Primary microglial leukodystrophy or leukoencephalopathy are disorders in which a genetic defect linked to microglia causes cerebral white matter damage. Pigmented orthochromatic leukodystrophy, adult-onset orthochromatic leukodystrophy associated with pigmented macrophages, hereditary diffuse leukoencephalopathy with (axonal) spheroids, and adult-onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP) are different terms apparently used to designate the same disease. However, ALSP linked to dominantly inherited mutations in CSF1R (colony-stimulating factor receptor 1) causes CSF-1R-related leukoencephalopathy (CRP). Yet, recessive ALSP with ovarian failure linked to AARS2 (alanyl-transfer (t)RNA synthase 2) mutations (LKENP) is a mitochondrial disease and not a primary microglial leukoencephalopathy. Polycystic membranous lipomembranous osteodysplasia with sclerosing leukoencephalopathy (PLOSL; Nasu–Hakola disease: NHD) is a systemic disease affecting bones, cerebral white matter, selected grey nuclei, and adipose tissue The disease is caused by mutations of one of the two genes TYROBP or TREM2, identified as PLOSL1 and PLOSL2, respectively.
- pigmented orthochromatic leukodystrophy
- adult-onset orthochromatic leukodystrophy associated with pigmented macrophages
- hereditary diffuse leukoencephalopathy with axonal spheroids
- adult-onset (or dominant) leukodystrophy with axonal spheroids and pigment
1. Introduction
2. Adult-Onset Leukodystrophy with Axonal Spheroids and Pigmented Glia (POLD, HDLS, ALSP): CRP Linked to Mutations in CSF1R, and LKENP (Leukoencephalopathy, Progressive with Ovarian Failure) Linked to Heterozygous Mutations in AARS2
2.1. Clinical Features
2.1.1. ALSP-CSFR1 or CRL
A large study comprising 90 families with the CSFR1 mutation revealed the mean age at onset to be 43 years (range 18–78 years), mean age at death 53 years (range 23–84 years), with a mean disease of duration 6.8 years (range 1–29 years); clinical symptoms in women appear at a younger age [36][7]. Behavioral and personality changes, memory impairment, executive dysfunction, and dementia are common symptoms. These are often accompanied by motor dysfunction including pyramidal signs (spasticity, hyperreflexia, hemiparesis, quadriparesis), sensory deficits, depression, and parkinsonian symptoms and signs such as gait impairment, rigidity, bradykinesia, postural instability, and tremor [26,27,36,37,38,39,40,41,42,43,44][7][8][9][10][11][12][13][14][15][16][17]. Speech difficulty, non-fluent aphasia, and symptoms mimicking frontotemporal dementia behavioral variant (FTD-bv) have been described [31,45,46,47][18][19][20][21]. Less common manifestations are corticobasal syndrome and stroke [40][13]. Cerebellar and bulbar/pseudobulbar signs may occur at advanced stages, whereas seizures may appear at the onset of the disease. Peripheral neuropathy has been noted in some patients [46,48][20][22]. Yet, whether peripheral neuropathy belongs to the CSF1R-related spectrum is an open question requiring further investigation [46][20]. Involvement of the optic nerve is very rare [49][23]. Considering the variability of clinical symptoms, misdiagnoses such as frontotemporal dementia, parkinsonism, multiple sclerosis, normal-pressure hydrocephalus, and vasculitis of the central nervous system, among others, are commonplace [50,51,52][24][25][26]. Differential diagnosis covers several entities, mainly adult-onset leukodystrophies [2,31][2][18].2.1.2. ALSP-AARS2 or LKENP
Dallabona et al. [33][27] described another group of patients with progressive leukoencephalopathy starting in childhood or in early adulthood, characterized by progressive gait ataxia, tremor, spasticity, dystonia, dysarthria, and cognitive decline. The affected women presented with ovarian failure and amenorrhea, followed by neurodegeneration, or presented ovarian failure during the progression of the neurological disorder. The investigation of mitochondrial function in two patients identified cytochrome c oxidase deficiency. Ragged-red fibers were absent. None of the patients had signs of cardiomyopathy. Brain MRI showed leukoencephalopathy with the involvement of left-right connections, descending tracts, and cerebellar atrophy. Next-generation sequencing revealed compound heterozygous mutations in AARS2, which encodes mitochondrial alanyl-tRNA synthetase, in both patients. Functional studies in yeast confirmed the pathogenicity of the mutations in one patient [33][27]. Additional cases of leukoencephalopathy linked to AARS2 mutations have been reported [53][28].2.2. Radiological Findings
