Interleukin-11 (IL11), a stromal-cell derived pleiotropic cytokine with profibrotic and cellular remodeling properties, as a potential biomarker in non-small cell lung cancer (NSCLC). IL11 is an important tumor-promoting cytokine that that has both diagnostic and prognostic value in patients with NSCLC. Multiple in vitro studies confirm that IL11 activates known tumor-promoting signaling pathways and clinical studies link increased IL11 expression to poorer prognosis.
- interleukin-11
- cytokines
- non-small cell lung cancer
- biomarkers
1. Interleukin-11: Member of the IL6 Family of Cytokines
| Cytokine | Receptors | References | |||||||
|---|---|---|---|---|---|---|---|---|---|
| IL6 | IL6R, gp130/IL6ST | [15, | ] | 16, | [ | 17,18, | 8][9][10] | 19,20,21,22] | [7[11][12][13][14] |
| IL-31 | IL31Rα, OSMR | [23] | [15] | ||||||
| LIF | LIFR/LIFRα, gp130/IL6ST | [24] | [16] | ||||||
| OSM | OSMR/OSMRβ, gp130/IL6ST, LIFR | [25, | [17 | 26] | ][18] | ||||
| CLCF1 | CNTFR, LIFR, gp130/IL6ST | [22,27] | [14][19] |
2. Interleukin 11 Drives Pulmonary Fibrosis and Inflammation
IL11 was initially implicated in several inflammatory lung diseases such as asthma and tuberculosis infection. However, recent evidence has demonstrated that IL11 is an important determinant of fibrosis and chronic inflammation in the lung (reviewed in [28])[20]. Pulmonary epithelial cells and fibroblasts express high levels of IL11RA and are prominent cellular sources of IL11 in response to respiratory infections. Hence, it is proposed that IL11 acts in an autocrine/paracrine fashion in response to pathogens or after tissue injury. IL11 is upregulated in pulmonary fibroblasts from patients with idiopathic pulmonary fibrosis (IPF), a form of progressive fibrosing interstitial pneumonia characterized by an excess of activated myofibroblasts, and its elevated expression in the IPF lung is associated with fibrosis and disease severity [29][21]. In vitro studies on non-transformed pulmonary cells showed that IL11 triggers the proliferation and transformation of quiescent fibroblasts into collagen-producing invasive myofibroblasts [29][21], and induces an EMT program in epithelial cells. Pharmacological inhibition of IL11 or fibroblast-specific blockade of IL11 signaling reduced fibroblast invasion in vitro and reversed pulmonary fibrosis and inflammation in a murine model of IPF [29,30][21][22].3. Interleukin 11 Is a Tumor-Promoting Cytokine in NSCLC
IL11 was first isolated in 1990 from a primate bone marrow-derived stromal cell line and was identified to possess hematopoietic and thrombopoietic properties [33][23]. Subsequently, IL11 was evaluated as a potential therapy for chemotherapy-induced thrombocytopenia among cancer patients [34,35][24][25]. The need to determine suitability of IL11 treatment for thrombocytopenia in cancer patients motivated early studies evaluating its effects on cancer cells. Early studies involving lung cancer cells concluded that IL11 did not promote tumor cell growth. Soda et al. harvested tumor cells from a heterogenous group of clinical specimens and subjected the cells to recombinant human IL11 (rhIL11) [36].