, A. Colorectal Cancer Statistics, 2014. CA Cancer J. Clin. 2014, 64, 104–117.
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30.
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30.
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34.
- Bolin, S.; Nilsson, E.; Sjödahl, R. Carcinoma of the Colon and Rectum--Growth Rate. Ann. Surg. 1983, 198, 151–158.
- Burke, J.R.; Brown, P.; Quyn, A.; Lambie, H.; Tolan, D.; Sagar, P. Tumour Growth Rate of Carcinoma of the Colon and Rectum: Retrospective Cohort Study. BJS Open 2020, 4, 1200–1207.
- Oto, A. Virtual Endoscopy. Eur. J. Radiol. 2002, 42, 231–239.
- Adler, S.N.; Metzger, Y.C. PillCam COLON Capsule Endoscopy: Recent Advances and New Insights. Ther. Adv. Gastroenterol. 2011, 4, 265–268.
- Gossum, A.V.; Fernandez-Urien, I.; Delvaux, M.; Neuhaus, H.; Riccioni, M.E.; Fraser, C.; Hagenmuller, F.; Devière, J. Capsule Endoscopy versus Colonoscopy for the Detection of Polyps and Cancer. N. Engl. J. Med. 2009, 361, 264–270.
- Azevedo, I.L.; Morgan, M.G.; Morgan, F. The Transition to Solid-State Lighting. Proc. IEEE 2009, 97, 481–510.
- Smith, S. The Scientist & Engineer’s Guide to Digital Signal Processing; California Technical Pub: Los Angeles, CA, USA, 1997.
- Tsai, T.-H.; Fujimoto, J.G.; Mashimo, H. Endoscopic Optical Coherence Tomography for Clinical Gastroenterology. Diagnostics 2014, 4, 57–93.
- Gaab, M.R. Instrumentation: Endoscopes and Equipment. World Neurosurg. 2013, 79, S14.e11–S14.e21.
- Swain, P. Role of Video Endoscopy in Managing Small Bowel Disease. Gut 2004, 53, 1866–1875.
- Iakovidis, D.K. Software Engineering Applications in Gastroenterology. Glob. J. Gastroenterol. Hepatol. 2014, 2, 11–18.
- van der Sommen, F.; de Groof, J.; Struyvenberg, M.; van der Putten, J.; Boers, T.; Fockens, K.; Schoon, E.J.; Curvers, W.; de With, P.; Mori, Y.; et al. Machine Learning in GI Endoscopy: Practical Guidance in How to Interpret a Novel Field. Gut 2020, 69, 2035–2045.
- Berci, G.; Forde, K. History of Endoscopy. Surg. Endosc. 2000, 14, 5–15.
- Mann, G.; Bozzini, P.; Bozzini, D. Der Frankfurter Lichtleiter: Neues Über Philipp Bozzini Und Sein Endoskop. Medizinhist. J. 1973, 8, 105–130.
- Rehnberg, V.; Walters, E. The Life and Work of Adolph Kussmaul 1822–1902: ‘Sword Swallowers in Modern Medicine. J. Intensive Care Soc. 2017, 18, 71–72.
- Hounnou, G.; Destrieux, C.; Desme, J.; Bertrand, P.; Velut, S. Anatomical Study of the Length of the Human Intestine. Surg. Radiol. Anat. 2002, 24, 290–294.
- Berci, G.; Davids, J. Endoscopy and Television. Br. Med. J. 1962, 1, 1610–1613.
- Soulas, A.; Dubois De Montreynaud, J.M.; Edwards, R.J.; Gladu, A.J. Bronchoscopy and Television. Dis. Chest 1957, 31, 580–584.
- Berci, G.; Shulman, A.; Morgenstern, L.; Paz-Partlow, M.; Cuschierei, A.; Wood, R. Television Choledochoscopy. Surg. Gynecol. Obstet. 1985, 160, 176–177.
- Baillie, J. The Endoscope. Gastrointest. Endosc. 2007, 65, 886–893.
- Jacobson, M.C.; deVere White, R.W.; Demos, S.G. In Vivo Testing of a Prototype System Providing Simultaneous White Light and near Infrared Autofluorescence Image Acquisition for Detection of Bladder Cancer. J. Biomed. Opt. 2012, 17, 036011.