Atrophy and increased signal in the white matter, thinning of the corpus callosum, abnormal signaling of the pyramidal tracts, and enlarged ventricles are seen on MRI. The subcortical and periventricular white matter shows T2-weighted and FLAIR hyper-intensities with no gadolinium-enhanced lesions; these hyperintensities are usually diffuse but they can be confluent, with asymmetric distribution. Calcifications in the white matter are found in about one half of cases; calcifications in the frontal periventricular white matter are common in cases linked to CSFR1 mutations (CRL), but they are absent in cases linked to AARS2 mutations (LKENP) [24,26,33,36,38,39,41,44,54,55,56,57,58,59,60][7][8][11][12][14][17][27][29][30][31][32][33][34][35][36]. In CT images, calcifications mainly involve the frontal white matter adjacent to the anterior horns of the lateral ventricles and the parietal subcortical white matter; calcifications have a symmetrical, “stepping stone” appearance in the pericallosal regions [61][37]. Thin-slice CT techniques are necessary to detect small calcifications [41][14]. The cerebellum and the brain stem appear normal. MR spectroscopy shows changes in metabolite concentrations not only in patients with HDLS linked to CSFR1 mutation and also in asymptomatic CSF1R mutation carriers [62][38].2.3. Neuropathology
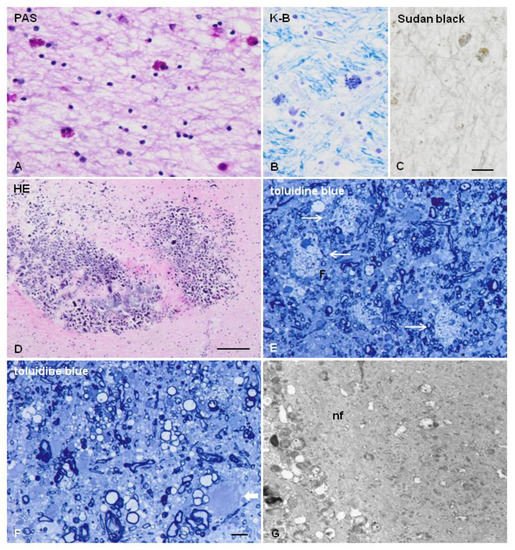
The characteristic lesions are: (a) bilateral and confluent demyelination of the cerebral white matter sparing the cortico-subcortical U fibers, and involvement of the corpus callosum and internal capsule; (b) axonal damage with spheroids in the white matter; (c) infiltration of macrophages filled with neutral lipids; and (d) cytoplasmic deposits in macrophages, astrocytes, and oligodendrocytes stained with periodic acid–Schiff, Sudan black, and Klüver–Barrera that are autofluorescent in paraffin sections [11,12,38,39,40,41,45][11][12][13][14][19][39][40]. Axonal damage is best seen with silver-based methods and immunohistochemistry with antibodies against neurofilaments, β-amyloid precursor protein, and ubiquitin. Electron microscopy reveals that spheroids are mainly composed of neurofilaments; less frequently, they also contain microtubules, mitochondria, and altered mitochondria, together with granular material [20,63][41][42]. Pigments contain electron-dense granular material with lamellar or fingerprint arrangement reminiscent of ceroid-lipofuscin [11,12,20,25][39][40][41][43] (Figure 1 and Figure 2). Characteristic lesions are also seen in cerebral biopsy samples.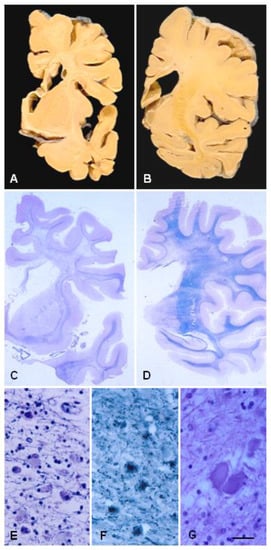
3. Polycystic Membranous Lipomembranous Osteodysplasia with Sclerosing Leukoencephalopathy (PLOSL; Nasu–Hakola Disease)
3.1. Clinical Features
The disease usually manifests in the third decade by multiple cyst-like lesions and loss of bone trabeculae, causing pain and tenderness, mainly in feet and ankles; fractures following minor accidents are common. The osseous stage is followed by a progressive neurological disease consisting of abnormal personality and behavior, episodes of depression and euphoria, loss of social inhibition, memory deficits, and apathy, together with spasticity, postural dyspraxia, and involuntary movements. Urinary incontinence, loss of libido, and sexual impotence are early symptoms in some cases. Seizures may be present. Patients die in a vegetative state before the age of 50 years [111,112,115,116,117,118,119,120,121,122,123,124,125][49][50][51][52][53][54][55][56][57][58][59][60][61]. Due to the first appearance of osseous lesions in most cases, neuropsychological tests and functional neuroimaging can be useful in identifying subclinical bone alterations in the early stages of NHD [126,127][62][63]. Progressive spastic paraplegia and dementia without skeletal symptoms, but accompanied by polycystic osteodysplasia following X-ray examination, are clinical manifestations in some subjects [126][62]. In some cases, skeletal symptoms are not apparent, and patients complain of behavioral and neurological deficits. NHD cases without apparent skeletal symptoms occur in patients with mutations in TREM2, but not TYROBP [128,129,130,131,132][64][65][66][67][68]. Osseous pathology is not always present or diagnosed [121,125,133][57][61][69]. Radiological examination of bones is recommended in patients with neurological deficits clinically suggestive of NHD.3.2. Radiological Examination
In NHD, cyst-like lesions are typically found in the carpal and tarsal bones and in the fingers [115,121,134][51][57][70]. Brain CT scans show cerebral atrophy with enlargement of the frontal regions of the lateral ventricles and calcifications in the globus pallidus. MRI reveals diffuse high density in the cerebral white matter and reduced density in the basal nuclei on T2-weighed images; white matter lesions extend from the periventricular areas to the periphery, sparing the cortico-cortical arcuate fibers [113,120,121,135,136,137,138,139][56][57][71][72][73][74][75][76]. Hypoperfusion of the grey matter has been noted in SPECT and PET studies [140,141][77][78].3.3. General Pathology
