A very low-calorie ketogenic diet (VLCKD) is characterized by low daily caloric intake (less than 800 kcal/day), low carbohydrate intake (<50 g/day) and normoproteic (1–1.5 g of protein/kg of ideal body weight) contents. It induces a significant weight loss and an improvement in lipid parameters, blood pressure, glycaemic indices and insulin sensitivity in patients with obesity and type 2 diabetes mellitus. Cushing’s syndrome (CS) is characterized by an endogenous or exogenous excess of glucocorticoids and shows many comorbidities including cardiovascular disease, obesity, type 2 diabetes mellitus and lipid disorders.
- Cushing’s syndrome
- glucocorticoid
- cortisol
- diabetes mellitus
- obesity
1. Introduction
2. Cushing’s Syndrome
CS is characterized by an excess of GCs that can be exogenous due to a chronic intake of corticosteroids or endogenous owing to the pituitary or adrenal hyperproduction of ACTH or cortisol, respectively. Rarely, the endogenous form can result from an extra-pituitary ACTH-secreting tumour (ectopic CS) [11]. CS is associated with increased mortality and a high risk of cardiovascular disease due to the presence of several comorbidities [12,13,14,15,16][12][13][14][15][16]. Comorbidities of CS include metabolic syndrome, characterized by systemic arterial hypertension, visceral obesity, impaired glucose metabolism and dyslipidaemia, polycystic ovary syndrome (PCOS), musculoskeletal disorders, such as myopathy, osteoporosis and skeletal fractures, infections, neuropsychiatric disorders, such as impaired cognitive function, depression or mania, impaired reproductive and sexual function and dermatological manifestations, represented mainly by acne, hirsutism and alopecia [14,15,16,17,18][14][15][16][17][18]. The therapeutic approach consists of surgery as the first-line therapy. When patients refuse surgery or it is contraindicated or when a relapse occurs, other therapeutic options including medical therapy, radiotherapy or bilateral adrenalectomy should be evaluated [19,20][19][20]. Medical therapy mainly consists of drugs directly inhibiting pituitary ACTH secretion, such as pasireotide and cabergoline, or adrenal steroidogenesis inhibitors such as metyrapone, ketoconazole, osilodrostat, mitotane and etomidate [21,22][21][22]. Another medical drug is the glucocorticoid receptor (GR) antagonist mifepristone, which impairs cortisol binding to GR and mainly acts on clinical comorbidities [23]. However, obtaining remission in CS is not always possible and sometimes it is necessary to combine the treatment options. In addition, these patients tend to show the metabolic comorbidities for a long time, sometimes even in the remission phase, and therefore a nutritional approach to improve metabolism should be started.Nutrition and Cushing’s Syndrome
2.1. Nutrition and Cushing’s Syndrome