[26], Twhis study dch defined tumor growth stimulation as a >150% survival increase in tumor colony-forming units and found that 97% of the specimens across a variety of cancers tested were not stimulated by rhIL11. Saitoh et al. utilized a murine model of lung cancer and showed that rhIL11 inhibited proliferation in vitro while not affecting the anti-tumor effects of carboplatin, mitomycin and etoposide in mice [37][27]. Treating Calu-1 cells, a NSCLC epithelial cell line, with IL11 seemed to reduce DNA synthesis but not significantly [38][28]. Taken together, these early studies suggest that IL11 was more likely an inhibitor, rather than a stimulator, of tumor growth. Later studies, however, identified IL11 as a tumor-promoting cytokine instead [39,40,41,42][29][30][31][32]. It is now known that rhIL11 does not activate mouse IL11 receptor (IL11RA), but competitively inhibits binding of endogenous murine IL11 instead [43,44][33][34]. Hence, the use of rhIL11 on murine lung cancer is not expected to recapitulate the effect of human IL11 on human lung cancer. It is likely due to the differential effects of cross- and same-species recombinant IL11 that a later study utilizing same-species rhIL11 concluded IL11 to be tumor promoting [45][35], while an earlier study that used cross-species rhIL11 concluded otherwise [37][27]. Zhao et al. provided direct evidence that IL11 promotes tumor growth using lentivirus-mediated IL11 overexpression and knockout in A549 and H1299 lung cancer cell lines [46][36]. IL11 signaling can occur either via classical signaling or trans-signaling. During classical signaling, IL11 binds to its specific receptor IL11RA, which leads to dimerization of the signal transducing gp130 subunit and activation of downstream signaling. IL11RA is differentially expressed in NSCLC and has been targeted in a preclinical study to reduce tumor growth [58][37]. In trans-signaling, soluble IL11RA are generated from mRNA splice variants or from proteolytic cleavage of the membrane-bound receptor complexing with the cytokine extracellularly [59][38]. This complex then binds to any gp130, which is ubiquitously expressed on cell surfaces, without requiring the cytokine-specific receptor potentially expanding the repertoire of effector cells. IL6 trans-signaling has been reported to be important in KRAs-driven NSCLC [60][39], but it is yet uncertain whether IL11 functions similarly. Downstream of cytokine-receptor binding, JAK/STAT [39[29][30][40],40,61], PI3K/AKT, and Ras/ERK pathways can be activated resulting in cell proliferation, inhibition of pro-apoptotic proteins, activation of anti-apoptosis proteins, and angiogenesis [62,63][41][42]. Activation of these pathways has been proposed as a prognostic outcome predictor for NSCLC [64,65,66,67][43][44][45][46].4. Sources of Biomarkers in NSCLC
Biomarkers are measurable characteristics of normal and pathogenic processes or exposure to interventions [74][47]. Sources for molecular biomarkers in NSCLC may include peripheral blood, bronchoalveolar lavage, breath exudate, lung tissue, pleural fluid, urine, sputum and saliva. These sources differ in feasibility, reproducibility, and procedural risk profile. Peripheral blood is readily accessible and is useful for comparisons between healthy, disease and treated populations and is also suitable in longitudinal studies measuring response to therapy. However, the sensitivity, specificity and reproducibility of blood biomarkers is limited by production by sources other than tumor, volume of distribution, and biomarker metabolism and turnover. Alternatively, molecular biomarkers identified via lung tumor tissue most directly reflect true tumor biology. However, procurement of tissue samples requires invasive methods such as diagnostic biopsy samples, post-mortem collection, or from surgical resection. Specimens from surgical resection provide the greatest quantity of tumor tissue and allows adjacent histologically normal tissue to be collected concurrently for comparisons.5. IL11 Differential Expression in NSCLC Tumor Tissue