Bone lesions are membrane-cystic lesions that destroy the osseous tissue. Membranes are convoluted, eosinophilic, PAS-positive, and autofluorescent; they contain carbohydrates, phospholipids, fatty acid crystals, hydroxyapatite crystals, and collagen. Under electron microscopy, the membranes mainly form tubular and saccular structures and contain granular material. Cysts are filled with triglycerides. In addition, the neighboring blood vessels show reduced lumen, enlargement of the inner elastic membrane, and degeneration of the muscular layer [114,120,142,143,144,145][56][79][80][81][82][83]. Examination of a transiliac bone biopsy sample from one patient revealed disordered lamellar collagen fibril arrangement and increased matrix mineralization, pointing toward the involvement of osteoclast defects in this condition [146][84]. In addition to the bones, membranous lipodystrophy appears as a form of degeneration of the adipose tissue [144][82]. Several tissues are also affected, such as the cutaneous and perivisceral adipose tissue, bone marrow, alveolar septa of the lungs, and rectal mucosa [120,126,147][56][62][85].3.4. Neuropathology
The central nervous system in NHD is decreased in size and has a reduced consistency of the cerebral white matter, atrophy of the frontal and temporal lobes, and dilated ventricles. The globus pallidus presents with brownish discoloration on macroscopic examination. Histological sections processed for myelin staining exhibit generalized symmetrical demyelination of the cerebral white matter with preservation of the arcuate subcortical fibers, corpus callosum, and white matter of the cerebellum. There is marked astrogliosis, but with the discrete presence of macrophages filled with sudanophilic material, and the absence of inflammatory infiltration. Axonal degeneration accompanied by axonal spheroids is common. Axonal spheroids contain neurofilaments, mitochondria, vesicles, and granular material [125,126,148,149][61][62][86][87]. The blood vessels in the white matter have increased thickness and multi-layering of the basement membrane [120,150][56][88]. The grey matter has less notable pathology [149][87]. The globus pallidus shows variable neuron loss and astrocytic gliosis, and numerous calcospherites containing calcium, iron, and glycoprotein matrix [126,139,148,149,151][62][76][86][87][89]. The thalamus and hippocampus show a discrete neuronal loss in most cases. Marked neuronal loss and astrocytic gliosis in the caudate nucleus, putamen, substantia nigra, and thalamus (particularly in the dorsomedial and anterior nucleus) are found in some patients [149][87]. Severe thalamic degeneration occurs only rarely [152][90]. Alzheimer’s disease pathology (neurofibrillary tangles and senile plaques) is as common in NHD as in the control population [153][91]. However, a recent report described a 51-year-old female with NHD, bearing a homozygous mutation (Q33X) of the TREM2 gene, and showing spots of neurofibrillary tangle pathology in the neocortex, but sparing the mesial temporal structures on post-mortem examination [154][92]. The percentage of short carbon chain non-hydroxyl fatty acids of sulfatide and the percentage of palmitic acid of ganglioside in the cortex in NHD were both increased in comparison to controls [155][93]. Peripheral neuropathy with axonal and segmental degeneration has been reported in a few cases [126,156][62][94].References
- Van Der Knaap, M.S.; Bugiani, M. Leukodystrophies: A proposed classification system based on pathological changes and pathogenetic mechanisms. Acta Neuropathol. 2017, 134, 351–382.
- Köhler, W.; Curiel, J.; Vanderver, A. Adulthood leukodystrophies. Nat. Rev. Neurol. 2018, 14, 94–105.
- Lynch, D.S.; De Paiva, A.R.B.; Zhang, W.; Bugiardini, E.; Freua, F.; Lucato, L.; de Souza, L.I.M.; Lakshmanan, R.; Kinsella, J.A.; Merwick, A.; et al. Clinical and genetic characterization of leukoencephalopathies in adults. Brain 2017, 140, 1204–1211.
- Van der Knaap, M.S.; Schiffmann, R.; Mochel, F.; Wolf, N. Diagnosis, prognosis, and treatment of leukodystrophies. Lancet Neurol. 2019, 18, 962–972.
- Resende, L.L.; De Paiva, A.R.B.; Kok, F.; Leite, C.D.C.; Lucato, L. Adult Leukodystrophies: A Step-by-Step Diagnostic Approach. RadioGraphics 2019, 39, 153–168.
- Garcia, L.M.; Hacker, J.L.; Sase, S.; Adang, L.; Almad, A. Glial cells in the driver seat of leukodystrophy pathogenesis. Neurobiol. Dis. 2020, 146, 105087.
- Konno, T.; Yoshida, K.; Mizuno, T.; Kawarai, T.; Tada, M.; Nozaki, H.; Ikeda, S.-I.; Nishizawa, M.; Onodera, O.; Wszolek, Z.K.; et al. Clinical and genetic characterization of adult-onset leukoencephalopathy with axonal spheroids and pigmented glia associated with CSF1R mutation. Eur. J. Neurol. 2016, 24, 37–45.
- Freeman, S.H.; Hyman, B.T.; Sims, K.B.; Hedley-Whyte, E.T.; Vossough, A.; Frosch, M.P.; Schmahmann, J.D. Adult Onset Leukodystrophy with Neuroaxonal Spheroids: Clinical, Neuroimaging and Neuropathologic Observations. Brain Pathol. 2008, 19, 39–47.
