Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Seong An and Version 2 by Catherine Yang.
Transthyretin (TTR) is a thyroid hormone-binding protein which transports thyroxine from the bloodstream to the brain. The structural stability of TTR in tetrameric form is crucial for maintaining its original functions in blood or cerebrospinal fluid (CSF). The altered structure of TTR due to genetic mutations or its deposits due to aggregation could cause several deadly diseases such as cardiomyopathy and neuropathy in autonomic, motor, and sensory systems.
- transthyretin
- mutation
1. Introduction
Transthyretin (TTR) protein was discovered incidentally from cerebrospinal fluid (CSF) in 1942 and was called prealbumin based on its observed electrophoretic pattern [1]. The name “transthyretin” was formulated from the combination of three words: transport, thyroxine and retinol. As the name implied, TTR is a carrier protein of thyroxine and retinol. The gene for TTR is located in chromosome 18 position 12.1 (18q11.2-12.1) or base pair 31,591,766 to 31,599,023 and consists of four exons and five introns [2].
2. Structural Overview: The Role of TTR
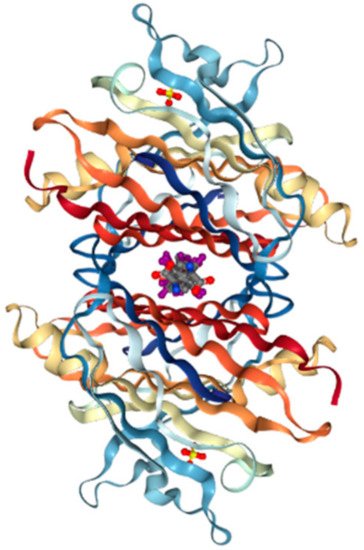
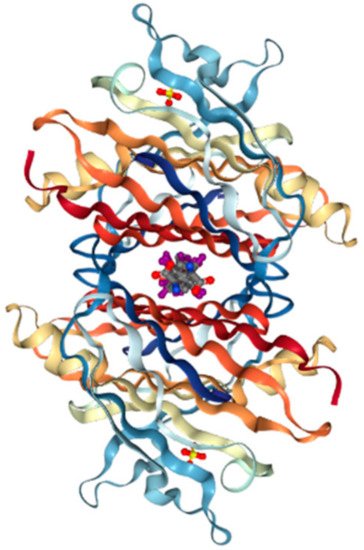
TTR has a molecular weight of 14 kDa in monomeric form and exists in tetrameric form (55 kDa) in plasma [3][13]. It is synthesized in the liver and choroid plexus as a homo-tetramer structure with a dimer of dimers quaternary structure. The amino acid sequence from 1 to 20 is the signal peptide, and the final protein structure is expressed from amino acids 21 to 147. Hence, each monomer consists of 127 amino acids with one alpha helix, called EF helix, and eight beta strands (Figure 1a) [4][5][14,15]. Hydrogen bonds primarily kept the monomer and dimer structures intact. The pairs of hydrogen bonds in D strands of the monomers contributed to structural stability by forming an internal convex-shaped channel (Figure 1b) [6][16]. The two dimers then gathered to form a homo-tetramer through additional hydrogen bonds, finalizing the assembly of the carrier protein [7][17].
