Sialadenoma papilliferum (SP) is a rare benign epithelial tumour of salivary gland origin, its diagnosis being potentially challenging. It was first described by Abrams and Finck in 1969 as an analog of the cutaneous syringocystadenoma papilliferum.The aim of this comprehensive review is to highlight the clinical and histopathological diagnostic aspects of intraoral SP, analyzing cases previously described and reporting new ones.
Methods. Medline, Scopus and Web of Science were searched up to February 2022, using as entry term “sialadenoma papilliferum”. No time limits were applied and only studies in English were taken into account. Only cases involving the mouth were included. Conference proceedings, personal communications, letters to editor were excluded.
Results. Forty-two out of 234 articles fulfilled the inclusion criteria, with 64 cases reported.Mean age of patients with SP was 57.2 years with a higher prevalence among males. The most affected site was the palate, particularly the hard palate. Four cases with uncertain malignant features have been reported. While clinical manifestations of SP are rather unspecific (e.g. submucosal swelling with ulceration), histopathological and immunohistochemical features are quite peculiar, SP have a limited growth potential, leading to conservative excision as treatment of choice.
Conclusions. SP, though rare, should be taken into consideration in the differential diagnosis of intraoral swellings, particularly those located on the palate.
- sialadenoma papilliferum
- salivary gland tumors
- oral pathology
- oral medicine
- oral surgery
1. General Introduction
1.1. Age and Sex
1.2. Clinical Features
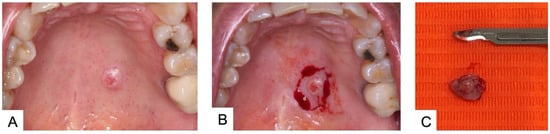
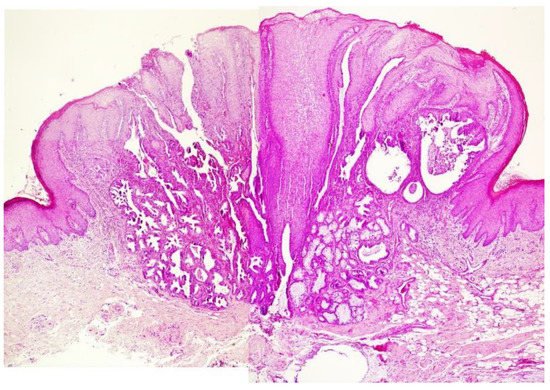
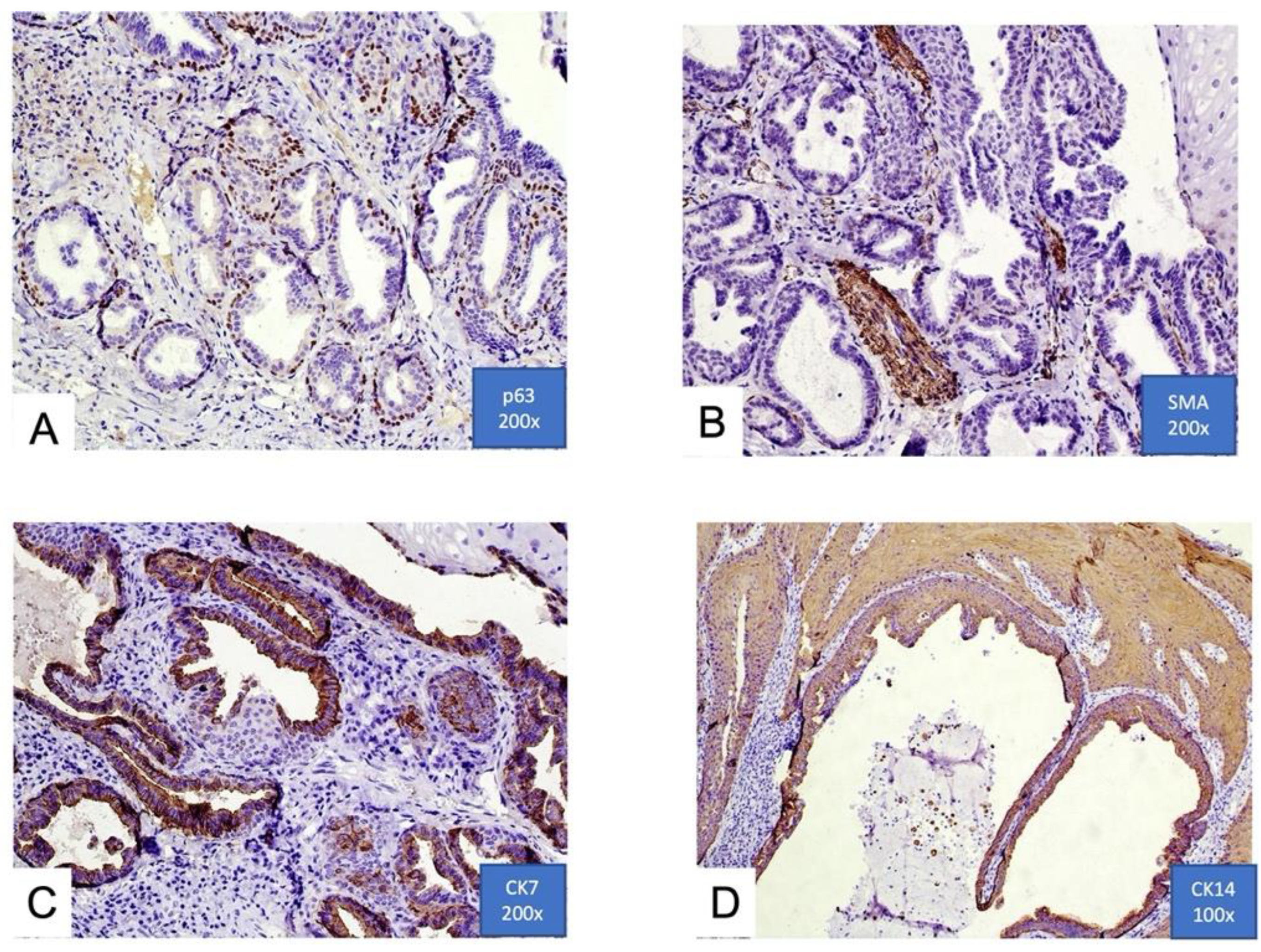
1.3. Histological Features
1.4. Treatment
1.5. Prognosis
1.6. Possible Malignant Transformation
2. Intraoral Sialadenoma Papilliferum
Salivary gland tumors are a morphologically and clinically diverse group of neoplasms that affect predominantly major salivary glands but also are not uncommon in the minor salivary glands. The global annual incidence, when all salivary glands tumors are considered, is approximately 1 case per 100,000 per year [49][13]. Pleomorphic adenoma and mucoepidermoid carcinoma are the two most common benign and malignant minor salivary gland tumors, while SP represents only a small percentage of cases (1.1–1.6%) [3,9][4][20]. A usual difficulty in