- Lynch, D.S.; Jaunmuktane, Z.; Sheerin, U.-M.; Phadke, R.; Brandner, S.; Milonas, I.; Dean, A.; Bajaj, N.; McNicholas, N.; Costello, D.; et al. Hereditary leukoencephalopathy with axonal spheroids: A spectrum of phenotypes from CNS vasculitis to parkinsonism in an adult onset leukodystrophy series. J. Neurol. Neurosurg. Psychiatry 2015, 87, 512–519.
- Sundal, C.; Fujioka, S.; Van Gerpen, J.A.; Wider, C.; Nicholson, A.M.; Baker, M.; Shuster, E.A.; Aasly, J.; Spina, S.; Ghetti, B.; et al. Parkinsonian features in hereditary diffuse leukoencephalopathy with spheroids (HDLS) and CSF1R mutations. Park. Relat. Disord. 2013, 19, 869–877.
- Kleinfeld, K.; Mobley, B.; Hedera, P.; Wegner, A.; Sriram, S.; Pawate, S. Adult-onset leukoencephalopathy with neuroaxonal spheroids and pigmented glia: Report of five cases and a new mutation. J. Neurol. 2012, 260, 558–571.
- Kimura, T.; Ishizawa, K.; Mitsufuji, T.; Abe, T.; Nakazato, Y.; Yoshida, K.; Sasaki, A.; Araki, N. A clinicopathological and genetic study of sporadic diffuse leukoencephalopathy with spheroids: A report of two cases. Neuropathol. Appl. Neurobiol. 2013, 39, 837–843.
- Guerreiro, R.; Kara, E.; Le Ber, I.; Bras, J.; Rohrer, J.D.; Taipa, R.; Lashley, T.; Dupuits, C.; Gurunlian, N.; Mochel, F.; et al. Genetic Analysis of Inherited Leukodystrophies. JAMA Neurol. 2013, 70, 875–882.
- Konno, T.; Tada, M.; Koyama, A.; Nozaki, H.; Harigaya, Y.; Nishimiya, J.; Matsunaga, A.; Yoshikura, N.; Ishihara, K.; Arakawa, M.; et al. Haploinsufficiency of CSF-1R and clinicopathologic characterization in patients with HDLS. Neurology 2013, 82, 139–148.
- Kawakami, I.; Iseki, E.; Kasanuki, K.; Minegishi, M.; Sato, K.; Hino, H.; Shibuya, K.; Fujisawa, K.; Higashi, S.; Akiyama, H.; et al. A family with hereditary diffuse leukoencephalopathy with spheroids caused by a novel c.2442+2T>C mutation in the CSF1R gene. J. Neurol. Sci. 2016, 367, 349–355.
- Ikeuchi, T.; Mezaki, N.; Miura, T. Cognitive dysfunction and symptoms of movement disorders in adult-onset leukoencephalopathy with axonal spheroids and pigmented glia. Park. Relat. Disord. 2018, 46, S39–S41.
- Leng, C.; Lu, L.; Wang, G.; Zhang, Y.; Xu, Y.; Lin, X.; Shen, N.; Xu, X.; Qun, S.; Sun, M.; et al. A novel dominant-negative mutation of the CSF1R gene causes adult-onset leukoencephalopathy with axonal spheroids and pigmented glia. Am. J. Transl. Res. 2019, 11, 6093–6101.
- Sundal, C.; Wszolek, Z.K. CSFR1-related adult-onset leukoencephalopathy with axonal spheroids and pigmented glia. In GeneReviews® ; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2017.
- Calatayud, T.; Turkalp, Z.T.; Gonzales, A.A.; Muñoz, D.G. Adult-onset leukoencephalopathy with axonal spheroids and pigmented glia: Report on a case with morphometric studies. Clin. Neuropathol. 2013, 32, 492–501.
- Tian, W.-T.; Zhan, F.-X.; Liu, Q.; Luan, X.-H.; Zhang, C.; Shang, L.; Zhang, B.-Y.; Pan, S.-J.; Miao, F.; Hu, J.; et al. Clinicopathologic characterization and abnormal autophagy of CSF1R-related leukoencephalopathy. Transl. Neurodegener. 2019, 8, 32.
- Funayama, M.; Sugihara, M.; Takata, T.; Mimura, M.; Ikeuchi, T. Remarkable behavioural signs and progressive non-fluent aphasia in a patient with adult-onset leucoencephalopathy with axonal spheroids and pigmented glia. Psychogeriatrics 2018, 19, 282–285.
- Di Donato, I.; Stabile, C.; Bianchi, S.; Taglia, I.; Mignarri, A.; Salvatore, S.; Giorgio, E.; Brusco, A.; Simone, I.; Dotti, M.T.; et al. A Novel CSF1R Mutation in a Patient with Clinical and Neuroradiological Features of Hereditary Diffuse Leukoencephalopathy with Axonal Spheroids. J. Alzheimer’s Dis. 2015, 47, 319–322.
- Shu, Y.; Long, L.; Liao, S.; Yang, J.; Li, J.; Qiu, W.; Yang, Y.; Bao, J.; Wu, A.; Hu, X.; et al. Involvement of the optic nerve in mutated CSF1R-induced hereditary diffuse leukoencephalopathy with axonal spheroids. BMC Neurol. 2016, 16, 171.
- Lynch, D.S.; Zhang, W.; Lakshmanan, R.; Kinsella, J.A.; Uzun, G.A.; Karbay, M.; Tufekcioglu, Z.; Hanagasi, H.; Burke, G.; Foulds, N.; et al. Analysis of Mutations in AARS2 in a Series of CSF1R-Negative Patients with Adult-Onset Leukoencephalopathy with Axonal Spheroids and Pigmented Glia. JAMA Neurol. 2016, 73, 1433–1439.
