Cardiovascular disease is a major global cause of death, with an estimated 17.9 million cardiovascular disease-related deaths in 2019, representing nearly one third of global deaths. Atherosclerosis, which can begin in childhood, is a multifactorial, chronic condition that contributes to cardiovascular disease. Characterized by lipid deposition in the blood vessel intima, atherosclerosis is associated with inflammation and calcification and can cause vessel stenosis with thrombotic occlusion and/or embolism. A more precise and sophisticated tool that can reliably predict the thrombosis and bleeding risks at an individual level is required in order for clinicians to confidently recommend early interventions with a favorable risk–benefit profile. Critical to the development of this tool is the assessment and understanding of Virchow’s triad and its complex interactions between hypercoagulability, endothelial dysfunction and vessel flow, a fundamental concept to the development of thrombosis.
- cardiovascular disease
- risk assessment
- Virchow's triad
1. Traditional Risk Factors for Cardiovascular Disease
Advancing age confers a major risk for cardiovascular. There are several mechanisms for the dominant effect of age including increased exposure time to age-dependent risk factors that may co-vary in number and severity with aging as well as changes in cardiovascular structure and function with age and how these changes interact with pathophysiological disease mechanisms [4]. In an attempt to limit the changes, the cardiovascular cells generate an inflammatory defense, through the activation of renin–angiotensin–aldosterone endothelin signaling cascades. Advancing age is also associated with the increased prevalence of salt-sensitive hypertension, Over time, the age-associated inflammation in the heart and arteries exceeds a threshold and together with aging-related hemodynamic alterations contributes to fibrosis and arterial stiffness, resulting in cardiovascular diseases [5].
2. Current Available Risk Assessment Tools
3. Virchow's Triad and Its Association with Thrombosis and Cardiovascular Disease
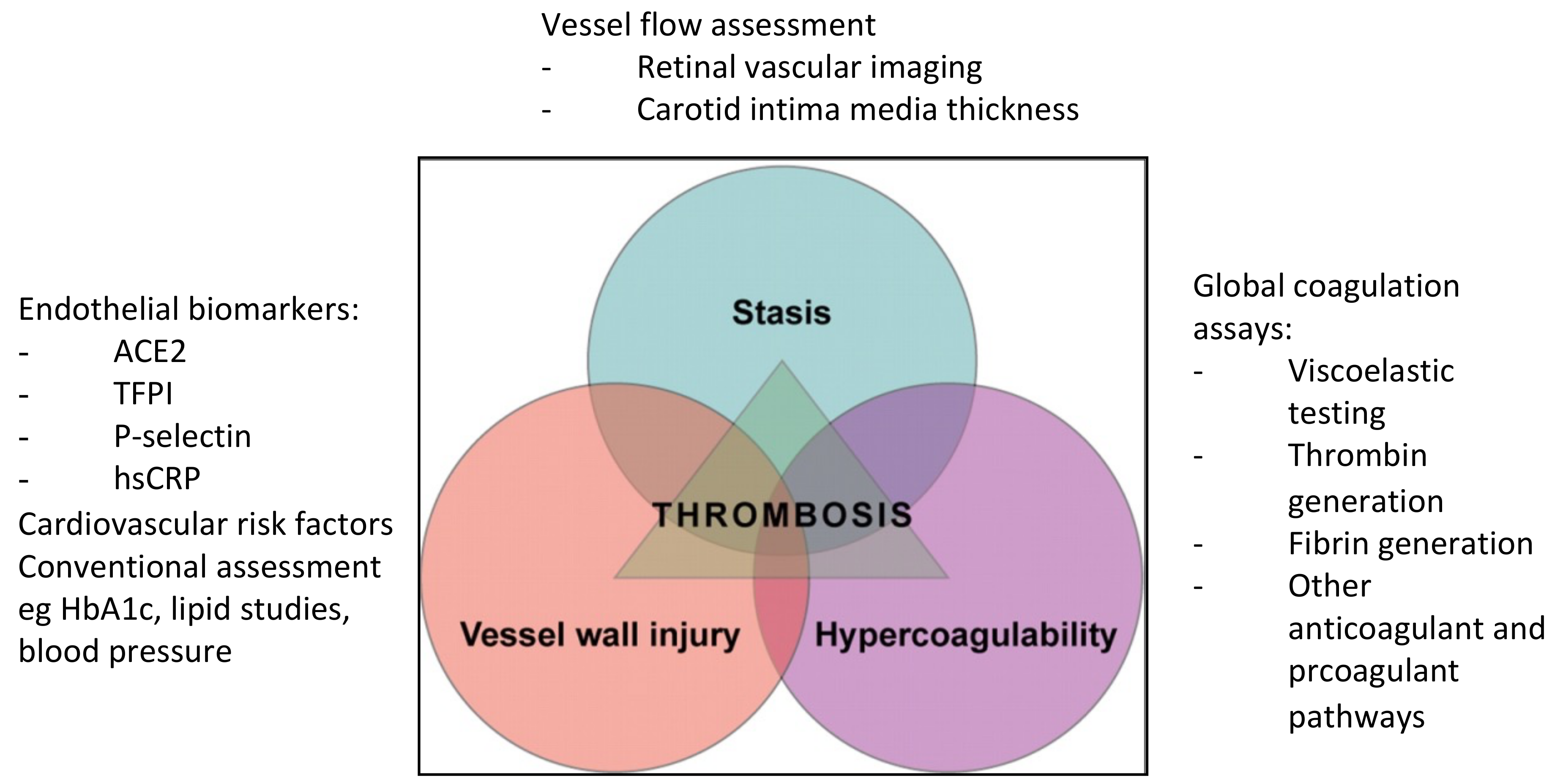
Crucial to the development of thrombosis is the concept of Virchow’s triad. The complex interplay between three elements—the presence of hypercoagulable state, flow stasis and endothelial injury or dysfunction—provides the perfect storm for thrombogenesis. In atherosclerosis, the triad are representative of abnormalities in the endothelium, platelets and coagulation and fibrinolytic pathways, as well as in hemorheology and turbulence at bifurcation and stenotic regions. Plaque rupture exposes prothrombotic proteins including collagen and tissue factor to the coagulation system resulting in thrombus formation, restricted blood flow and onset of cardiovascular disease. The activated platelets also interact with the atherosclerotic endothelium, resulting in the delivery of pro-inflammatory chemokines, further propagating the inflammatory process.
