Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Ivan Santolalla Arnedo and Version 2 by Amina Yu.
Suicide is a serious health problem affecting people of all ages and in all countries. Suicide prevention, listed by the World Health Organisation (WHO) as a global imperative, has grown in importance in recent years to become a priority task in global public health. Suicide death rates are high, with an estimated 800,000 deaths by suicide each year.
- suicide
- prevention
- risk factors
- health care plan/programme
1. Health care Plans as a Preventive Measure against Suicide
National prevention strategies must be resourced and periodically re-evaluated to take account of evolving societal changes [1]. In addition to these strategies, health plans for suicide prevention developed by each province are essential to reinforce general preventive measures and adapt them to the type of population and resources of each community [2][6]. The elaboration of these preventive strategies and plans is a highly relevant act of research and data collection as measures are put in place. This allows the identification of at-risk and vulnerable groups; of the needs of the population; of gaps in current knowledge; and of the main risk, precipitating and protective factors for each group. This allows interventions to be tailored according to the needs of the provinces [1][2][1,6].
The year 2020 was the year with the highest number of suicides in the history of Spain since data have been recorded, totalling 3941 people, which is an average of 11 suicides per day or one every 2.2 h [3][4][7,8]. This is why it is necessary to review the literanture in order to analyse and discern points for improvement.
Suicide prevention involves not only the health sector, but also several key sectors such as social services, education and politics, as well as society as a whole. Therefore, the WHO encourages governments to invest in multisectoral strategies to reduce the rates of suicide deaths and suicide attempts [1].
Since 2000, several countries have developed preventive strategies against suicide. Spain is one of them, having created the Clinical Practice Guideline for the Prevention and Treatment of Suicidal Behaviour in 2012, which was revised in 2020 by a group of experts who considered maintaining the validity of the proposed interventions [5][9]. This guide addresses important issues such as the care and attention of the different sectors involved, as well as preventive measures. It also includes screening and identification of risk groups, promotion of the development of protective factors, restriction of access to lethal means, training programmes for health and non-health personnel, information for media professionals, care for family members and relatives and the development of diagnostic and therapeutic strategies [5][6][9,10]. In Spain, all provinces agree with the statement published by the WHO declaring suicide and its associated behaviours as preventable acts if appropriate measures are taken in the vulnerable population [7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29][11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33].
2. General Interventions
In the group of general interventions, the plans of the province of Asturias and Castilla y León are excluded as they are documents aimed at health professionals and, therefore, their interventions are focused on this area [11][15][15,19]. Awareness-raising among the general population is applied in all provinces and cities except the Balearic Islands, which focuses on other preventive aspects. To promote public awareness, most communities propose activities on key days related to suicide such as 10 September (World Suicide Prevention Day) and actions to improve the detection of suicidal risk in order to enable the population to recognise risk factors and enable the early detection of suicidal ideation. On the other hand, the population is also provided with truthful information and scientific evidence on social networks and official websites, in addition to the fact that most communities are equipped with an extensive infrastructure for telephone assistance and help contacts. The province of Aragon focuses especially on telematic care and the use of new technologies to raise awareness among the general population due to the arrival of the pandemic caused by COVID-19 [9][10][11][13][14][15][16][17][18][19][20][21][22][23][24][25][26][13,14,15,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. The regions of Extremadura and Murcia, on the other hand, only include in this section the detection of risk factors in vulnerable groups [21][24][25,28]. Approximately 65% of the communities (Andalusia, Aragon, Balearic Islands, Canary Islands, Cantabria, Galicia, La Rioja, Madrid, Navarre, Basque Country and Valencia) mention among their general interventions the importance of placing restrictions on potentially lethal means. These measures are comprehensive in nature as they integrate several aspects. All the plans that mention measures related to restricting access to lethal means agree that the epidemiology of suicide in the area must be known in order to prevent the development of new cases that follow the same methodology of suicide [7][8][9][10][12][13][14][22][23][27][28][29][30][31][32][33][34][35][11,12,13,14,16,17,18,26,27,31,32,33,34,35,36,37,38,39]. Several