- Wang, M.; Zhang, X. A novel CSF-1R mutation in a family with hereditary diffuse leukoencephalopathy with axonal spheroids misdiagnosed as hydrocephalus. Neurogenetics 2019, 20, 155–160.
- Mao, C.; Zhou, L.; Zhou, L.; Yang, Y.; Niu, J.; Li, J.; Huang, X.; Ren, H.; Zhao, Y.; Peng, B.; et al. Biopsy histopathology in the diagnosis of adult-onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP). Neurol. Sci. 2019, 41, 403–409.
- Dallabona, C.; Diodato, D.; Kevelam, S.H.; Haack, T.B.; Wong, L.-J.; Salomons, G.S.; Baruffini, E.; Melchionda, L.; Mariotti, C.; Strom, T.M.; et al. Novel (ovario) leukodystrophy related to AARS2 mutations. Neurology 2014, 82, 2063–2071.
- Dong, Q.; Long, L.; Chang, Y.-Y.; Lin, Y.-J.; Liu, M.; Lu, Z.-Q. An adolescence-onset male leukoencephalopathy with remarkable cerebellar atrophy and novel compound heterozygous AARS2 gene mutations: A case report. J. Hum. Genet. 2018, 63, 841–846.
- Itoh, K.; Shiga, K.; Shimizu, K.; Muranishi, M.; Nakagawa, M.; Fushiki, S. Autosomal dominant leukodystrophy with axonal spheroids and pigmented glia: Clinical and neuropathological characteristics. Acta Neuropathol. 2005, 111, 39–45.
- Van Gerpen, J.A.; Wider, C.; Broderick, D.F.; Dickson, D.W.; Brown, L.A.; Wszolek, Z.K. Insights into the dynamics of hereditary diffuse leukoencephalopathy with axonal spheroids. Neurology 2008, 71, 925–929.
- Sundal, C.; Van Gerpen, J.A.; Nicholson, A.M.; Wider, C.; Shuster, E.A.; Aasly, J.; Spina, S.; Ghetti, B.; Roeber, S.; Garbern, J.; et al. MRI characteristics and scoring in HDLS due to CSF1R gene mutations. Neurology 2012, 79, 566–574.
- Fujioka, S.; Broderick, D.F.; Sundal, C.; Baker, M.C.; Rademakers, R.; Wszolek, Z.K. An adult-onset leukoencephalopathy with axonal spheroids and pigmented glia accompanied by brain calcifications: A case report and a literature review of brain calcifications disorders. J. Neurol. 2013, 260, 2665–2668.
- Bender, B.; Klose, U.; Lindig, T.; Biskup, S.; Nägele, T.; Schöls, L.; Karle, K.N. Imaging features in conventional MRI, spectroscopy and diffusion weighted images of hereditary diffuse leukoencephalopathy with axonal spheroids (HDLS). J. Neurol. 2014, 261, 2351–2359.
- Robinson, J.L.; Suh, E.; Wood, E.M.; Lee, E.B.; Coslett, H.B.; Raible, K.; Lee, V.M.-Y.; Trojanowski, J.Q.; Van Deerlin, V.M. Common neuropathological features underlie distinct clinical presentations in three siblings with hereditary diffuse leukoencephalopathy with spheroids caused by CSF1R p.Arg782His. Acta Neuropathol. Commun. 2015, 3, 42.
- Ayrignac, X.; Nicolas, G.; Carra-Dallière, C.; Hannequin, D.; Labauge, P. Brain Calcifications in Adult-Onset Genetic Leukoencephalopathies. JAMA Neurol. 2017, 74, 1000.
- Codjia, P.; Ayrignac, X.; Mochel, F.; Mouzat, K.; Carra-Dalliere, C.; Castelnovo, G.; Ellie, E.; Etcharry-Bouyx, F.; Verny, C.; Belliard, S.; et al. Adult-Onset Leukoencephalopathy with Axonal Spheroids and Pigmented Glia: An MRI Study of 16 French Cases. Am. J. Neuroradiol. 2018, 39, 1657–1661.
- Konno, T.; Broderick, D.F.; Mezaki, N.; Isami, A.; Kaneda, D.; Tashiro, Y.; Tokutake, T.; Keegan, B.M.; Woodruff, B.K.; Miura, T.; et al. Diagnostic Value of Brain Calcifications in Adult-Onset Leukoencephalopathy with Axonal Spheroids and Pigmented Glia. Am. J. Neuroradiol. 2016, 38, 77–83.
- Abe, T.; Kawarai, T.; Fujita, K.; Sako, W.; Terasawa, Y.; Matsuda, T.; Sakai, W.; Tsukamoto-Miyashiro, A.; Matsui, N.; Izumi, Y.; et al. MR Spectroscopy in Patients with Hereditary Diffuse Leukoencephalopathy with Spheroids and Asymptomatic Carriers of Colony-stimulating Factor 1 Receptor Mutation. Magn. Reson. Med Sci. 2017, 16, 297–303.
- Gray, F.; Destée, A.; Bourre, J.-M.; Gherardi, R.; Krivosic, I.; Warot, P.; Poirier, J. Pigmentary Type of Orthochromatic Leukodystrophy: A new case with ultrastructural and biochemical study. J. Neuropathol. Exp. Neurol. 1987, 46, 585–596.