- McWade, M.A.; Paras, C.; White, L.M.; Phay, J.E.; Solórzano, C.C.; Broome, J.T.; Mahadevan-Jansen, A. Label-Free Intraoperative Parathyroid Localization With Near-Infrared Autofluorescence Imaging. J. Clin. Endocrinol. Metab. 2014, 99, 4574–4580.
- Iseki, K.; Tatsuta, M.; Iishi, H.; Sakai, N.; Yano, H.; Ishiguro, S. Effectiveness of the Near-Infrared Electronic Endoscope for Diagnosis of the Depth of Involvement of Gastric Cancers. Gastrointest. Endosc. 2000, 52, 755–762.
- Ortiz-Fernandez-Sordo, J.; Sami, S.S.; Mansilla-Vivar, R.; Subramanian, V.; Mannath, J.; Telakis, E.; Ragunath, K. Evaluation of a Novel Infra-Red Endoscopy System in the Assessment of Early Neoplasia in Barretts Esophagus: Pilot Study from a Single Center. Dis. Esophagus 2018, 31, dox137.
- Betz, C.S.; Stepp, H.; Janda, P.; Arbogast, S.; Grevers, G.; Baumgartner, R.; Leunig, A. A Comparative Study of Normal Inspection, Autofluorescence and 5-ALA-Induced PPIX Fluorescence for Oral Cancer Diagnosis. Int. J. Cancer 2002, 97, 245–252.
- Zhao, H.L.; Zhang, C.P.; Zhu, H.; Jiang, Y.F.; Fu, X.B. Autofluorescence of Collagen Fibres in Scar. Skin Res. Technol. 2017, 23, 588–592.
- Deal, J.; Mayes, S.; Browning, C.; Hill, S.; Rider, P.; Boudreaux, C.; Rich, T.C.; Leavesley, S.J. Identifying Molecular Contributors to Autofluorescence of Neoplastic and Normal Colon Sections Using Excitation-Scanning Hyperspectral Imaging. J. Biomed. Opt. 2018, 24, 021207.
- Takeuchi, Y.; Hanaoka, N.; Hanafusa, M.; Ishihara, R.; Higashino, K.; Iishi, H.; Uedo, N. Autofluorescence Imaging of Early Colorectal Cancer. J. Biophotonics 2011, 4, 490–497.
- Bae, S.-J.; Lee, D.-S.; Berezin, V.; Kang, U.; Lee, K.-H. Multispectral Autofluorescence Imaging for Detection of Cervical Lesions: A Preclinical Study. J. Obstet. Gynaecol. Res. 2016, 42, 1846–1853.
- Chen, W.; Gao, X.; Tian, Q.; Chen, L. A Comparison of Autofluorescence Bronchoscopy and White Light Bronchoscopy in Detection of Lung Cancer and Preneoplastic Lesions: A Meta-Analysis. Lung Cancer 2011, 73, 183–188.
- Ignjatovic, A.; East, J.; Guenther, T.; Hoare, J.; Morris, J.; Ragunath, K.; Shonde, A.; Simmons, J.; Suzuki, N.; Thomas-Gibson, S. What Is the Most Reliable Imaging Modality for Small Colonic Polyp Characterization? Study of White-Light, Autofluorescence, and Narrow-Band Imaging. Endoscopy 2011, 43, 94–99.
- Falk, G.W. Autofluorescence Endoscopy. Gastrointest. Endosc. Clin. N. Am. 2009, 19, 209–220.
- Becker, A.; Hessenius, C.; Licha, K.; Ebert, B.; Sukowski, U.; Semmler, W.; Wiedenmann, B.; Grötzinger, C. Receptor-Targeted Optical Imaging of Tumors with near-Infrared Fluorescent Ligands. Nat. Biotechnol. 2001, 19, 327–331.
- Guo, Z.; Park, S.; Yoon, J.; Shin, I. Recent Progress in the Development of Near-Infrared Fluorescent Probes for Bioimaging Applications. Chem. Soc. Rev. 2014, 43, 16–29.
More