communities add the surveillance of dangerous places considered as “suicide black spots” due to the accumulation of several deaths due to suicide. Architectural barriers are proposed to be installed to prevent and/or hinder access to these sites, as most of them are high-rise areas [8][9][10][12][22][36][37][3,5,12,13,14,16,26]. Pharmacological control and vigilance are closely related to health interventions, consisting of ensuring that the medication guidelines for people at risk of suicide are correct and appropriate. In relation to the control of doses and their administration, preventive measures are mentioned in the plans of 8 of the 17 provinces: Andalusia, Aragon, Balearic Islands, Galicia, La Rioja, Madrid, Navarre and the Basque Country. The province of Madrid lists control of access to drugs as its main measure in terms of restricting access to lethal drugs [7][8][9][10][12][22][23][25][26][11,12,13,14,16,26,27,29,30]. Inter-institutional coordination is essential for the development of preventive measures, both in the health system and at the social level. This is why almost 83% of the provinces include this aspect among the proposed interventions. Most of them propose the improvement of their coordination strategies both at a territorial level and between the different disciplines related to the detection and approach to suicide and related behaviours. The main institutions referred to by most communities are health centres, educational centres, socio-health centres and security forces, such as police or fire brigades. Collaboration with prisons and coordination with the state and public administrations in arranging new measures such as patient associations or mutual help groups are also mentioned [8][9][10][13][14][16][17][18][19][20][21][22][23][24][25][26][27][12,13,14,17,18,20,21,22,23,24,25,26,27,28,29,30,31]. Some provinces have created, or propose to create, the formation of working groups whose functions are exclusively aimed at guaranteeing and monitoring coordination between the different bodies and services involved in order to improve suicide prevention [7][22][25][26][11,26,29,30]. Asturias, in proposing a prevention plan focused on health care, establishes coordination measures, but refers only to the different points of health care and the relationship of continuity that they should have [11][15]. The measures proposed for the development of a suicide prevention plan in the Balearic Islands’ Strategic Plan for Mental Health concern broader measures, but coincide with Asturias in terms of the health care approach to coordination [12][16]. More than half of the Spanish provinces agree on the need to improve research related to suicide and self-injurious behaviour. In this way, facilities are proposed to prevent suicide in vulnerable people or those with associated pathologies such as depression. Alongside this improved research, epidemiological surveillance and its major impact on the effectiveness of preventive interventions within the community are discussed. To this end, the communities of Aragon, Baleares, Canarias, Cantabria, Castilla La Mancha, Cataluña, Extremadura, Galicia, La Rioja, Madrid, Navarre, País Vasco and Valencia allude to an improvement in recording cases of death by suicide by means of periodic reports or data-recording strategies such as the use of psychological highways, this being the technique that is most frequently reiterated throughout the plans presented [7][9][10][12][13][14][16][17][18][19][20][21][22][23][25][26][27][28][29][30][11,13,14,16,17,18,20,21,22,23,24,25,26,27,29,30,31,32,33,34]. To strengthen epidemiological surveillance, the Spanish Foundation for Suicide Prevention has created an organisation, the Spanish Suicide Observatory, whose mission encompasses the analysis and dissemination of epidemiological data related to suicide in order to enable its prevention. Many of the provinces have decided to create a Suicide Observatory at the provincial level to extract data specific to their area [3][7].3. Training Interventions
The communities of Asturias and Castilla y León, as in the group of general interventions, are excluded from the group of training interventions, focusing only on how to deal with a crisis situation on the part of health personnel [11][15][15,19]. The most frequently mentioned risk group with which training activities are intended to be carried out is the school environment. All communities except Asturias, Cantabria, Castilla y León, Extremadura, Madrid and Murcia propose workshops and courses aimed at both schoolteachers and pupils. The main objective of these training workshops is to train teachers to detect and deal with possible cases of suicidal behaviour and crisis situations, in order to increase their knowledge related to the identification of risk factors and the strengthening of protective factors, as well as to guide students not only in the detection of possible cases, but also in the correct mutual support among them, forming mutual help groups in the classroom and improving their coping skills [7][8][9][10][12][13][16][17][18][19][20][22][25][26][27][11,12,13,14,16,17,20,21,22,23,24,26,29,30,31]. The autonomous cities of Ceuta and Melilla consider strengthening emotional education from the school years onwards as a measure to be included in their