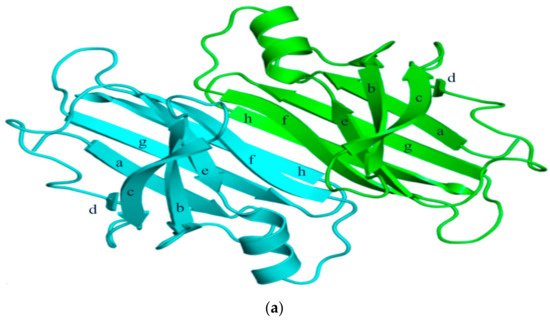
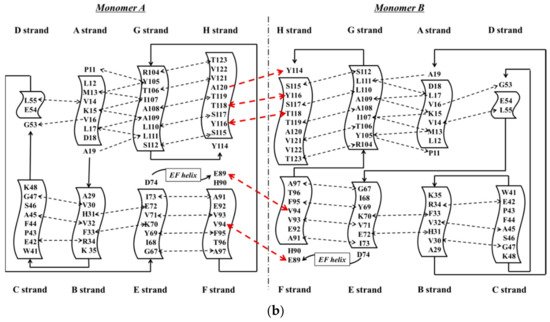
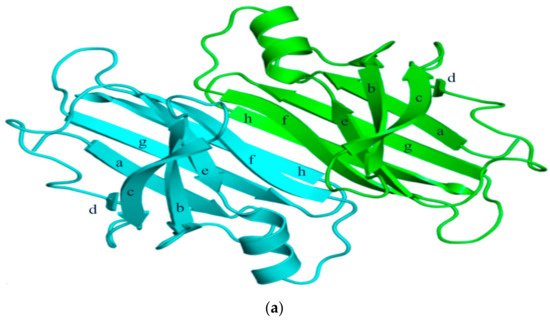
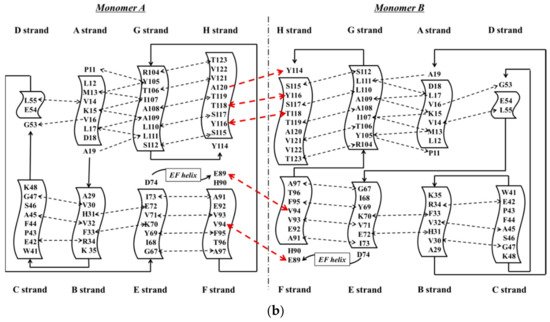
Figure 1. (a) 3-Dimensional structure of ATTRwt (PDBe ID code; 1BMZ [8][18]) in dimeric form; (b) Schematic diagram of hydrogen bonds in transthyretin and monomer–monomer’s hydrogen bonds. Arrowhead indicates acceptor, the tail indicates donor. In acidic condition, hydrogen bonds will be broken and destabilized.
Production of TTR by the liver or choroid plexus is followed by the translocation of the protein into the blood or CSF. The role of homo-tetrameric TTR is to transport T4 hormone and retinol. More than 99% of human T4 hormones are transported by carrier proteins, such as albumin, thyroxine-binding globulin, and TTR, and these same proteins are responsible for 15% of T4 hormone transports in circulation [9][19]. Homo-tetrameric TTR has two binding sites at a central channel called T4 pocket and is formed by side chain interactions [6][16]. Earlier reports of T4 binding studies predicted only one binding site, but investigation using a fluorescent probe, 8-anilinonapthalene-1-sulfonate, revealed two binding sites at opposite ends. Despite TTR having two T4 hormone-binding sites, the T4 hormone would preferentially bind to only one of the two sites. This preferential binding is influenced by relatively stronger binding affinity of one binding site and negative cooperativity, as well as structural changes of TTR, which can significantly reduce affinity at the other binding site [10][20]. Finally, the formation of hydrogen bonds between T4 hormone and Lys15 at the A strand/Glu54 at the D strand reinforced the hormone at the center of the tetramer (Figure 2) [11][21].
On the other hand, vitamin A (retinol) binds to TTR through a mediating protein, called retinol-binding protein (RBP) instead of the T4 binding protein. RBP (20 kDa) is synthesized by hepatocytes in the liver and consists of one alpha helix and eight anti-parallel beta-barrels [12][22]. Two RBPs bind and surround the TTR tetramer from both sides, but the limited concentration of RBP would result in a 1:1 molar ratio in plasma [13][23]. The amino acids of TTR interact with the following amino acids of RBP: Leu35, Trp67, Lys89, Trp91, Ser95, Phe96, Leu97 and Lys99 [14][24]. Retinol could not escape renal filtration through the urine once bound to the complex, TTR-RBP, thereby preserving retinol concentration as well as that of RBP [15][16][25,26]. The stability of the TTR-RBP-retinol complex is reduced when retinol is removed [17][27].