The Cancer Genome Atlas (TCGA) database is a commonly referenced publicly accessible dataset containing RNAseq data for tumor samples from NSCLC patients, including a proportion of matched adjacent normal samples [75][48]. The Genotype-Tissue Expression (GTEx) project is a publicly available resource that provides genotype and expression data for tissue from different sources, including those from non-cancerous lung [76][49]. Based on the UCSC Xena platform [77[50][51],78], which utilizes these datasets collectively, IL11 mRNA expression is elevated in tumor tissues as compared to adjacent normal or tissues from donors without lung cancer (Figure 1).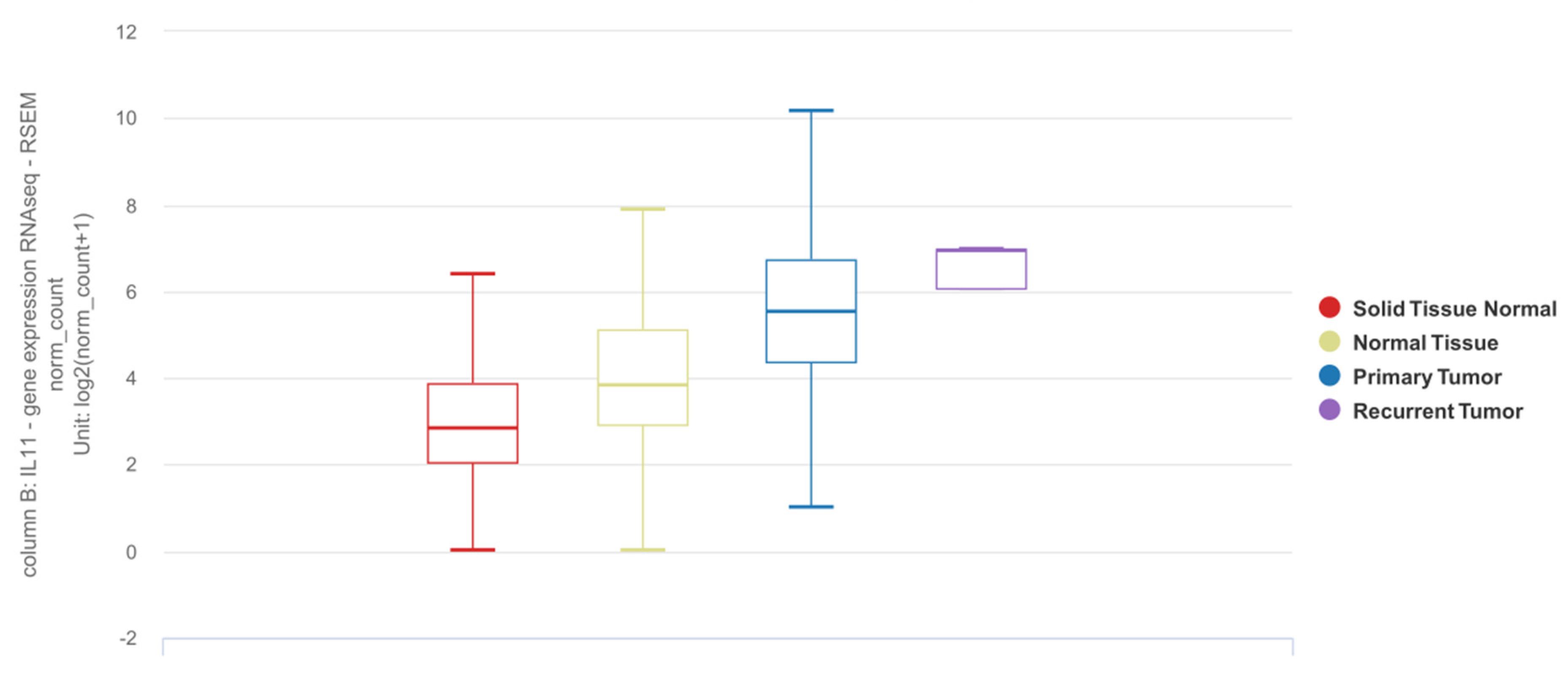
6. Detection of IL11 for Diagnosis of NSCLC
To the best of ourthe knowledge, there are two studies that describe the utility of IL11 as a diagnostic biomarker (Table 2). Pastor et al. recruited a prospective cohort of 369 patients for which use of diagnostic biomarkers in bronchoalveolar lavage fluid (BALF) can potentially facilitate early detection of lung cancer [90][52]. Among 80 cytokines and growth factors, inflammation-related protein array analyses identified IL11 expression to be differentially increased in LUAD BALF samples in an initial discovery cohort, and subsequently validated in two separate exploratory and diagnostic cohorts. This study demonstrated that BALF IL11 expression was largely restricted to patients with LUAD, with or without chronic obstructive pulmonary disease (COPD). Despite the eventual diagnosis at stage III or IV in the majority of the LUAD cohort, the diagnostic performance of BALF IL11 remains similar between the subgroups even for the early stages. Interestingly, BALF IL11 expression was not increased in squamous cell carcinoma (SCC), a type of NSCLC of epithelial origin, which may suggest cell type-selective IL11 expression in NSCLC. In another study, Wu et al. measured IL11 protein concentration in serum and exhaled breath condensate in NSCLC cases compared to healthy donors and found increased IL11 expression in NSCLC patients even at early-stage disease [91][53].
| Study | Recruited Population | Comparison | Sample Type | Diagnostic Biomarker | Assay | Receiver Operator Curve and Test Metrics | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC (95% CI) |
Cutoff (pg/mL) | Sensitivity (95% CI) |
Specificity (95% CI) | PPV (95% CI) |
NPV (95% CI) |
||||||
| Pastor et al. [90] | Pastor et al. [52] | Age > 40 yrs, current or ex-smokers of 30 pack-years, evaluated for hemoptysis or pulmonary nodule or mass, excluding those with prior diagnosis of malignancy, active tuberculosis, history of drug abuse or other inflammatory disease apart from COPD | LUAD vs. non-LUAD—First validation cohort (n = 149) | BALF | IL11 protein | ELISA | 0.93 (0.90–0.97) | 42.0 | |||
| 78.1 | |||||||||||
| 79.4 | NR | NR | |||||||||
7. Quantification of IL11 Expression for Prognostication of NSCLC
Accurate prognostication is important for identifying patients who may benefit from adjuvant or neoadjuvant therapy. Using molecular biomarkers in addition to clinical data can potentially allow patients to be stratified into risk groups with greater accuracy [106,107][54][55]. Numerous studies have identified IL11 mRNA in NSCLC lung tissue taken at the time of surgical resection to be prognostic of overall survival, both by itself and among other genes as part of a prognostic signature (summarized in Table 43).
