Video capsule endoscopy (VCE) is a minimally invasive endoscopic modality, which was initially introduced for the investigation of the small intestine, but currently a range of capsules are available that can facilitate the inspection of the entire GI tract.
1. Introduction
Video capsule endoscopy (VCE) is a minimally invasive endoscopic modality, which was initially introduced for the investigation of the small intestine, but currently a range of capsules are available that can facilitate the inspection of the entire GI tract
[1]. The role of virtual chromoendoscopy (VC) in capsule endoscopy has been investigated in previous studies, but has not gained wide acceptance in clinical practice, unlike the use of VC in conventional fibreoptic endoscopy
[2]. Several types of VC are integrated in modern endoscopes, enabling the inspection of microvascular and surface patterns, such as narrow band imaging (NBI; Olympus, Tokyo, Japan), Fuji intelligent color enhancement (FICE; Fujinon Inc., Saitama, Japan), and I-Scan (Pentax, Tokyo, Japan). Recently, FICE technology and the blue mode have been included into the RAPID software of VCE
[2].
Flexible spectral imaging color enhancement (FICE) is a form of virtual chromoendoscopy that is incorporated in the capsule reading software and can be used by reviewers to enhance the delineation of lesions in the small bowel
[2]. FICE technology decomposes images by using specific wavelengths (red, green, and blue) and then directly recreates the images with enhanced surface contrast. This leads to enhancement of tissue microvasculature, because of the different optical absorption of light by hemoglobin in the mucosa. On the other hand, blue mode imaging shifts the color within a short wavelength range of 490 to 430 nm, superimposed on the regular white light. Both of these technologies provide real-time enhancement of the surface patterns and color gradients of the GI mucosa, with the intention to better depict small differences between adjacent mucosal areas
[3].The FICE wavelength settings are as follows: FICE 1 (red, 595 nm; green, 540 nm; blue, 535 nm); FICE 2 (red, 420 nm; green, 520 nm; blue 530 nm); and FICE 3 (red, 595 nm; green, 570 nm; blue, 415 nm). FICE 1 reduces the bile interference, FICE 2 emphasizes blood, and FICE 3 emphasizes the differences between bile and blood
[4]. However, despite the presumed theoretical advantages, data on the application of virtual chromoendoscopy in VCE are limited
[5] and the ideal settings for better recognition of the various lesions that can be found in the small bowel and the remaining GI tract are not studied adequately
[3].
2. Angiectasias, Erosions/Ulcers and Tumors
The detection of small bowel lesions using virtual chromoendoscopy settings in VCE is a controversial issue, with studies reporting contrasting results
[1][4][6][1,4,6].
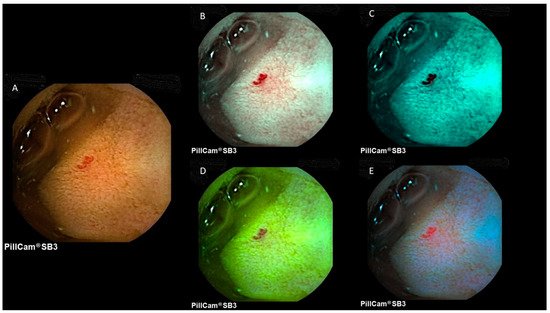
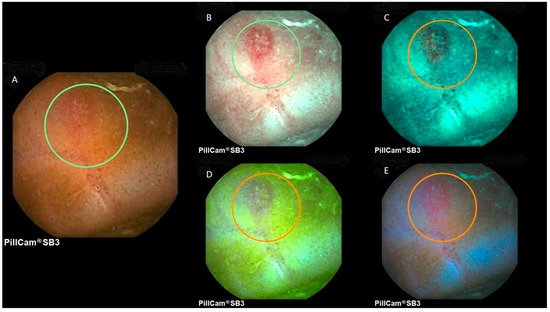
Figure 12 and
Figure 23 provide representative images of a small bowel angiectasia and aphthous ulceration, respectively, using white light, FICE1, FICE2, FICE3 and the blue mode.
Figure 12. Image of a small bowel angiectasia at PillCam SB3. (A) White light; (B) FICE1; (C) FICE2; (D) FICE3; (E) blue mode.
Figure 23. Image of a small bowel aphthous ulcer at PillCam SB3. (A) White light; (B) FICE1; (C) FICE2; (D) FICE3; (E) blue mode.