the management of minor salivary gland tumors is the very heterogeneous clinical and radiographic features, as well as the rather wide range of histopathological subtypes. The exophytic growth pattern of SP is similar to most intraoral salivary gland tumors, which present as submucosal nodular swellings, with or without superficial ulceration. Such a clinic pattern is shared with other lesions, including among others squamous papilloma, verrucous hyperplasia, and exophytic ductal papilloma. Squamous papilloma and verrucous hyperplasia show only squamous epithelial proliferation and thus can be easily differentiated from SP. Exophytic ductal papilloma displays exophytic papillary ductal epithelial proliferation, but it lacks a ductal proliferation underneath the epithelium. Instead, SP shows as unique histopathologic features an exophytic proliferation of papillary stratified squamous epithelium and a contiguously endophytic salivary ductal proliferation underneath [50][21]. SP frequently presents as an erythematous lesion, with ulceration or erosion that may suggest a malignant lesion, such as verrucous carcinoma or even sarcomas [38][22]. From the epidemiological point of view, age and gender are not very helpful in the differential diagnosis, as most salivary gland tumors have no gender predilection and the mean age found in the present revisewarch for SP is similar to that reported for other salivary gland tumors (45 years, with a range of 11–74) [51][23]. SP appears to have a limited growth potential, with an average size at diagnosis of 0.79 cm, facilitating a conservative surgical treatment. There are insufficient data to support the malignant potential of SP, although four cases of supposed malignant transformation were reported. Research is currently focused to determine the cells of origin of SP, but despite immunohistochemical studies, such question remain unanswered. In conclusion SP, though rare, should be taken into consideration in the differential diagnosis of intraoral swellings, particularly those located on the palate, and more studies are necessary to better understand its biology.References
- Abrams, A.M.; Finck, F.M. Sialadenoma papilliferum: A previously un-reported salivary gland tumor. Cancer 1969, 24, 1057–1063.
- Loehn, B.; Sutton, C.; Jastram-Belcher, J.; Harton, A.; Anderson, D.; Walvekar, R.R. Sialadenoma papilliferum of the parotid gland: Case report and review of literature. Head Neck 2013, 35, E74–E76.