Coagulation also plays an important role in atherogenesis. It is a dynamic but tightly regulated process. While conventional coagulation assays are not useful in predicting thrombosis risks, global coagulation assays provide a more comprehensive assessment of coagulation including the evaluation of the final products of the coagulation cascade, thrombin and fibrin [14]. Although limited in their clinical use in thrombosis medicine in the current state, these assays appear promising, particularly in detecting hypercoagulable states. Some examples of these assays include viscoelastic testing such as thromboelastography and rotational thromboelastometry, thrombin generation assays with calibrated automated thrombogram, and fibrin generation with overall haemostatic potential assays.
The endothelium is highly plastic and diverse and is very amenable in both health and disease. The vascular endothelial cells play critical roles in regulating the crosstalk of the various components required for the maintenance of cardiovascular homeostasis. Endothelial dysfunction is associated with increased vascular permeability and the decreased production of nitric oxide as well as increased reactive oxygen species (ROS) and proinflammatory factors, and it is induced by oxidized LDL [1]. Several chronic metabolic conditions such as the previously listed traditional risk factors of cardiovascular disease can lead to a loss of this equilibrium, shifting towards endothelial dysfunction, a key pathophysiology in atherosclerosis. There are several ways to measure endothelial function which the use of biomarkers including those that are lipid-related, inflammation-based or components of renin-angiotensin system such as angiotensin-converting enzyme 2 (ACE2) [15].
The third contributing factor in Virchow’s triad is flow stasis. Imaging of vessel flow to measure the burden of atherosclerosis may provide better risk assessment than risk assessment calculators. Coronary artery calcium (CAC) scoring can be helpful for determining the extent of coronary artery plaque, while coronary computed tomography angiography (CCTA) provides very high sensitivity for the detection of coronary artery stenosis and nonobstructive plaques [16]. Retinal vascular imaging is a relatively new non-invasive technology for assessing cardiovascular disease risk. The changes in retinal microvasculature have been associated with early-life cardiovascular risk factors including lower birth weight, lesser physical activity, parental hypertension history, childhood obesity and type 1 diabetes [17]. Figure 1 shows some key biomarkers that can be used to assess the components of Virchow’s triad.
4. Genetic Insights into Cardiovascular Risk and Disease
While traditional risk factors account for a large proportion of cardiovascular disease, many persons with atherosclerosis do not have established risk factors, and residual risk exists in patients despite optimal medical therapy, suggesting the presence of unknown risk factors. The majority of cardiovascular risk factors and disease are polygenic, with contributions from both heritable and environmental contributions [18][19]. Genome-wide association studies (GWAS) have led to the discovery of hundreds of loci associated with cardiovascular diseases in the last 15–20 years and have further extended understanding and provided additional insights into the underlying biological pathways, as well as provide a new potential tool for risk calculation, prediction of treatment efficacy or detection of individuals prone to drug side effects [19]. An exploratory analysis by Jaiswal et al. reported that carriers of the age-related clonal hematopoiesis of indeterminate potential (CHIP) are at increased risk for not only hematological malignancies and all-cause mortality but also for coronary heart disease (hazard ratio 2.0; 95% confidence interval (CI) 1.2–3.4) and ischemic stroke (hazard ratio 2.6; 95% CI 1.4–4.8) [20]. CHIP, defined as the presence of an expanded somatic blood-cell clone in persons without other hematologic abnormalities, is more common in older persons, with more than 10% of persons over age 70 years carrying this mutation [21]. Jaiswal et al. also reported that participants with CHIP had 4.0 times greater risk of myocardial infarction than non-carriers (95% CI 2.4–6.7) and increased coronary-artery calcification [21]. Moreover, mice engineered to bear the mutations also demonstrated accelerated atherosclerosis. While the mechanisms behind the causal associations between CHIP and cardiovascular disease are still being investigated, it is now known that the most commonly described CHIP mutations in patients with cardiovascular disease are DNMT3A, TET2, ASXI1, TP53, JAK2 and SF3B [22][23]. Some animal models have demonstrated that CHIP amplifies inflammatory responses, while clinical studies have observed that CHIP carriers have increased levels of inflammatory markers [23], supporting the association between aging, CHIP and inflammation.5. Conclusions
A more specific and sensitive risk assessment model is required to allow clinicians to confidently recommend early interventions in thrombosis and cardiovascular disease management with favorable risk–benefit profiles. Critical to the development of this model is the assessment and understanding of Virchow’s triad and its complex interactions between hypercoagulability, endothelial dysfunction and vessel flow. To achieve this, individualized risk assessment can be improved through an integrated, multimodal approach using a combination of tools such as global coagulation assays, endothelial biomarkers and vessel flow assessment in tandem with clinical surrogate markers. The addition of new tools such as GWAS may further refine the risk stratification