- Tuñón, T.; Ferrer, I.; Gállego, J.; Delgado, G.; Villanueva, J.A.; Martinez-Peñuela, J.M. Leucodystrophy with pigmented glial and scavenger cells (pigmentary type of orthochromatic leucodystrophy). Neuropathol. Appl. Neurobiol. 1988, 14, 337–344.
- Hoffmann, S.; Murrell, J.; Harms, L.; Miller, K.; Meisel, A.; Brosch, T.; Scheel, M.; Ghetti, B.; Goebel, H.-H.; Stenzel, W. Enlarging the Nosological Spectrum of Hereditary Diffuse Leukoencephalopathy with Axonal Spheroids (HDLS). Brain Pathol. 2014, 24, 452–458.
- Mendes, A.; Pinto, M.; Vieira, S.; Castro, L.; Carpenter, S. Adult-onset leukodystrophy with axonal spheroids. J. Neurol. Sci. 2010, 297, 40–45.
- Ali, Z.S.; Van Der Voorn, J.P.; Powers, J.M. A Comparative Morphologic Analysis of Adult Onset Leukodystrophy with Neuroaxonal Spheroids and Pigmented Glia-A Role for Oxidative Damage. J. Neuropathol. Exp. Neurol. 2007, 66, 660–672.
- Martinez-Saez, E.; Shah, S.; Costa, C.; Fleminger, S.; Connor, S.; Bodi, I. Adult onset leukodystrophy with neuroaxonal spheroids and demyelinating plaque-like lesions. Neuropathology 2011, 32, 285–292.
- Alturkustani, M.; Sharma, M.; Hammond, R.; Ang, L.-C. Adult-Onset Leukodystrophy: Review of 3 Clinicopathologic Phenotypes and a Proposed Classification. J. Neuropathol. Exp. Neurol. 2013, 72, 1090–1103.
- Oyanagi, K.; Kinoshita, M.; Inoue, T.; Nakahara, A.; Tokiwai, M.; Arai, N.; Aoki, N.; Jinnai, K.; Yazawa, I.; Ishihara, K.; et al. Adult onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP) and Nasu-Hakola disease: Lesion staging and dynamic changes of axons and microglial subsets. Brain Pathol. 2017, 27, 748–769.
- Alturkustani, M.; Keith, J.; Hazrati, L.-N.; Rademakers, R.; Ang, L.-C. Pathologic Staging of White Matter Lesions in Adult-Onset Leukoencephalopathy/Leukodystrophy With Axonal Spheroids. J. Neuropathol. Exp. Neurol. 2015, 74, 233–240.
- Lin, W.L.; Wszolek, Z.K.; Dickson, D.W. Hereditary diffuse leukoencephalopathy with spheroids: Ultrastructural and immunoe-lectron microscopic studies. Int. J. Clin. Exp. Pathol. 2010, 3, 665–674.
- Terayama, K. Two cases of cystic bone disease showing peculiar features. Nippon Seikeigeka Gakkai Zasshi 1961, 35, 626.
- Hakola, H.P.A.; Järvi, O.H.; Sourander, P. Osteodysplasia polycystica hereditaria combined with sclerosing leucoencephalopathy. Acta Neurol. Scand. 2009, 46, 79–80.
- Nasu, T.; Tsukahara, Y.; Terayama, K. A lipid metabolic disease—“Membranous lipodystrophy”—An autopsy case demonstrating numerous peculiar membrane-structures composed of compound lipid in bone and bone marrow and various adipose tissues. Acta Pathol. Jpn. 1973, 23, 539–558.
- Harada, K. A case of “membranous lipodystrophy (Nasu)” with emphasis on psychiatric and neuropathologic aspects. Folia Psychiatr. Neurol. Jpn. 1975, 29, 169–177.
- Hakola, P.; Virtama, P. Radiologic bone changes of polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy. Skelet. Radiol. 1982, 8, 51–54.
- Minagawa, M.; Maeshiro, H.; Shioda, K.; Hirano, A. Membranous lipodystrophy (Nasu disease): Clinical and neuropathological study of a case. Clin. Neuropathol. 1985, 4, 38–45.
- Hakola, H.P. Polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy (membranous lipodystrophy): A neuropsychiatric follow-up study. In Monographs of Psychiatria Fennica; Henriksson, M., Huttunen, M., Kuoppasalmi, K., Lindfors, O., Lonnqvist, J., Eds.; Foundation for Psychiatric Research: Helsinki, Finland, 1990; pp. 1–114.
- Ishigooka, M.; Hashimoto, T.; Izumiya, K.; Kodama, C.; Nakada, T. Membranous Lipodystrophy (Nasu’s Disease): A Rare Cause of Neuropathic Urinary Incontinence. Urol. Int. 1993, 50, 179–181.
- Verloes, A.; Maquet, P.; Sadzot, B.; Vivario, M.; Thiry, A.; Franck, G. Nasu-Hakola syndrome: Polycystic lipomembranous osteodysplasia with sclerosing leucoencephalopathy and presenile dementia. J. Med. Genet. 1997, 34, 753–757.
- Bm, J.P.; Autti, T.; Raininko, R.; Partanen, J.; Salonen, O.; Puranen, M.; Hakola, P.; Haltia, M. CNS manifestations of Nasu-Hakola disease: A frontal dementia with bone cysts. Neurology 2001, 56, 1552–1558.
