Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Eduardo Navarro Jiménez and Version 2 by Jessie Wu.
Cancer-related cachexia is a complex multifactorial phenomenon in which systemic inflammation plays a key role in the development and maintenance of the symptomatology. Pharmacological interventions seem to produce a positive effect on inflammatory state and cachexia. Nutritional interventions are focused on a high-energy diet with high-density foods and the supplementation with antioxidants, while physical activity is focused on strength-based training. The implementation of multidisciplinary non-pharmacological interventions in cancer-related cachexia could be an important tool to improve traditional treatments and improve patients’ quality of life.
- cancer
- cachexia
- exercise
1. Cancer Related Cachexia
Cachexia is a multifactorial syndrome characterized by its affection in different tissues, organs, and metabolic pathways. Its axis of pathological action begins with a process of systemic inflammation, which results in a progressive loss of the patient’s weight. In this loss, the main characteristic is negative body recomposition, increasing adipose tissue, and decreasing metabolically active tissue and lean muscle mass. This process can adversely affect patients during cancer treatment, reducing their tolerance and response to treatments, resulting in a loss of quality of life and increased mortality in patients with advanced cancer [1][24].
Clinically, cachexia is defined as a weight loss greater than 5% in the previous 6 months or corresponding to 2–5% for patients with a body mass index (BMI) ≤ 20 kg/m2 or with reduced muscle mass (sarcopenia) [2][25]. According to the authors of the recent reviews, its prevalence is estimated at 15.8/10,000 in Europe (2013), 16.5/10,000 in the United States (2014), and 13.4/10,000 in Japan [3][26]. Indeed, its epidemiology varies depending on the type of cancer. The prevalence is 80% in patients with pancreatic and gastric cancer; 60% in patients with colon cancer, prostate cancer, lung cancer, and non-Hodgkin’s lymphoma; and about 40% in patients with breast cancer, sarcoma, and leukemia. Moreover, it is considered to be indirectly associated with 20% of all cancer-related deaths [4][27].
The main pathological feature is the deterioration of lean muscle mass, sarcopenia. However, there are a greater number of factors which are related to the appearance of sarcopenia. For this, Figure 1 offers a quick overview of them. However, the affection is multi-organic, affecting the intestine, heart, kidneys, and liver function and morphology. With its progression, related pathologies may arise, such as cardiac arrhythmias, hypoventilation, thromboembolic events, and cardiorenal disorders [1][24]. Indeed, cardiac dysfunction is present in a high percentage of cancer cachexia-induced patients [5][28]. Thus, understanding the relationship between the heart and skeletal muscles in the clinical course of the patient with cancer cachexia is essential, linking established measures for its treatment and prevention.
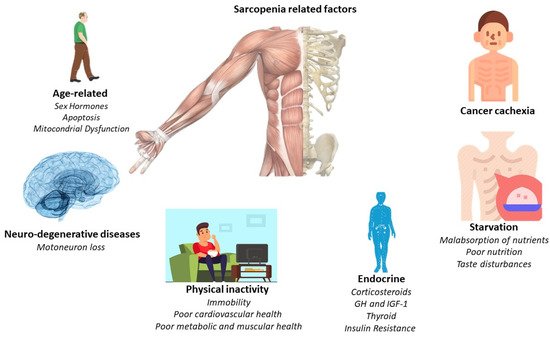
Figure 1.
Principal sarcopenia-related factors.
1.1. Pathological Changes Underlying Muscle Atrophy in Cancer Cachexia
The subjacent mechanisms of cancer cachexia are multiple and intertwined. Factors related to skeletal and cardiac muscles (myokines and cardiokines) or factors secreted by cancer and cancer-associated immune cells (TGF-β, DAMPSs, and LIF) trigger a cascade of processes that ultimately result in cachexia. Circulating factors, intracellular signaling pathways, and atrophic end effectors lead to cardiac and skeletal muscle atrophy. Although the biological processes underlying cardiac and skeletal muscle atrophy are similar, their relative contribution and the specific molecular players involved differ slightly: damage-associated molecular patterns (DAMPs), growth differentiation factor 15 (GDF15), IL interleukins, leukemia inhibitory factor LIF, tumor necrosis factor alpha TNF-α, and transforming growth factor beta TGF-β [4][27].