| Study | Year | Training Cohort | Validation Cohort (s) | Cancer Type | Prognostic Signature | Findings | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 90.2 (79–95.7) | 88.7 (90.6–93.5) | ||||||||||||||||||||||||||||
| Kratz et al. [107] | Kratz et al. [55] | 2012 | Non-squamous NSCLC (n = 361) | Stage I non-squamous NSCLC (n = 433), and stage I-III non-squamous NSCLC (n = 1006) | Non-squamous NSCLC | 11 Target genes ( | BAG1 | , | BRCA1 | , | CDC6 | , 80.7 (68.7–88.9) | CDK2AP1 | , | ERBB3 | , | FUT3 | , | IL11 | , | LCK | ) and 3 reference genes ( | ESD | , | TBP | , 94.5 (87.8–97.6) | |||
| YAP1 | ) |
|
| LUAD vs. non-LUAD—Second validation cohort (n = 160) | BALF | IL11 protein | ELISA | 0.95 (0.92–0.98) | 42.0 | 90.6 (79.7–95.9) | 83.0 (86.8–87.7) | 60.8 (49.7–70.8) | 96.8 (92.7–98.6) | ||||||||||||||||
| Watza et al. [108] | Watza et al. [56] | 2018 | NSCLC patients without history of bronchiectasis or cystic fibrosis (n = 280) | TCGA Lung SCC and TCGA LUAD datasets (n = 1026) | NSCLC | 23 genes involved in the interleukin signaling pathway, including | IL11 |
| Wu et al. [91] | Wu et al. [53] | NSCLC patients with no history of radiochemotherapy, immune-targeted therapy or surgery (n = 91 for serum, of which 63 have LUAD and 28 have SCC; 64 for EBC) | Healthy volunteers without acute or chronic infectious diseases, vital organ diseases, or genetic family tumor history (n = 72 for serum; 63 for EBC) | Serum | IL11 protein | ELISA | ||||||||||||||
| Wang et al. [79] | Wang et al. | 0.93 (0.88–0.97) | [57] | 2020 | TCGA LUAD dataset (497 LUAD tissues, 54 normal lung tissues) | n/a | LUAD | 6 genes ( | CRABP1 | , | IGKV4-1 | , | IL11 | , | INHA | , | LGR4 | , | VIPR1 | ) |
| 126.1 | 75.0 | 100.0 | NR |
| NR | ||
|
|
| EBC | IL11 protein | |||||||||||||||||||||||||
| Fan et al. [109] | Fan et al. [58] | 2021ELISA | TGCA LUAD dataset (n = 464)(majority stage I and II)0.78 (0.69–0.86) | GSE13213 (n = 117), GSE30219 (n = 85), GSE31210 (n = 226), GSE72094 (n = 420)(majority stage I and II)21.5 | LUAD | 5 genes ( | IL7R | , | IL5RA | , | IL20RB | , | IL11 | , | IL22RA1 | ) |
| ||||||||||||
| Chen et al. [110] | Chen et al. [59] | 2021 | TCGA LUAD (535 LUAD tissues, 59 normal lung tissues)GSE161116 (9 LUAD tissues, 9 LUAD brain metastasis tissues) | n/a | LUAD | 6 genes ( | TNFRSF11A | , | MS4A2 | , | IL11 | , | CAMP | , | MS4A1 | , | F2RL1 | ) |
| ||||||||||
| Peng et al. [111] | Peng et al. [60] | 2021 | GSE161116 (13 lung tumor tissues, 15 brain tissues), GSE747706 (18 lung tumor tissues, 18 normal tissues), GSE21933 (21 lung tumor tissues, 21 normal tissues) datasets | n/a | NSCLC andBrain tumor | n/a |
|
References
- Metcalfe, R.D.; Putoczki, T.L.; Griffin, M.D.W. Structural Understanding of Interleukin 6 Family Cytokine Signaling and Targeted Therapies: Focus on Interleukin 11. Front. Immunol. 2020, 11, 1424.
- Rose-John, S. Interleukin-6 Family Cytokines. Cold Spring Harb. Perspect. Biol. 2018, 10, a028415.
- van Duijneveldt, G.; Griffin, M.D.W.; Putoczki, T.L. Emerging Roles for the IL-6 Family of Cytokines in Pancreatic Cancer. Clin. Sci. 2020, 134, 2091–2115.
- Felcher, C.M.; Bogni, E.S.; Kordon, E.C. IL-6 Cytokine Family: A Putative Target for Breast Cancer Prevention and Treatment. Int. J. Mol. Sci. 2022, 23, 1809.
- Unver, N.; McAllister, F. IL-6 Family Cytokines: Key Inflammatory Mediators as Biomarkers and Potential Therapeutic Targets. Cytokine Growth Factor Rev. 2018, 41, 10–17.
- Jones, S.A.; Jenkins, B.J. Recent Insights into Targeting the IL-6 Cytokine Family in Inflammatory Diseases and Cancer. Nat. Rev. Immunol. 2018, 18, 773–789.