3. ATTR Causative Diseases
Mutations which are present in the TTR core structure reduce the stability of the protein. As a result, the TTR tetramer could separate into dimeric and monomeric forms, and these monomers coalesce by forming amyloid TTR (ATTR) aggregates (Figure 3) [18][28]. This aggregation, called amyloidogenesis, progresses to plaque formation, later depositing into tissues and neurons and inducing cytotoxicity. The different amyloidogenic diseases that present as a result were initially termed as the following: senile systemic amyloidosis (SSA), familial amyloid cardiomyopathy (FAC), and familial amyloid polyneuropathy (FAP) [18][19][28,29]. SSA, FAC, and FAP were reported to share the same accumulation of ATTR, but the types of ATTR found were different for each disease. In the case of SSA, aggregated constituents were composed mainly of large quantities of deposited wild-type ATTR (ATTRwt) in myocardia [20][21][30,31]. Updates in nomenclature were recently recommended by the International Society of Amyloidosis (ISA) to modify the terms SSA, FAC, and FAP to more exact definitions due to overlap in clinical presentation [22][32]. SSA was renamed as wild-type amyloid TTR amyloidosis (ATTRwt amyloidosis). It usually occurs in 25% of the elderly population over 80 with higher frequency in males at 25~50: 1 ratio [23][24][33,34]. Large amyloid deposits in the myocardia could cause congestive heart failure [25][35] and ventricular hypertrophy when echocardiography showed thickened ventricular walls along with low QRS voltages from electrocardiography (ECG) [26][36]. Common observable symptoms are fatigue, edema, shortness of breath, chest pain, and angina, and the severity of symptoms from these diseases may vary depending on the degree of ATTRwt deposits [27][28][29][37,38,39].
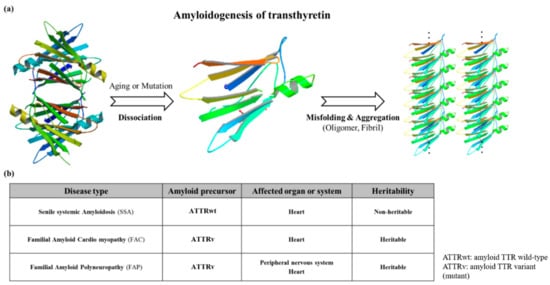
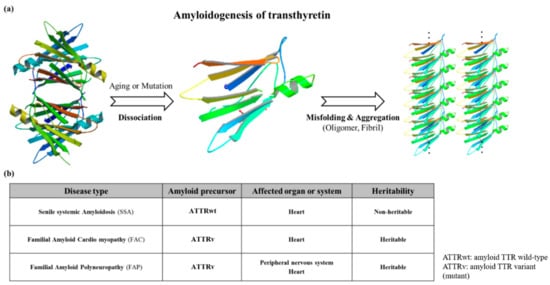
Figure 3. (a) Schematic diagram showing the amyloidogenesis of transthyretin. Transthyretin amyloidosis requires tetramer dissociation to monomer. (Transthyretin tetramer—PDB ID code; 4PVL83, Transthyretin monomer—PDB ID code; 3I9A84, Fibrils structure is made by ATTRv monomer without calculation); (b) Types of transthyretin amyloidoses.