1.2. Signaling Pathways Involved in Muscle Atrophy
The activation of inflammatory cytokines, specifically TNF, IL-1, and IL-6, leads to activation of NF-κB and FOXO (Figure 2). Binding of IL-6 to its receptor induces STAT3 expression, leading to the activation of the NF-κB pathway. The autophagy–lysosome system is activated by the transcription factor FOXO. Activation of p38 and JAK/MAPK leads to caspase-mediated apoptosis. Myostatin also activates protein degradation through FOXO and can decrease protein synthesis by inhibiting AKT through SMAD. Levels of insulin-like growth factor-1 (IGF-1) decrease during muscle atrophy, suppressing the IGF-1 pathway, thus inhibiting protein synthesis. The ubiquitin–proteasome system (UPS) is initiated by transcription of the E3 ubiquitin ligases MuRF-1 and MAFbx/atrogin-1: ActRIIB, activin receptor type IIB; TNFα, tumor necrosis factor-α; IL, interleukin; JAK, Janus kinase; STAT, signal transducers and activators of transcription; FOXO, Forkhead box transcription factors; mTOR, mammalian target of rapamycin; NF κB, nuclear factor-κB; MAPK, mitogen-activated protein kinase; MuRF-1, muscle RING finger protein-1; IGF-1, insulin-like growth factor-1; and MAFbx, muscle atrophy F-box protein 1 [1][24].
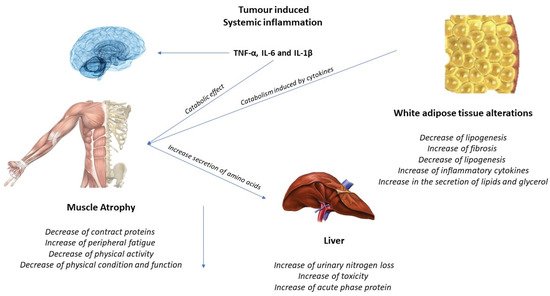
Figure 2. Tumor-induced systemic inflammation.
1.3. Effects of Exercise on the Muscle and Possible Mechanisms for the Treatment of Cachexia
Increased IL-6 may induce an anti-inflammatory effect, increasing IL-10 and IL-1ra and reducing TNF-alpha. A higher production of antioxidants than pro-oxidants may be responsible for the restoration of redox homeostasis during exercise. Increased activity of the PI3K/ALT/mTOR pathway and reduced activity of the ubiquitin proteasome and lysosomal autophagy pathways may induce protein homeostasis, increasing muscle synthesis and decreasing muscle degradation (Figure 3). PGC-1alpha activation can regulate genes involved in mitochondrial biogenesis and redox homeostasis (nuclear respiratory factors 1 and 2 and mitochondrial transcription factor A); increase GLUT-4 expression; regulate glucose metabolism; and decrease glucose metabolism, FOXO function, and proteolysis [6][7][29,30].
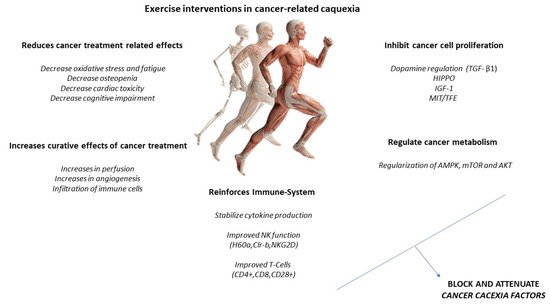
Figure 3.
Exercise intervention in cancer-related cachexia.
However, treatment and guidelines for patients with cachectic cancer have yet to be fully developed. Systemic alterations common to cancer remain viable therapeutic targets for both preventing and treating the cachectic state. Focusing on skeletal muscle maintenance has the potential to reduce systemic inflammation and improve patients’ metabolism and overall physical function. Along these lines, metabolic health and muscle mass are dramatically affected by physical activity and exercise. It is clear that physical activity and exercise are beneficial during cancer treatment and survivorship and have clear potential as a non-pharmacological treatment for muscle-wasting conditions. However, successful randomized controlled trials in patients with cachectic cancer on muscle mass, metabolism, and physical function are lacking. Further research is needed to determine the mechanistic basis for these improvements and whether these benefits can be achieved.