- Bianchin, M.M.; Capella, H.M.; Chaves, D.L.; Steindel, M.; Grisard, E.C.; Ganev, G.G.; da Silva Júnior, J.P.; Neto Evaldo, S.; Poffo, M.A.; Walz, R.; et al. Nasu-Hakola disease (polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy—PLOSL): A dementia associated with bone cystic lesions. From clinical to genetic and molecular aspects. Cell Mol. Neurobiol. 2004, 24, 1–24.
- Kaneko, M.; Sano, K.; Nakayama, J.; Amano, N. Nasu-Hakola disease: The first case reported by Nasu and review: The 50th An-niversary of Japanese Society of Neuropathology. Neuropathology 2010, 30, 463–470.
- Ilonen, T.; Hakola, P.; Vanhanen, M.; Tiihonen, J. Rorschach assessment of personality functioning in patients with polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy. Acta Neuropsychiatr. 2012, 24, 236–244.
- Paloneva, J.; Autti, T.; Hakola, P.; Haltia, M.J. Polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy (PLOSL). In GeneReviews® ; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Stephens, K., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2020.
- Kitajima, I.; Kuriyama, M.; Usuki, F.; Izumo, S.; Osame, M.; Suganuma, T.; Murata, F.; Nagamatsu, K. Nasu-Hakola disease (membranous lipodystrophy): Clinical, histopathological and biochemical studies of three cases. J. Neurol. Sci. 1989, 91, 35–52.
- Montalbetti, L.; Ratti, M.T.; Greco, B.; Aprile, C.; Moglia, A.; Soragna, D. Neuropsychological tests and functional nuclear neuroim-aging provide evidence of subclinical impairment in Nasu-Hakola disease heterozygotes. Funct. Neurol. 2005, 20, 71–75.
- Chouery, E.; Delague, V.; Bergougnoux, A.; Koussa, S.; Serre, J.-L.; Mégarbané, A. Mutations in TREM2 lead to pure early-onset dementia without bone cysts. Hum. Mutat. 2008, 29, E194–E204.
- Guerreiro, R.; Bilgic, B.; Guven, G.; Bras, J.; Rohrer, J.; Lohmann, E.; Hanagasi, H.; Gürvit, H.; Emre, M. A novel compound heterozygous mutation in TREM2 found in a Turkish frontotemporal dementia-like family. Neurobiol. Aging 2013, 34, 2890.e1–2890.e5.
- Guerreiro, R.J.; Lohmann, E.; Bras, J.; Gibbs, J.R.; Rohrer, J.; Gurunlian, N.; Dursun, B.; Bilgic, B.; Hanagasi, H.; Gürvit, H.; et al. Using Exome Sequencing to Reveal Mutations in TREM2 Presenting as a Frontotemporal Dementia–like Syndrome Without Bone Involvement. JAMA Neurol. 2013, 70, 78–84.
- Bock, V.; Botturi, A.; Gaviani, P.; Lamperti, E.; Maccagnano, C.; Piccio, L.; Silvani, A.; Salmaggi, A. Polycystic Lipomembranous Osteodysplasia with Sclerosing Leukoencephalopathy (PLOSL): A new report of an Italian woman and review of the literature. J. Neurol. Sci. 2013, 326, 115–119.
- Le Ber, I.; De Septenville, A.; Guerreiro, R.; Bras, J.; Camuzat, A.; Caroppo, P.; Lattante, S.; Couarch, P.; Kabashi, E.; Bouya-Ahmed, K.; et al. Homozygous TREM2 mutation in a family with atypical frontotemporal dementia. Neurobiol. Aging 2014, 35, 2419.e23–2419.e25.
- Matsuo, T.; Suetsugu, M.; Eguchi, M.; Sasaki, M.; Tsuneyoshi, M. Membranous lipodystrophy. A case report. Arch Psychiatr. Nervenkr. 1982, 231, 123–130.
- Hakola, H.P. Neuropsychiatric and genetic aspects of a new hereditary disease characterized by progressive dementia and lipomembranous polycystic osteodysplasia. Acta Psychiatr. Scand. Suppl. 1972, 232, 1–73.
- Nwawka, O.K.; Schneider, R.; Bansal, M.; Mintz, U.N.; Lane, J. Membranous lipodystrophy: Skeletal findings on CT and MRI. Skelet. Radiol. 2014, 43, 1449–1455.
- Hakola, H.P.; Partanen, V.S. Neurophysiological findings in the hereditary presenile dementia characterised by polycystic lipomembranous osteodysplasia and sclerosing leukoencephalopathy. J. Neurol. Neurosurg. Psychiatry 1983, 46, 515–520.
- Bird, T.D.; Koerker, R.M.; Leaird, B.J.; Vlcek, B.W.; Thorning, D.R. Lipomembranous polycystic osteodysplasia (brain, bone, and fat disease): A genetic cause of presenile dementia. Neurology 1983, 33, 81.
- Shibata, K.; Uchiyama, S.; Takeuchi, M.; Kobayashi, I.; Maruyama, S. A case of membranous lipodystrophy (Nasu) with diffuse cerebral, white matter involvement and cerebellar atrophy on brain CT and NM (in Japanese). Rinsho Shinkeigaku 1990, 30, 1232–1237.