Generally speaking, patients with CS need a low sodium, high-protein and high-calcium diet to prevent muscle and bone loss, respectively. However, an interesting and complex relationship exists between diet macronutrients and cortisol [24]. Meal macronutrients have a strong influence on cortisol concentrations, reducing or increasing their levels [25,26,27,28][25][26][27][28]. Long-standing studies have shown that fasting and starvation are associated with an increase in serum, salivary and urinary free cortisol levels and inadequate suppression of cortisol after a low dose dexamethasone test [29,30,31,32][29][30][31][32]. However, to what degree caloric restriction cortisol levels increased was not ascertained in any study [33,34][33][34]. The sympathetic nervous system (SNS) and hypothalamic–pituitary–adrenal axis (HPA) are strictly involved in stress management. An unhealthy behaviour (consumption of highly rich carbohydrate food, chronic stress and reduced sleep) may stimulate cortisol secretion with the development of obesity in subjects who are predisposed for it [35]. By contrast, calorie-restricted diets inducing a decrease in cortisol values are associated with weight loss and reduced chronic inflammation [36]. There are a few clinical studies evaluating the effects of calorie restriction on cortisol levels. Stimson et al. evaluated the effects of a high-fat/low-carb diet vs. a moderate-fat/moderate-carb diet on cortisol metabolism in obese men [37]. They showed that a lower carb diet was able to regenerate cortisol by increasing the enzyme 11-β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) that activates cortisol and reducing the enzymes (5-alpha and 5-beta reductase) that inactivate cortisol. Other improvements seen in the lower carb group were greater weight loss and improvements in glucose and insulin levels. The regeneration of cortisol in the low-carb group was independent of the difference in caloric intake between the low-carb and the high-carb group, meaning that the number of calories consumed was not a factor in the positive changes seen; rather, it was the carb ratio in the diet that made the difference. Another study by the same authors showed that dietary macronutrients have different effects on cortisol production [38]. They conducted a study on eight lean men and observed the effects of carbohydrate, high-protein and fat meals on insulin and cortisol levels, showing that all these meals stimulate a rise in cortisol levels, in different ways. Indeed, carbohydrates stimulate both the adrenal cortisol secretion and the extra-adrenal cortisol regeneration mediated by 11β-HSD1, which is present in the liver, adipose tissue and brain, and regenerate cortisol from cortisone releasing it into the bloodstream. By contrast, high-protein and fat meals stimulate adrenal cortisol secretion to a greater degree than extra-adrenal regeneration. The extra-adrenal cortisol regeneration is strictly related to the increase in insulin levels. Interestingly, a meta-analysis conducted on 13 studies analysed the effects of fasting, a very low-calorie diet (VLCD) and a low-calorie diet (LCD) on serum cortisol levels [39]. This meta-analysis only included studies that evaluated serum cortisol levels, while it excluded those based on salivary or urinary cortisol levels, in order to avoid heterogeneity of the studies. The results of the meta-analysis showed that short-term calorie restriction was more associated with an increase in cortisol values, compared to a VLCD and LCD, which, in turn, had no long-term effects on serum cortisol values and were less stressful than fasting. In addition, carbohydrate restriction was associated with a decrease in insulin concentration, leading to extra-adrenal cortisol synthesis [39]. Furthermore, some