Regarding the blue filter (BF) mode, only a few retrospective studies were available with conflicting results. In 1 of them, 167 videos from 200 capsule endoscopies were reviewed by 2 experienced endoscopists. For all lesion categories, BF provided image improvement in 83% compared to white light, while with FICE 1, improvement was observed only in 34%, with a worse image observed in 55.9% of cases. FICE1 was effective in improving images of luminal blood. There was no significant image improvement in other lesion subgroups. With FICE 2, improvement was observed in 8.6%, but the image was worse in 77.5% and with FICE 3, improvement was observed in 7.7%, but the image was worse in 79.9%. The study concluded that BF offered better image enhancement in CE as compared with FICE
[7][20]. However, Koulaouzidis et al., in a small cohort of 27 patients with IBD, reported that although the blue mode may enhance mucosal details, such as small mucosal breaks, it did not perform better than WL in the identification of the degree of small bowel inflammation using the Lewis score
[8][21].
On the other hand, there are retrospective studies that have not shown any superiority of chromoendoscopy compared to conventional CE. In these studies, FICE was found to increase only visibility but not necessarily the detection rate of small bowel lesions. Kobayashi et al. studied a cohort of 24 patients who underwent VCE with a variety of small bowel abnormalities (tumors, angiectasias and ulcerative lesions). Three endoscopists reviewed the results in WL and each of the three different FICE modes and measured their sensitivity and specificity for small intestinal lesions. The overall sensitivity of CE was 94.4% with the standard mode, 90.7% with FICE1, 87.0% with FICE2 and 87.0% with FICE 3 and the overall specificity was 66.7%, 55.6%, 77.8% and 66.7%, respectively. No significant differences in the overall sensitivity were found. There was no significant difference between the standard and each FICE mode. In the per lesion analysis, FICE 1 had significantly increased the detection rate of angioectasias and ulcerative lesions compared to the standard mode (angioectasia, 25.7 vs. 21.0,
p = 0.005; ulcerative lesions, 19.3 vs. 14.0,
p = 0.06). However, FICE 1 had decreased the detectability of tumors compared to standard mode (4.3 vs. 10.0,
p = 0.003)
[9][18]. In another study by Gupta et al., in 60 patients who underwent SBCE for OGIB, no significant difference was found in the sensitivity or specificity of FICE for the detection of P2 lesions (lesions with high bleed potential) versus conventional imaging. FICE1 only improved the visibility of non-pathological P0 lesions (
p < 0.01)
[10][22]. Similarly, Matsumura et al. showed that the diagnostic yield for OGIB had not improved by FICE compared to conventional imaging. However, the total number of detected mucosal lesions was significantly higher using FICE (
p < 0.01). The overall diagnostic yield in FICE sets 1, 2, 3 and conventional imaging were 51.9%, 40.7%, 51.9% and 48.1%, respectively, which showed no statistical difference
[11][23]. Finally, a meta-analysis by Yung et al. on the clinical validity of FICE in SBCE concluded that the use of the three FICE modes did not significantly improve the delineation or detection rate of small bowel lesions overall. However, in pigmented lesions (angiectasias, ulcer/erosions), FICE1 performed better in lesion delineation and detection
[6].
3. Colon Capsule Endoscopy
On
e re
cent study by Nakazawa et al. assessed whether chromoendoscopy in colon capsule endoscopy (CCE) can assist in differentiating adenomatous and hyperplastic polyps non-invasively. The second generation CCE (CCE-2) has a high detection rate of approximately 84–94% for polyps ≥ 6 mm and 88–92% for polyps ≥10 mm, offering a pain-free, non-invasive examination. CCE-2 is equipped with flexible spectral imaging color enhancement (FICE) and blue mode (BM). Good differentiation was made possible between adenomatous and hyperplastic polyps by calculating the FICEΔE′ from the CCE images, with a sensitivity of 91.2% and specificity of 88.2%. A total of 52 lesions from 18 patients were assessed. The authors concluded that, if a lesion is <6 mm with FICEΔE′ ≤ 1.76 and the location is the rectum or sigmoid colon, it can be considered hyperplastic, and a watch-and-wait approach can be applied. If a lesion is 6–9 mm and the FICEΔE′ ≤ 1.76, colonoscopy may not be required immediately, as the lesion may be a hyperplastic polyp. However, the patient should undergo CCE or colonoscopy after one year or more
[12][25].