- Xu, B.; Chen, Q.; Yue, C.; Lan, L.; Jiang, J.; Shen, Y.; Lu, B. Prognostic Value of IL-6R mRNA in Lung Adenocarcinoma and Squamous Cell Carcinoma. Oncol. Lett. 2018, 16, 2935–2948.
- Silva, E.M.; Mariano, V.S.; Pastrez, P.R.A.; Pinto, M.C.; Castro, A.G.; Syrjanen, K.J.; Longatto-Filho, A. High Systemic IL-6 Is Associated with Worse Prognosis in Patients with Non-Small Cell Lung Cancer. PLoS ONE 2017, 12, e0181125.
- Liao, C.; Yu, Z.; Guo, W.; Liu, Q.; Wu, Y.; Li, Y.; Bai, L. Prognostic Value of Circulating Inflammatory Factors in Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Cancer Biomark. 2014, 14, 469–481.
- De Vita, F.; Orditura, M.; Auriemma, A.; Infusino, S.; Roscigno, A.; Catalano, G. Serum Levels of Interleukin-6 as a Prognostic Factor in Advanced Non-Small Cell Lung Cancer. Oncol. Rep. 1998, 5, 649–652.
- Meaney, C.L.; Zingone, A.; Brown, D.; Yu, Y.; Cao, L.; Ryan, B.M. Identification of Serum Inflammatory Markers as Classifiers of Lung Cancer Mortality for Stage I Adenocarcinoma. Oncotarget 2017, 8, 40946–40957.
- Song, L.; Smith, M.A.; Doshi, P.; Sasser, K.; Fulp, W.; Altiok, S.; Haura, E.B. Antitumor Efficacy of the Anti-Interleukin-6 (IL-6) Antibody Siltuximab in Mouse Xenograft Models of Lung Cancer. J. Thorac. Oncol. 2014, 9, 974–982.
- Keegan, A.; Ricciuti, B.; Garden, P.; Cohen, L.; Nishihara, R.; Adeni, A.; Paweletz, C.; Supplee, J.; Jänne, P.A.; Severgnini, M.; et al. Plasma IL-6 Changes Correlate to PD-1 Inhibitor Responses in NSCLC. J. Immunother Cancer 2020, 8, e000678.
- Vicent, S.; Sayles, L.C.; Vaka, D.; Khatri, P.; Gevaert, O.; Chen, R.; Zheng, Y.; Gillespie, A.K.; Clarke, N.; Xu, Y.; et al. Cross-Species Functional Analysis of Cancer-Associated Fibroblasts Identifies a Critical Role for CLCF1 and IL-6 in Non-Small Cell Lung Cancer in Vivo. Cancer Res. 2012, 72, 5744–5756.
- Yang, Y.; Li, L.; Chen, F.; Zhang, L.; Bu, H. The Role of Interleukin-31 Polymorphisms in Non-Small Cell Lung Cancer Genetic Susceptibility and Clinical Outcome. Genet. Test. Mol. Biomark. 2018, 22, 314–319.
- Wang, H.; Si, S.N.; Jiang, M.; Chen, L.; Huang, K.; Yu, W. Leukemia Inhibitory Factor Is Involved in the Pathogenesis of NSCLC through Activation of the STAT3 Signaling Pathway. Oncol. Lett. 2021, 22, 663.
- Chen, D.; Chu, C.-Y.; Chen, C.-Y.; Yang, H.-C.; Chiang, Y.-Y.; Lin, T.-Y.; Chiang, I.-P.; Chuang, D.-Y.; Yu, C.-C.; Chow, K.-C. Expression of Short-Form Oncostatin M Receptor as a Decoy Receptor in Lung Adenocarcinomas. J. Pathol. 2008, 215, 290–299.
- Shien, K.; Papadimitrakopoulou, V.A.; Ruder, D.; Behrens, C.; Shen, L.; Kalhor, N.; Song, J.; Lee, J.J.; Wang, J.; Tang, X.; et al. JAK1/STAT3 Activation through a Proinflammatory Cytokine Pathway Leads to Resistance to Molecularly Targeted Therapy in Non-Small Cell Lung Cancer. Mol. Cancer Ther. 2017, 16, 2234–2245.
- Kim, J.W.; Marquez, C.P.; Kostyrko, K.; Koehne, A.L.; Marini, K.; Simpson, D.R.; Lee, A.G.; Leung, S.G.; Sayles, L.C.; Shrager, J.; et al. Antitumor Activity of an Engineered Decoy Receptor Targeting CLCF1-CNTFR Signaling in Lung Adenocarcinoma. Nat. Med. 2019, 25, 1783–1795.
- Ng, B.; Cook, S.A.; Schafer, S. Interleukin-11 Signaling Underlies Fibrosis, Parenchymal Dysfunction, and Chronic Inflammation of the Airway. Exp. Mol. Med. 2020, 52, 1871–1878.