amino acids, such as tryptophan, can lead to a decrease in cortisol levels [40]. Similarly, supplementation with phospholipids at the dose of at least 400 mg/day also results in a reduction in cortisol levels [41]. In addition, other nutrients including vitamin B6 and B12, folic acid, lithium, taurine, fermented milk products and sprouts of brown rice, barley and beans, which stimulate the GABAergic system, in turn, can reduce the secretion of CRH, leading to a decrease in cortisol levels [24,41,42,43][24][41][42][43].3. Ketogenic Diet
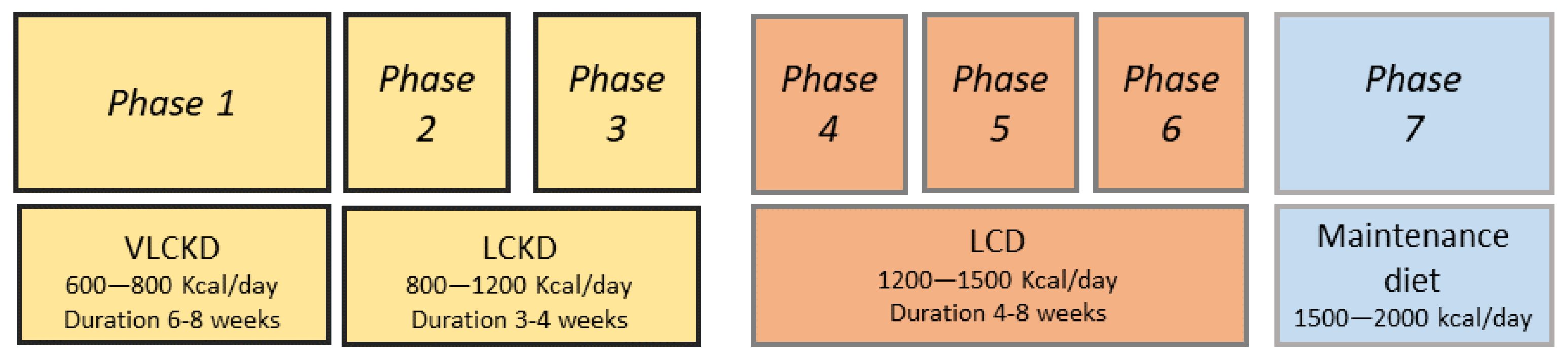
The ketogenic diet (KD) was used for the first time for the treatment of epilepsy in 1921 [44]. Its use was proposed to mimic the effects of fasting. The KD is a high-fat, low carbohydrate, normocaloric diet. It is characterized by a 4:1 ratio of fat to protein, plus carbohydrates and about 90% of calories are provided by fats (Table 1). In the scenario of the use of a KD, some variants can be identified, the low-calorie ketogenic diet (LCKD) with a calorie intake of 800–1200 Kcal/day and the very-low-calorie ketogenic diet (VLCKD) with a calorie intake of less than 800 Kcal/day (Table 1) [45].KD | LCKD | VLCKD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Caloric intake | Normocaloric | 800–1200 Kcal/day | <800 Kcal/day | ||||||||
Carbohydrate (%) | 5–10 | 13 | 13 | ||||||||
Protein (%) | 15–20 | 29 | 44 | ||||||||
Fat (%) | 70–80 | 58 | 43 | ||||||||
Foods | Vegetable oils, fish, eggs, meat, cheese, olives, avocado, coconut | Natural high biological value proteins (1–2 servings) including meat, fish, eggs, processed meat | Replacement meals with high biological value proteins composed by 18 g of proteins, 4 g of carbohydrates and 3 g of fats | ||||||||
Recommendations for use [1] |
|
|
|
4. VLCKD
References
- Kirkpatrick, C.F.; Bolick, J.P.; Kris-Etherton, P.M.; Sikand, G.; Aspry, K.E.; Soffer, D.E.; Willard, K.E.; Maki, K.C. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J. Clin. Lipidol. 2019, 13, 689–711.e1.
- Muscogiuri, G.; El Ghoch, M.; Colao, A.; Hassapidou, M.; Yumuk, V.; Busetto, L.; Obesity Management Task Force (OMTF) of the European Association for the Study of Obesity (EASO). European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes. Fact. 2021, 14, 222–245.
- Muscogiuri, G.; Barrea, L.; Laudisio, D.; Pugliese, G.; Salzano, C.; Savastano, S.; Colao, A. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J. Transl. Med. 2019, 17, 356.
- Kolb, H.; Kempf, K.; Röhling, M.; Lenzen-Schulte, M.; Schloot, N.C.; Martin, S. Ketone bodies: From enemy to friend and guardian angel. BMC Med. 2021, 19, 313.
- Boden, G.; Sargrad, K.; Homko, C.; Mozzoli, M.; Stein, T.P. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann. Intern. Med. 2005, 142, 403–411.
- Dashti, H.M.; Mathew, T.C.; Khadada, M.; Al-Mousawi, M.; Talib, H.; Asfar, S.K.; Behbahani, A.I.; Al-Zaid, N.S. Beneficial effects of ketogenic diet in obese diabetic subjects. Mol. Cell. Biochem. 2007, 302, 249–256.
- Gupta, L.; Khandelwal, D.; Kalra, S.; Gupta, P.; Dutta, D.; Aggarwal, S. Ketogenic diet in endocrine disorders: Current perspectives. J. Postgrad. Med. 2017, 63, 242–251.
- Barañano, K.W.; Hartman, A.L. The ketogenic diet: Uses in epilepsy and other neurologic illnesses. Curr. Treat. Options Neurol. 2008, 10, 410–419.