- Araki, T.; Ohba, H.; Monzawa, S.; Sakuyama, K.; Hachiya, J.; Seki, T.; Takahashi, Y.; Yamaguchi, M. Membranous lipodystrophy: MR imaging appearance of the brain. Radiology 1991, 180, 793–797.
- Coomans, C.; Sieben, A.; Lammens, M.; Groote, C.C.-D.; Vandenbroecke, C.; Goethals, I.; Van Melkebeke, D.; Hemelsoet, D. Early-onset dementia, leukoencephalopathy and brain calcifications: A clinical, imaging and pathological comparison of ALSP and PLOSL/Nasu Hakola disease. Acta Neurol. Belg. 2018, 118, 607–615.
- Takeshita, T.; Kaminaga, T.; Tatsumi, T.; Hatanaka, Y.; Furui, S. Regional cerebral blood flow in a patient with Nasu-Hakola disease. Ann. Nucl. Med. 2005, 19, 309–312.
- Hakola, H.P.A.; Iivanainen, M. A new hereditary disease with progressive dementia and polycystic osteodysplasia: Neuroradiological analysis of seven cases. Neuroradiology 1973, 6, 162–168.
- Klunemann, H.H.; Ridha, B.H.; Magy, L.; Wherrett, J.R.; Hemelsoet, D.; Keen, R.W.; De Bleecker, J.L.; Rossor, M.; Marienhagen, J.; Klein, H.E.; et al. The genetic causes of basal ganglia calcification, dementia, and bone cysts: DAP12 and TREM2. Neurology 2005, 64, 1502–1507.
- Sageshima, M.; Masuda, H.; Kawamura, K.; Shozawa, T. Membranous lipodystrophy. Light and electron microscopic study of a biopsy case. Acta Pathol. Jpn. 1987, 37, 281–290.
- Machinami, R. Degenerative change of adipose tissue; the so-called membranous lipodystrophy. Virchows Arch. 1990, 416, 373–374.
- Mii, Y.; Miyauchi, Y.; Yoshikawa, T.; Honoki, K.; Aoki, M.; Tsutsumi, M.; Maruyama, H.; Funauchi, M.; Konishi, Y.; Tamai, S. Ultrastructural lipid and glycoconjugate cytochemistry of membranous lipodystrophy (Nasu-Hakola disease). Virchows Arch. 1991, 419, 137–142.
- Shboul, M.; Roschger, P.; Ganger, R.; Paschalis, L.; Rokidi, S.; Zandieh, S.; Behunova, J.; Muschitz, C.; Fahrleitner-Pammer, A.; Ng, A.Y.J.; et al. Bone matrix hypermineralization associated with low bone turnover in a case of Nasu-Hakola disease. Bone 2018, 123, 48–55.
- Yagishita, S.; Ito, Y.; Sakai, H.; Amano, N. Membranocystic lesions of the lung in Nasu-Hakola disease. Virchows Arch. 1985, 408, 211–217.
- Tanaka, J. Nasu-Hakola disease: A review of its leukoencephalopathic and membranolipodystrophic features. Neuropathology 2000, 20, 25–29.
- Aoki, N.; Tsuchiya, K.; Togo, T.; Kobayashi, Z.; Uchikado, H.; Katsuse, O.; Suzuki, K.; Fujishiro, H.; Arai, T.; Iseki, E.; et al. Gray matter lesions in Nasu-Hakola disease: A report on three autopsy cases. Neuropathology 2010, 31, 135–143.
- Kalimo, H.; Sourander, P.; Jarvi, O.; Hakola, P. Vascular changes and blood-brain barrier damage in the pathogenesis of polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy (membranous lipodystrophy). Acta. Neurol. Scand. 1994, 89, 353–356.
- Matsushita, M.; Oyanagi, S.; Hanawa, S.; Shiraki, H.; Kosaka, K. Nasu-Hakola’s disease (membranous lipodystrophy). Acta Neuropathol. 1981, 54, 89–93.
- Miyazu, K.; Kobayashi, K.; Fukutani, Y.; Nakamura, I.; Hasegawa, H.; Yamaguchi, N.; Saitoh, T. Membranous lipodystrophy (Nasu-Hakola disease) with thalamic degeneration: Report of an autopsied case. Acta Neuropathol. 1991, 82, 414–419.
- Satoh, J.-I.; Kino, Y.; Yanaizu, M.; Saito, Y. Alzheimer’s disease pathology in Nasu-Hakola disease brains. Intractable Rare Dis. Res. 2018, 7, 32–36.
- Maderna, E.; Visonà, S.; Bolcato, V.; Redaelli, V.; Caroppo, P.; Montalbetti, L.; Giaccone, G.; Osculati, A. Neuropathological Alzheimer’s Disease Lesions in Nasu-Hakola Disease with TREM2 Mutation: Atypical Distribution of Neurofibrillary Changes. J. Alzheimer’s Dis. 2021, 79, 25–30.
- Yokoi, S.; Suzuki, K.; Amano, N.; Yagishita, S. Fatty Acid Analysis of Galactolipids and Ganglioside in the Brains of Four Cases of Nasu-Hakola Disease. Psychiatry Clin. Neurosci. 1989, 43, 695–701.
- Iannaccone, S.; Ferini-Strambi, L.; Nemni, R.; Marchettini, P.; Corbo, M.; Pinto, P.; Smirne, S. Pheripheral motor-sensory neuropathy in membranous lipodystrophy (Nasu’s disease): A case report. Clin. Neuropathol. 1992, 11, 49–53.