- Ng, B.; Dong, J.; D’Agostino, G.; Viswanathan, S.; Widjaja, A.A.; Lim, W.-W.; Ko, N.S.J.; Tan, J.; Chothani, S.P.; Huang, B.; et al. Interleukin-11 Is a Therapeutic Target in Idiopathic Pulmonary Fibrosis. Sci. Transl. Med. 2019, 11, eaaw1237.
- Ng, B.; Dong, J.; Viswanathan, S.; Widjaja, A.A.; Paleja, B.S.; Adami, E.; Ko, N.S.J.; Wang, M.; Lim, S.; Tan, J.; et al. Fibroblast-Specific IL11 Signaling Drives Chronic Inflammation in Murine Fibrotic Lung Disease. FASEB J. 2020, 34, 11802–11815.
- Paul, S.R.; Bennett, F.; Calvetti, J.A.; Kelleher, K.; Wood, C.R.; O’Hara, R.M., Jr.; Leary, A.C.; Sibley, B.; Clark, S.C.; Williams, D.A. Molecular Cloning of a cDNA Encoding Interleukin 11, a Stromal Cell-Derived Lymphopoietic and Hematopoietic Cytokine. Proc. Natl. Acad. Sci. USA 1990, 87, 7512–7516.
- Tepler, I.; Elias, L.; Smith, J.W., 2nd; Hussein, M.; Rosen, G.; Chang, A.Y.; Moore, J.O.; Gordon, M.S.; Kuca, B.; Beach, K.J.; et al. A Randomized Placebo-Controlled Trial of Recombinant Human Interleukin-11 in Cancer Patients with Severe Thrombocytopenia due to Chemotherapy. Blood 1996, 87, 3607–3614.
- Xu, Y.; Song, X.; Du, F.; Zhao, Q.; Liu, L.; Ma, Z.; Lu, S. A Randomized Controlled Study of rhTPO and rhIL-11 for the Prophylactic Treatment of Chemotherapy-Induced Thrombocytopenia in Non-Small Cell Lung Cancer. J. Cancer 2018, 9, 4718–4725.
- Soda, H.; Raymond, E.; Sharma, S.; Lawrence, R.; Cerna, C.; Gomez, L.; Schaub, R.; Von Hoff, D.D.; Izbicka, E. Recombinant Human Interleukin-11 Is Unlikely to Stimulate the Growth of the Most Common Solid Tumors. Anticancer Drugs 1999, 10, 97–101.
- Saitoh, M.; Taguchi, K.; Momose, K.; Suga, K.; Yamazaki, N.; Ono, C.; Suzuki, T.; Takeuchi, O.; Yasuda, S.; Miyata, K. Recombinant Human Interleukin-11 Improved Carboplatin-Induced Thrombocytopenia without Affecting Antitumor Activities in Mice Bearing Lewis Lung Carcinoma Cells. Cancer Chemother. Pharmacol. 2002, 49, 161–166.
- Spence, M.J.; Streiff, R.; Day, D.; Ma, Y. Oncostatin M Induces Tissue-Type Plasminogen Activator and Plasminogen Activator Inhibitor-1 in Calu-1 Lung Carcinoma Cells. Cytokine 2002, 18, 26–34.
- Howlett, M.; Giraud, A.S.; Lescesen, H.; Jackson, C.B.; Kalantzis, A.; Van Driel, I.R.; Robb, L.; Van der Hoek, M.; Ernst, M.; Minamoto, T.; et al. The Interleukin-6 Family Cytokine Interleukin-11 Regulates Homeostatic Epithelial Cell Turnover and Promotes Gastric Tumor Development. Gastroenterology 2009, 136, 967–977.
- Wang, D.; Zheng, X.; Fu, B.; Nian, Z.; Qian, Y.; Sun, R.; Tian, Z.; Wei, H. Hepatectomy Promotes Recurrence of Liver Cancer by Enhancing IL-11-STAT3 Signaling. EBioMedicine 2019, 46, 119–132.
- Ma, J.; Song, X.; Xu, X.; Mou, Y. Cancer-Associated Fibroblasts Promote the Chemo-Resistance in Gastric Cancer through Secreting IL-11 Targeting JAK/STAT3/Bcl2 Pathway. Cancer Res. Treat. 2019, 51, 194–210.
- Wang, X.; Che, X.; Liu, C.; Fan, Y.; Bai, M.; Hou, K.; Shi, X.; Zhang, X.; Liu, B.; Zheng, C.; et al. Cancer-Associated Fibroblasts-Stimulated Interleukin-11 Promotes Metastasis of Gastric Cancer Cells Mediated by Upregulation of MUC1. Exp. Cell Res. 2018, 368, 184–193.