- Thammongkol, S.; Vears, D.F.; Bicknell-Royle, J.; Nation, J.; Draffin, K.; Stewart, K.G.; Ingrid, E.; Scheffer, E.; Mackay, M.T. Efficacy of the ketogenic diet: Which epilepsies respond? Epilepsia 2012, 53, e55–e59.
- Rubini, A.; Bosco, G.; Lodi, A.; Cenci, L.; Parmagnani, A.; Grimaldi, K.; Zhongjin, Y.; Paoli, A. Effects of twenty days of the ketogenic diet on metabolic and respiratory parameters in healthy subjects. Lung 2015, 193, 939–945.
- Pivonello, R.; De Martino, M.C.; Iacuaniello, D.; Simeoli, C.; Muscogiuri, G.; Carlomagno, F.; De Leo, M.; Cozzolino, A.; Colao, A. Metabolic Alterations and Cardiovascular Outcomes of Cortisol Excess. Front. Horm. Res. 2016, 46, 54–56.
- Nieman, L.K. Hypertension and Cardiovascular Mortality in Patients with Cushing Syndrome. Endocrinol. Metab. Clin. N. Am. 2019, 48, 717–725.
- Barbot, M.; Zilio, M.; Scaroni, C. Cushing’s syndrome: Overview of clinical presentation, diagnostic tools and complications. Best Pract. Res. Clin. Endocrinol. Metab. 2020, 34, 101380.
- Giordano, C.; Guarnotta, V.; Pivonello, R.; Amato, M.C.; Simeoli, C.; Ciresi, A.; Cozzolino, A.; Colao, A. Is diabetes in Cushing’s syndrome only a consequence of hypercortisolism? Eur. J. Endocrinol. 2013, 170, 311–319.
- Ragnarsson, O. Cushing’s syndrome—Disease monitoring: Recurrence, surveillance with biomarkers or imaging studies. Best Pract. Res. Clin. Endocrinol. Metab. 2020, 34, 101382.
- Ferriere, A.; Tabarin, A. Cushing’s syndrome: Treatment and new therapeutic approaches. Best Pract. Res. Clin. Endocrinol. Metab. 2020, 34, 101381.
- Guarnotta, V.; Prinzi, A.; Pitrone, M.; Pizzolanti, G.; Giordano, C. Circulating Irisin Levels as a Marker of Osteosarcopenic-Obesity in Cushing’s Disease. Diabetes Metab. Syndr. Obes. 2020, 13, 1565–1574.
- Braun, L.T.; Vogel, F.; Reincke, M. Long-term morbidity and mortality in patients with Cushing’s syndrome. J. Neuroendocrinol. 2022, 4, e13113.
- Castinetti, F. Medical management of Cushing’s disease: When and how? J. Neuroendocrinol. 2022, 15, e13120.
- Pivonello, R.; Ferrigno, R.; De Martino, M.C.; Simeoli, C.; Di Paola, N.; Pivonello, C.; Barba, L.; Negri, M.; De Angelis, C.; Colao, A. Medical Treatment of Cushing’s Disease: An Overview of the Current and Recent Clinical Trials. Front. Endocrinol. 2020, 11, 648.
- Tritos, N.A. Adrenally Directed Medical Therapies for Cushing Syndrome. J. Clin. Endocrinol. Metab. 2021, 106, 16–25.
- Brown, D.R.; East, H.E.; Eilerman, B.S.; Gordon, M.B.; King, E.E.; Knecht, L.A.; Salke, B.; Samson, S.L.; Yuen, K.C.J.; Yau, H. Clinical management of patients with Cushing syndrome treated with mifepristone: Consensus recommendations. Clin. Diabetes Endocrinol. 2020, 6, 18.
- Stachowicz, M.; Lebiedzińska, A. The effect of diet components on the level of cortisol. Eur. Food Res. Technol. 2016, 242, 2001–2009.
- Lemmens, S.; Born, J.M.; Martens, E.A.; Martens, M.J.; Westerterp Plantenga, M.S. Influence of consumption of a high-protein vs. high-carbohydrate meal on the physiological cortisol and psychological mood response in men and women. PLoS ONE 2011, 6, e16826.