future prevention plans [28][29][32,33]. In addition, training actions aimed at other groups such as adolescents, survivors in cases of death of a loved one due to suicide, the elderly and their informal carers, inmates in penitentiary centres and people in situations of discrimination or violence of any kind are mentioned. People suffering from Severe Mental Disorder (SMD) are added as one of the main vulnerable groups receiving the necessary information primarily from mental health centres [7][8][9][10][12][13][16][17][18][19][20][22][25][26][27][11,12,13,14,16,17,20,21,22,23,24,26,29,30,31]. The province of La Rioja includes the main activities to be carried out in schools, penitentiary centres, juvenile centres, centres for the elderly and in the field of forensic medicine [22][26]. In addition, the Suicide Prevention Strategy of Aragon includes the university population as a vulnerable group due to the psychological distress of students experiencing states of anxiety, social dysfunction and even symptoms compatible with depression [9][10][13,14]. Training aimed at health care professionals focuses on keeping current information up to date, as well as training staff to identify early risk and warning signs using indicators, improving clinical interview techniques to obtain more accurate information, making appropriate referrals between services by promoting coordination and agreeing on unified protocols and procedures. To this end, continuous face-to-face, blended and online training activities are presented [8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. Both the 17 provinces and the two autonomous cities agree to carry out these activities aimed at health personnel [8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29][12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. Asturias and Castilla y León, as mentioned in previous paragraphs, dedicate their plan exclusively to actions by the health sector in risk situations and do not explicitly mention training for this group. At the same time, they propose interventions for which this training is necessary, such as the use of the clinical interview or the recognition of risk factors [11][15][15,19]. It also shows the trend towards the development of training work among non-health professionals, which is defined in 12 of the 17 Spanish provinces. A general mention is made of the group of non-health professionals in relation to at-risk patients or vulnerable groups, although the importance of providing adequate training for social service workers, social health and security forces, including police and firefighters, is highlighted [7][8][12][13][14][17][20][22][23][25][26][27][11,12,16,17,18,21,24,26,27,29,30,31]. In addition, the strategy for suicide prevention in the Basque Country incorporates the promotion of psychological first aid in these interventions, as well as training aimed at staff providing telephone assistance to people at risk [26][30]. Finally, around 71% of the provinces include training interventions together with the dissemination of information and recommendations for the media, so that an adequate approach to suicide in the press is possible, one that does not have a negative impact on suicide rates [8][9][10][12][14][16][17][18][19][20][21][22][23][25][26][12,13,14,16,18,20,21,22,23,24,25,26,27,29,30]. One of the main concerns reported by the WHO is the ease with which the general population can access inappropriate information related to suicidal practices through the media and the internet. WHO includes the following objective among the components that should be included in national strategies: “Promote implementation of media guidelines to support responsible reporting of suicide in print, broadcasting and social media” [1][30][1,34]. The WHO document “Preventing suicide” emphasises collaboration and educational engagement with the media to achieve this goal. It also describes preventive measures related to responsible communication in the media, including interventions such as the use of responsible language; dissemination of information about available treatments; information about organisations, mobile apps and social networks as support mechanisms; and avoiding sensationalism, simplification or detailed description of the event [1].4. Health Interventions
To improve the rates of early detection of risk (Figure 13), all communities except the Balearic and Canary Islands agree that it is necessary to improve assessment techniques, mainly those used in the first care received by patients, in order to identify the problem as early as possible and the risk factors that may lead to suicidal behaviour and act accordingly [6][7][8][9][10][13][14][15][16][17][18][19][20][21][22][23][24][25][26][10,11,12,13,14,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. To this end, the plans of several communities focus on the risk assessment carried out in primary care and emergency and telephone services together with the emergency psychiatric assessment carried out by mental health professionals once an indication of risk has been detected at earlier points in the care chain, cited in the plans of Andalusia, Castilla y León, Catalonia and La Rioja [8][15][17][18][19][20][22][12,19,21,22,23,24,26].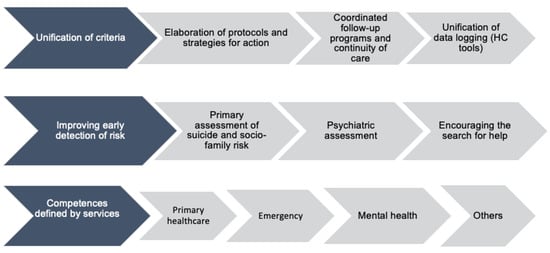
Figure 13.
Classification of health interventions.