- Widjaja, A.A.; Viswanathan, S.; Jinrui, D.; Singh, B.K.; Tan, J.; Wei Ting, J.G.; Lamb, D.; Shekeran, S.G.; George, B.L.; Schafer, S.; et al. Molecular Dissection of Pro-Fibrotic IL11 Signaling in Cardiac and Pulmonary Fibroblasts. Front. Mol. Biosci. 2021, 8, 740650.
- Cook, S.A.; Schafer, S. Hiding in Plain Sight: Interleukin-11 Emerges as a Master Regulator of Fibrosis, Tissue Integrity, and Stromal Inflammation. Annu. Rev. Med. 2020, 71, 263–276.
- Peng, N.; Lu, M.; Kang, M.; Liu, X.; Li, B.; Dong, C. Recombinant Human IL-11 Promotes Lung Adenocarcinoma A549 Cell Growth and EMT through Activating STAT3/HIF-1α/EMT Signaling Pathway. Anticancer Agents Med. Chem. 2021, 21, 1996–2003.
- Zhao, M.; Liu, Y.; Liu, R.; Qi, J.; Hou, Y.; Chang, J.; Ren, L. Upregulation of IL-11, an IL-6 Family Cytokine, Promotes Tumor Progression and Correlates with Poor Prognosis in Non-Small Cell Lung Cancer. Cell. Physiol. Biochem. 2018, 45, 2213–2224.
- Cardó-Vila, M.; Marchiò, S.; Sato, M.; Staquicini, F.I.; Smith, T.L.; Bronk, J.K.; Yin, G.; Zurita, A.J.; Sun, M.; Behrens, C.; et al. Interleukin-11 Receptor Is a Candidate Target for Ligand-Directed Therapy in Lung Cancer: Analysis of Clinical Samples and BMTP-11 Preclinical Activity. Am. J. Pathol. 2016, 186, 2162–2170.
- Lokau, J.; Nitz, R.; Agthe, M.; Monhasery, N.; Aparicio-Siegmund, S.; Schumacher, N.; Wolf, J.; Möller-Hackbarth, K.; Waetzig, G.H.; Grötzinger, J.; et al. Proteolytic Cleavage Governs Interleukin-11 Trans-Signaling. Cell Rep. 2016, 14, 1761–1773.
- Brooks, G.D.; McLeod, L.; Alhayyani, S.; Miller, A.; Russell, P.A.; Ferlin, W.; Rose-John, S.; Ruwanpura, S.; Jenkins, B.J. IL6 Trans-Signaling Promotes KRAS-Driven Lung Carcinogenesis. Cancer Res. 2016, 76, 866–876.
- Ernst, M.; Najdovska, M.; Grail, D.; Lundgren-May, T.; Buchert, M.; Tye, H.; Matthews, V.B.; Armes, J.; Bhathal, P.S.; Hughes, N.R.; et al. STAT3 and STAT1 Mediate IL-11-Dependent and Inflammation-Associated Gastric Tumorigenesis in gp130 Receptor Mutant Mice. J. Clin. Investig. 2008, 118, 1727–1738.
- Ernst, M.; Putoczki, T.L. Molecular Pathways: IL11 as a Tumor-Promoting Cytokine-Translational Implications for Cancers. Clin. Cancer Res. 2014, 20, 5579–5588.
- Heavey, S.; O’Byrne, K.J.; Gately, K. Strategies for Co-Targeting the PI3K/AKT/mTOR Pathway in NSCLC. Cancer Treat. Rev. 2014, 40, 445–456.
- Al-Saad, S.; Donnem, T.; Al-Shibli, K.; Persson, M.; Bremnes, R.M.; Busund, L.-T. Diverse Prognostic Roles of Akt Isoforms, PTEN and PI3K in Tumor Epithelial Cells and Stromal Compartment in Non-Small Cell Lung Cancer. Anticancer Res. 2009, 29, 4175–4183.
- Tang, J.-M.; He, Q.-Y.; Guo, R.-X.; Chang, X.-J. Phosphorylated Akt Overexpression and Loss of PTEN Expression in Non-Small Cell Lung Cancer Confers Poor Prognosis. Lung Cancer 2006, 51, 181–191.
- Tong, M.; Wang, J.; Jiang, N.; Pan, H.; Li, D. Correlation between P-STAT3 Overexpression and Prognosis in Lung Cancer: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0182282.
- Yu, Y.; Zhao, Q.; He, X.-P.; Wang, Z.; Liu, X.-Y.; Zhang, Z.-P. Signal Transducer and Activator of Transcription 3 Overexpression Promotes Lymph Node Micrometastasis in Early-Stage Non-Small Cell Lung Cancer. Thorac. Cancer 2018, 9, 516–522.
- FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and Other Tools) Resource; Food and Drug Administration (US): Silver Spring, MD, USA, 2016.
- Cancer Genome Atlas Research Network; Weinstein, J.N.; Collisson, E.A.; Mills, G.B.; Shaw, K.R.M.; Ozenberger, B.A.; Ellrott, K.; Shmulevich, I.; Sander, C.; Stuart, J.M. The Cancer Genome Atlas Pan-Cancer Analysis Project. Nat. Genet. 2013, 45, 1113–1120.
- GTEx Consortium The Genotype-Tissue Expression (GTEx) Project. Nat. Genet. 2013, 45, 580–585.
- Goldman, M.J.; Craft, B.; Hastie, M.; Repečka, K.; McDade, F.; Kamath, A.; Banerjee, A.; Luo, Y.; Rogers, D.; Brooks, A.N.; et al. Visualizing and Interpreting Cancer Genomics Data via the Xena Platform. Nat. Biotechnol. 2020, 38, 675–678.
- Vivian, J.; Rao, A.A.; Nothaft, F.A.; Ketchum, C.; Armstrong, J.; Novak, A.; Pfeil, J.; Narkizian, J.; Deran, A.D.; Musselman-Brown, A.; et al. Toil Enables Reproducible, Open Source, Big Biomedical Data Analyses. Nat. Biotechnol. 2017, 35, 314–316.
- Pastor, M.D.; Nogal, A.; Molina-Pinelo, S.; Quintanal-Villalonga, Á.; Meléndez, R.; Ferrer, I.; Romero-Romero, B.; De Miguel, M.J.; López-Campos, J.L.; Corral, J.; et al. IL-11 and CCL-1: Novel Protein Diagnostic Biomarkers of Lung Adenocarcinoma in Bronchoalveolar Lavage Fluid (BALF). J. Thorac. Oncol. 2016, 11, 2183–2192.
- Wu, J.; Chen, J.; Lv, X.; Yang, Q.; Yao, S.; Zhang, D.; Chen, J. Clinical Value of Serum and Exhaled Breath Condensate Inflammatory Factor IL-11 Levels in Non-Small Cell Lung Cancer: Clinical Value of IL-11 in Non-Small Cell Lung Cancer. Int. J. Biol. Markers 2021, 36, 64–76.
- Haro, G.J.; Sheu, B.; Cook, N.R.; Woodard, G.A.; Mann, M.J.; Kratz, J.R. Comparison of Conventional TNM and Novel TNMB Staging Systems for Non-Small Cell Lung Cancer. JAMA Netw. Open 2019, 2, e1917062.
- Kratz, J.R.; He, J.; Van Den Eeden, S.K.; Zhu, Z.-H.; Gao, W.; Pham, P.T.; Mulvihill, M.S.; Ziaei, F.; Zhang, H.; Su, B.; et al. A Practical Molecular Assay to Predict Survival in Resected Non-Squamous, Non-Small-Cell Lung Cancer: Development and International Validation Studies. Lancet 2012, 379, 823–832.
- Watza, D.; Lusk, C.M.; Dyson, G.; Purrington, K.S.; Chen, K.; Wenzlaff, A.S.; Ratliff, V.; Neslund-Dudas, C.; Bepler, G.; Schwartz, A.G. Prognostic Modeling of the Immune-Centric Transcriptome Reveals Interleukin Signaling Candidates Contributing to Differential Patient Outcomes. Carcinogenesis 2018, 39, 1447–1454.
- Wang, H.; Wang, M.-S.; Wang, Y.; Huang, Y.-Q.; Shi, J.-P.; Ding, Z.-L.; Wang, W.-J. Prognostic Value of Immune Related Genes in Lung Adenocarcinoma. Oncol. Lett. 2020, 20, 259.
- Fan, T.; Pan, S.; Yang, S.; Hao, B.; Zhang, L.; Li, D.; Geng, Q. Clinical Significance and Immunologic Landscape of a Five-IL(R)-Based Signature in Lung Adenocarcinoma. Front. Immunol. 2021, 12, 693062.
- Chen, C.; Guo, Q.; Tang, Y.; Qu, W.; Zuo, J.; Ke, X.; Song, Y. Screening and Evaluation of the Role of Immune Genes of Brain Metastasis in Lung Adenocarcinoma Progression Based on the TCGA and GEO Databases. J. Thorac. Dis. 2021, 13, 5016–5034.
- Peng, L.; Tao, Y.; Wu, R.; Su, J.; Sun, M.; Cheng, Y.; Xie, Z.; Mao, J.; Zhan, X.; Liu, G. NFAT as a Biomarker and Therapeutic Target in Non-Small Cell Lung Cancer-Related Brain Metastasis. Front. Oncol. 2021, 11, 781150.