- Peeters, F.; Nicholson, N.A.; Berkhof, J. Cortisol responses to daily events in major depressive disorder. Psychosom. Med. 2003, 65, 836–841.
- Martens, M.J.; Rutters, F.; Lemmens, S.G.; Born, J.M.; Westerterp-Plantenga, M.S. Effects of single macronutrients on serum cortisol concentrations in normal weight men. Physiol. Behav. 2010, 101, 563–567.
- Bray, G.A.; Most, M.; Rood, J.; Redmann, S.; Smith, S.R. Hormonal responses to a fast-food meal compared with nutritionally comparable meals of different composition. Ann. Nutr. Metab. 2007, 51, 163–171.
- Galvao-Teles, A.; Graves, L.; Burke, C.W.; Fotherby, K.; Fraser, R. Free cortisol in obesity; effect of fasting. Acta Endocrinol. 1976, 81, 321–329.
- Edelstein, C.K.; Roy-Byrne, P.; Fawzy, F.I.; Dornfeld, L. Effects of weight loss on the dexamethasone suppression test. Am. J. Psychiatry 1983, 140, 338–341.
- Berger, M.P.K.; Doerr, P.; Krieg, C.; von Zersseen, D. Influence of weight loss on the dexamethasone suppression test. Arch. Gen. Psychiatry 1983, 19, 585–586.
- Tomiyama, A.J.; Mann, T.; Vinas, D.; Hunger, J.M.; Dejager, J.; Taylor, S.E. Low calorie dieting increases cortisol. Psychosom. Med. 2010, 72, 357–364.
- Dubuc, G.R.; Phinney, S.D.; Stern, J.S.; Havel, P.J. Changes of serum leptin and endocrine and metabolic parameters after 7 days of energy restriction in men and women. Metab. Clin. Exp. 1998, 47, 429–434.
- Pasiakos, S.M.; Caruso, C.M.; Kellogg, M.D.; Kramer, F.M.; Lieberman, H.R. Appetite and endocrine regulators of energy balance after 2 days of energy restriction: Insulin, leptin, ghrelin, and DHEA-S. Obesity 2011, 19, 1124–1130.
- van der Valk, E.S.; Savas, M.; van Rossum, E.F.C. Stress and obesity: Are there more susceptible individuals? Curr. Obes. Rep. 2018, 7, 193–203.
- Valenzano, A.; Polito, R.; Trimigno, V.; Di Palma, A.; Moscatelli, F.; Corso, G.; Sessa, F.; Salerno, M.; Montana, A.; Di Nunno, N.; et al. Effects of very low calorie ketogenic diet on the orexinergic system, visceral adipose tissue, and ROS production. Antioxidants 2019, 8, 643.
- Polito, R.; Messina, G.; Valenzano, A.; Scarinci, A.; Villano, I.; Monda, M.; Cibelli, G.; Porro, C.; Pisanelli, D.; Monda, V.; et al. The Role of Very Low Calorie Ketogenic Diet in Sympathetic Activation through Cortisol Secretion in Male Obese Population. J. Clin. Med. 2021, 10, 4230.
- Stimson, R.H.; Johnstone, A.M.; Homer, N.Z.; Wake, D.J.; Morton, N.M.; Andrew, R.; Lobley, G.E.; Walker, B.R. Dietary macronutrient content alters cortisol metabolism independently of body weight changes in obese men. J. Clin. Endocrinol. Metab. 2007, 92, 4480–4484.
- Stimson, R.H.; Mohd-Shukri, N.A.; Bolton, J.L.; Andrew, R.; Reynolds, R.M.; Walker, B.R. The postprandial rise in plasma cortisol in men is mediated by macronutrient-specific stimulation of adrenal and extra-adrenal cortisol production. J. Clin. Endocrinol. Metab. 2014, 99, 160–168.