- Fowler, C.B.; Damm, D.D. Sialadenoma Papilliferum: Analysis of Seven New Cases and Review of the Literature. Head Neck Pathol. 2018, 12, 193–201.
- Freedman, P.D.; Lumerman, H. Sialoadenoma papilliferum. Oral Surg. 1978, 45, 88–94.
- Solomon, M.P.; Rosen, Y.; Alfonso, A. Intraoral papillary squamous cell tumor of the soft palate with features of sialadenoma papilliferum? Malignant sialadenoma papilliferum. Cancer 1978, 42, 1859–1869.
- Mccoy, J.M.; Eckert, J.R.E.F. Sialoadenoma papilliferum. J. Oral Surg. 1980, 38, 691–693.
- Nasu, M.; Takagi, M.; Ishikawa, G. Sialoadenoma papilliferum. Report of a case. J. Oral Surg. 1981, 39, 367–369.
- Fantasia, J.E.; Nocco, C.E.; Lally, E.T. UItrastructureof sialadenoma papilliferum. Arch. Pathol. Lab. Med. 1986, 110, 523–527.
- Maiorano, E.; Favia, G.; Ricco, R. Sialadenoma papilliferum: An immunohistochemical study of five cases. J. Oral Pathol. Med. 1996, 25, 336–342.
- Ubaidat, M.A.; Robinson, R.A.; Belding, P.J.; Merryman, D.J. Sialadenoma papilliferum of the hard palate: Report of 2 cases and immunohistochemical evaluation. Arch. Pathol. Lab. Med. 2001, 125, 1595–1597.
- Gomes, A.P.; Sobral, A.P.; Loducca, S.V.; de Araujo, V.C. Sialadenoma papilliferum: Immunohistochemical study. Int. J. Oral Maxillofac. Surg. 2004, 33, 621–624.
- Atarbashi-Moghadam, S.; Lotfi, A.; Moshref, M.; Mokhtari, S. Sialadenoma papilliferum of the hard palate: A rare case report. Indian J. Pathol. Microbiol. 2019, 62, 163–164.
- Melo, G.M.; Cervantes, O.; Abrahao, M.; Covolan, L.; Ferreira, E.S.; Baptista, H.A. A brief history of salivary gland surgery. Rev. Colégio Bras. Cir. 2017, 44, 403–412.
- Van der Wal, J.E.; Van der Waal, I. The rare sialadenoma papilliferum: Report of a case and review of the literature. Int. J. Oral Maxillofac. Surg. 1992, 21, 104–106.
- Rennie, J.S.; MacDonald, D.G.; Critchlow, H.A. Sialadenoma papilliferum. A case report and review of the literature. Int. J. Oral Surg. 1984, 13, 452–454.
- Pimentel, M.T.; Lopez Amado, M.; Garcia, S.A. Recurrent sialadenoma papilliferum of the buccal mucosa. J. Laryngol. Otol. 1995, 109, 787–790.
- Ide, F.; Kikuchi, K.; Kusama, K.; Kanazawa, H. Sialadenoma papilliferum with potentially malignant features. J. Clin. Pathol. 2010, 63, 362–364.
- Santos, J.N.; Barros, A.C.; Gurgel, C.A.; Ramalho, L.M.P. Sialadenoma papilliferum of the tongue mimicking a malignant tumor. Braz. J. Otorhinolaryngol. 2013, 79, 404.
- Shimoda, M.; Kameyama, K.; Morinaga, S.; Tanaka, Y.; Hashiguchu, K.; Shimada, M.; Okara, Y. Malignant transformation of sialadenoma papilliferum of the palate: A case report. Virchows Arch. 2004, 445, 641–646.
- Waldron, C.A.; El-Mofty, S.K.; Gnepp, D.R. Tumors of the intraoral minor salivary glands: A demographic and histologic study of 426 cases. Oral Surg. Oral Med. Oral Pathol. 1988, 66, 323–333.
- Hsieh, M.S.; Bishop, J.A.; Yu Fong Chang, J. Sialadenoma Papilliferum. Surg. Pathol. Clin. 2021, 14, 43–51.
- Anuradha, A.; Ram Prasad, V.V.; Kashyap, B.; Srinivas, V. Sialadenoma papilliferum: Clinical misdiagnosis with a histological decree. Case Rep. Dent. 2012, 2012, 356271.
- Vaidya, A.D.; Pantvaidya, G.H.; Metgudmath, R.; Kane, S.V.; D’Cruz, A.K. Minor salivary gland tumors of the oral cavity: A case series with review of literature. J. Cancer Res. Ther. 2012, 8 (Suppl. S1), S111–S115.