FAC/FAP belong to the same pathological spectrum and differ from ATTRwt amyloidosis mainly due to ATTR mutations. In this case, ATTRv (amyloid TTR variant) refers to the mutant form of ATTR, and FAC/FAP was renamed to ATTR appended with the specific mutation that caused it (i.e., ATTRV30M) and the accompanying symptom (i.e. ATTR with cardiomyopathy) [22][32]. Depending on the mutations, the hydrophobic interaction of dimer–dimer formation would vary, resulting in the instability and breakdown of the tetramers. As a result, the tendency to produce the amyloid form is enhanced and favors the development of the disease [30][40]. FAP was formerly categorized into four types: FAP-I, FAP-II, FAP-III and FAP-IV, and the pathogenicity of FAP and FAC could overlap [31][32][33][41,42,43]. FAP-I has since been renamed as ATTRV30M amyloidosis and is also known as the Portuguese–Swedish–Japanese type, and haplotype comparison among foci suggested common Portuguese origins among Japanese, Spanish, and Brazilian patients, while Swedish patients had entirely different haplotypic origins [34][35][44,45]. ATTRV30M amyloidosis resulted in a wide range of symptoms such as sensory-autonomic, gastrointestinal and cardiac disturbances, impotence, and cardiomyopathy; as well as renal insufficiency in later stages of the disease [36][37][46,47]. A study on 15 Swedish families with ATTRV30M determined through Western blot showed the type of amyloid fibril composition remained the same despite the differences of the disease age of onset. Only one family showed different types of amyloid fibril composition on two brothers with similar ages of disease onset [38][48]. Despite the endemicity of the early onset form of ATTRV30M in some Portuguese, Japanese, and Swedish populations, the late onset form was shown to be more prevalent in non-endemic areas of Japan and Cyprus than previously thought, and much is still not known about its causative factors [39][40][49,50]. Symptoms of ATTRI84S amyloidosis were similar to ATTRV30M amyloidosis, but additional sensorimotor polyneuropathy could appear late in the disease [41][55]. In addition, amyloid deposits could be found in the eye, thyroid, adrenal glands, and blood vessels, leading to additional side effects from both diseases [42][43][44][45][56,57,58,59]. Even though ATTRv amyloidosis was like ATTRwt amyloidosis in terms of disease pathomechanism, the expression of ATTRv outside cardiac tissue may lead to amyloidosis resulting in hereditary ATTR cardiomyopathy (ATTR-CM). This was described in a Danish family carrying ATTRMet111 expressed in plasma that led to hereditary ATTR-CM (previously known as familial amyloid cardiomyopathy or FAC), whereas unafflicted members were seronegative [46][60]. Patients beyond the age of 60 were reported to have hereditary ATTR-CM, and ATTRV122I and ATTRT60A could be responsible. ATTRV122I was most commonly found in 4% of African-Americans, followed by ATTRT60A in patients from United Kingdom and Ireland [47][48][49][61,62,63]. The role of the non-coding variation of ATTRV122I was assessed in 4,361 unrelated African-Americans. The study showed that this allele increased 6.8-fold the risk of having ten or more outpatient surgeries. Additionally, men had a 15.2-fold higher risk of having ten or more outpatient surgeries. This non-coding variation seemed to accelerate the negative consequences associated with ATTRV122I amyloidosis [50][64]. Amyloid deposits in cardiac tissues may cause a thickening of cardiac walls leading to congestive heart failure and atrial arrhythmias, and result in cardiac arrest and death [45][51][59,65]. Carpal tunnel syndrome may manifest in the early phase of ATTRv amyloidosis and may require a great deal of attention and not simply dismissed as an unrelated symptom [52][66]. More than 140 ATTRv mutations have been identified [53][3] along with non-amyloidogenic mutations (Figure 4), which may not produce amyloid, but were reported to cause functional abnormalities in vivo [54][55][67,68]. Among non-amyloidogenic mutations, few were revealed to have a high affinity for thyroxine [54][67], and rarely, alanine mutations, particularly A109T and A109V, which were described in a family with dominantly-inherited euthyroid hyperthyroxinemia [56][69].
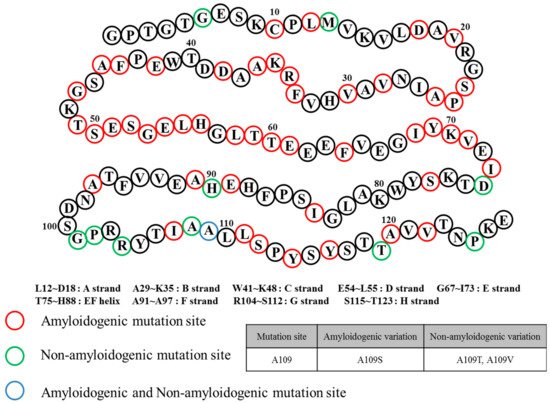
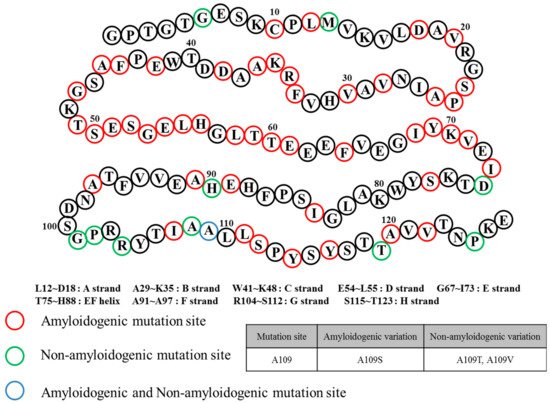
Figure 4.