- Nakamura, Y.; Walker, B.R.; Ikuta, T. Systematic review and meta-analysis reveals acutely elevated plasma cortisol following fasting but not less severe calorie restriction. Stress 2016, 19, 151–157.
- Capello, A.E.; Marcus, C.R. Effect of sub chronic tryptophan supplementation on stress-induced cortisol and appetite in subjects differing in 5-HTTLPR genotype and trait neuroticism. Psychoneuroendocrinology 2014, 45, 96–107.
- Starks, M.A.; Starks, S.L.; Kingsley, M.; Purpura, M.; Jager, R. The effects of phosphatidylserine on endocrine response to moderate intensity exercise. J. Int. Soc. Sports Nutr. 2008, 5, 11–17.
- Miklos, I.H.; Kovacs, K.J. GABAergic innervation of corticotropin-releasing hormone (CRH)-secreting parvocellular neurons and its plasticity as demonstrated by quantitative immunoelectron micorscopy. Neuroscience 2002, 113, 581–592.
- Song, Z.; Hatton, G.I. Taurine and the control of basal hor mone release from rat neurophysis. Exp. Neurol. 2003, 183, 330–337.
- Wilder, R.M. The effects of ketonemia on the course of epilepsy. Mayo Clin. Proc. 1921, 2, 307–308.
- Sukkar, S.G.; Muscaritoli, M. A Clinical Perspective of Low Carbohydrate Ketogenic Diets: A Narrative Review. Front. Nutr. 2021, 8, 642628.
- Abbasi, J. Interest in the ketogenic diet grows for weight loss and type 2 diabetes. JAMA 2018, 319, 215–217.
- Merra, G.; Gratteri, S.; De Lorenzo, A.; Barrucco, S.; Perrone, M.A.; Avolio, E.; Bernardini, S.; Marchetti, M.; Di Renzo, L. Effects of very-low-calorie diet on body composition, metabolic state, and genes expression: A randomized double-blind placebo-controlled trial. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 329–345.
- Paoli, A.; Rubini, A.; Volek, J.S.; Grimaldi, K.A. Beyond weight loss: A review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur. J. Clin. Nutr. 2013, 67, 789–796.
- Cicero, A.F.; Benelli, M.; Brancaleoni, M.; Dainelli, G.; Merlini, D.; Negri, R. Middle and long-term impact of a very low-carbohydrate ketogenic diet on cardiometabolic factors: A multi-center, cross-sectional, clinical study. High Blood Press Cardiovasc. Prev. 2015, 22, 389–394.
- Merra, G.; Miranda, R.; Barrucco, S.; Gualtieri, P.; Mazza, M.; Moriconi, E.; Marchetti, M.; Chang, T.F.M.; De Lorenzo, A.; Di Renzo, L. Very-low-calorie ketogenic diet with aminoacid supplement versus very low restricted-calorie diet for preserving muscle mass during weight loss: A pilot double-blind study. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 2613–2621.
- Antonio, J.; Ellerbroek, A.; Silver, T.; Vargas, L.; Tamayo, A.; Buehn, R.; Peacock, C.A. A high protein diet has no harmful efects: A oneyear crossover study in resistance-trained males. J. Nutr. Metab. 2016, 2016, 9104792.
- Lafel, L. Ketone bodies: A review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab. Res. Rev. 1999, 15, 412–426.
- McPherson, P.A.; McEneny, J. The biochemistry of ketogenesis and its role in weight management, neurological disease and oxidative stress. J. Physiol. Biochem. 2012, 68, 141–151.
- Dehghan, M.; Mente, A.; Zhang, X.; Swaminathan, S.; Li, W.; Mohan, V.; Iqbal, R.; Kumar, R.; Wentzel-Viljoen, E.; Rosengren, A.; et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 2017, 390, 2050–2062.
- Currenti, W.; Galvano, F. Very low-calorie ketogenic diet (VLCKD): Indicazioni ed efficacia nel trattamento dell’obesità. L’Endocrinologo 2020, 21, 458–463.