Transthyretin mutation sites and relation to amyloidosis.
4. General Diagnostic Workflow for ATTR Causative Diseases
Upon initial detection of the clinical symptoms mentioned above, additional diagnoses are still required to discern ATTR disease types for prompt treatment. ECG, magnetic resonance imaging (MRI), echocardiography, tissue biopsy, and genetic analysis could be performed for wild-type and hereditary ATTR amyloidoses. ECG is prioritized if the detected symptoms are primarily observed in the heart. In recent years, many kinds of ECG analysis were reported to lead to better initial diagnosis. As an example, left bundle branch block can differentiate ATTRwt amyloidosis from primary light chain amyloidosis (AL) as this ECG pattern can be observed in 40% of ATTRwt patients but is rare (4%) in AL [57][70]. Notably, low QRS voltages were observed in 60% of AL patients but were not as frequent in ATTRwt patients (40%) [57][58][70,71]. An abnormal ECG result would call for MRI using gadolinium enhancement by visualizing amyloid deposition in cardiac tissue for a more accurate diagnosis [59][72]. Echocardiography was used for diagnosing hypoplasia in the left and right ventricles of neonates [60][73] and has also been considered as an invaluable tool in providing real time and rapid evaluation of ventricular function in neonates and children with suspected ventricular anomalies [61][74]. This is largely in part due to its noninvasive nature and absence of side effects during right ventricular evaluation [62][75] which consists of assessment of ventricular atrophy based on ventricular muscle thickness [63][76]. Echocardiography also proved to be equally valuable in the assessment of left ventricular function through the measurement of different parametric velocities of the ventricular wall [64][77]. More recently, global longitudinal strain (GLS) measurement through speckle-tracking analysis of 2D-echocardiography was demonstrated to be a feasible non-invasive and more accurate alternative to the more traditional left ventricular ejection fraction (LVEF) [65][78]. Tissue biopsy could more accurately differentiate whether the disease was due to wild-type or variant-type ATTR deposits compared to simple visualization. If ATTR amyloidosis was suspected following MRI or 2D-echocardiography, tissue should be collected from the appropriate site depending on the patient’s condition, such as the heart tissue and sural nerve [66][79]. Each tissue was analyzed for ATTR types through amyloid fibril analysis using Congo red, immunohistochemistry, and mass spectrometry [67][68][69][80,81,82]. Despite its accuracy, acquiring tissue samples internally through biopsy is an invasive procedure when compared to ECG and 2D-echo, thus other more easily accessible organ sources were considered. Not too recently, skin biopsy was shown to be a promising alternative to the otherwise more invasive method of acquiring internal tissues from the heart or sural nerve in ATTRv (FAP) diagnosis [70][83]. Intraepidermal, sweat gland, and pilomotor nerve fiber densities were measured and compared in ATTRv patients, asymptomatic ATTRv carriers, healthy controls, diabetic neuropathy disease controls, and AL patients [70][83]. Immunohistochemistry revealed decreased fiber densities from all three tissue sources in ATTRv patients compared to normal controls, while ATTRv carriers showed intermediate reductions. The sensitivity and specificity for ATTRv diagnosis through detecting amyloid in skin was calculated to be 70% and 100%, respectively [70][83]. Additional genetic analyses using blood can be done to determine the type of disease. ATTR variants were identified by PCR-based full sequence analysis with 99% accuracy [71][72][84,85]. From these methods, patients with ATTRV112I were diagnosed as ATTR-CM (FAC at the time) [49][63], and the ATTRV30M variant could suggest amyloid deposition in the cardiac muscle or nerve [73][86]. If no mutation was found, the patient would be diagnosed with ATTRwt amyloidosis [20][30].
