The accuracy of nucleic acid amplification tests is highly dependent on the time of obtaining the sample, as well as the type, storage, and handling of the sample. These tests can only diagnose active infections. False-negative results can occur if the sample is not obtained appropriately or if the subject is tested too soon or too late after exposure to the virus. In addition, the tests are complex and require specialized laboratory equipment and reagents, as well as specialists to perform the tests, which can be problematic due to the prolonged time required for obtaining the results.
Many researchers have attempted to overcome the limitations of reverse transcription polymerase chain reaction (RT-PCR) assays
[34][35][36][37][35,36,37,38]. Antibody detection assays present several advantages over RT-PCR. Antibodies are more stable than RNA and are less degradable during transport and storage, thus reducing the risk of false-negative results. Although the research on antibody-based tests is ongoing, there are limitations to overcome. The main reason for this is the lack of specificity. Additionally, there is a lag phase from the initial virus exposure to the antibody response against infection. According to the accumulated immunological data, the antibody response peaks at approximately 11 days, indicating an insufficient time period for preventing the rapid spread of infectious diseases at early stages of infection. Therefore, antibody detection assays are less effective in diagnosing emerging and re-emerging viral diseases.
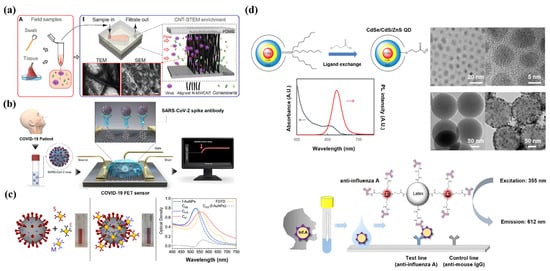
There is a need to develop new diagnostic platforms that are accurate, specific, fast, and easy to use, to facilitate rapid screening. Currently, research dynamics have shifted towards rapid diagnostics based on nanomaterials
[38][39][40][41][39,40,41,42]. In this regard, nanotechnology-based applications can greatly improve the sensitivity of previously developed detection techniques, such as RT-PCR and immunoassays. Nanoparticles (NPs) have the characteristics of high adsorption capacity, the quantum size effect, and high reactivity. The large surface area of NPs can enhance detection effectiveness, as it allows efficient interaction with target analytes. Therefore, through physical or chemical bonding, nanomaterial-based diagnosis can be developed to increase selectivity and specificity and reduce detection time. Appropriately using advanced nanomaterials is the key to achieving improvements in nanotechnology. Nanomaterials are the basis for the design of a wide range of virus diagnostic tools. The unique characteristics of nanomaterials make them suitable for application in state-of-the-art virus detection technologies.
3. NP Vaccines for Emerging Viruses
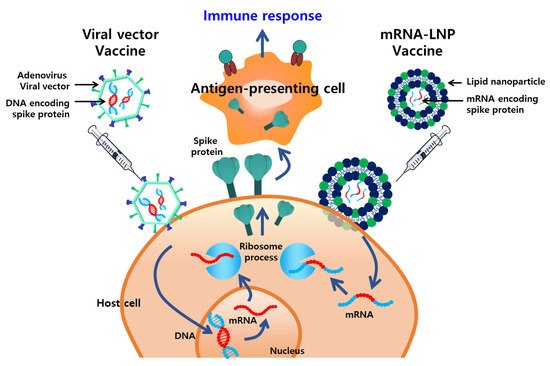
Vaccines are the most effective and cost-efficient means for preventing infectious diseases. Despite the significant successes of various vaccines, the ongoing development of new, safer, and more potent vaccines is required because of the emergence of new pathogens, recurrence of old pathogens, and mutations in existing pathogens. Typically, vaccines incorporate adjuvants, which are supplementary substances that compensate for the poor immunogenicity of antigens and enhance the cellular and humoral immunity. Several nanoplatforms that improve vaccine immunogenicity by enhancing the delivery of antigens to the immune system or via a depot effect have been developed. The WHO Emergency Use Listing for combating the COVID-19 pandemic includes vaccines that incorporate a delivery system based on NPs, such as lipid NPs (LNPs) (Moderna, MA, US and Pfizer-BioNTech, NY, US) and adenovirus viral vectors (Janssen, NJ, US and AstraZeneca, UK) (
Figure 2).
Figure 2. Overview of nanoplatform-based vaccines approved by the World Health Organization (WHO) for the prevention of emerging infectious diseases. Viral vectors and lipid NPs (LNPs) elicit potent immune responses by stably delivering DNA and mRNA encoding antigens, respectively, to antigen-presenting cells.
Delivery systems formulated with NPs are being used in next-generation vaccines for effectively delivering antigens and/or intrinsic immunostimulants
[42][43][44][45][46][93,94,95,96,97]. These vaccines are being engineered not only for the prevention of emerging infectious diseases, but also for treating chronic diseases, such as diseases caused by hepatitis C infections
[47][48][98,99], human immunodeficiency virus (HIV) infections
[49][50][100,101], herpes
[51][102], and cancer. Next-generation vaccines aim to induce both humoral and cellular immune responses, while being applied prophylactically and therapeutically
[52][53][103,104]. Various nanoplatforms have been incorporated into delivery systems and immunogenicity-enhancing strategies, such as LNPs, polymeric NPs, nano-complexes, virus-like particles, and inorganic NPs. The main principle of delivery systems is to deliver the vaccine antigens or immunopotentiators to the antigen-presenting cells (APCs; including macrophages and dendritic cells) responsible for the induction of innate immune responses. A delivery system that is similar in size to nano-sized pathogens is expected to be advantageous for APC phagocytosis and for presenting antigens to naïve T cells in lymphoid tissues. Further, nanoparticulate delivery agents can protect the payload, deliver it in an intact native conformation to a target site within the immune system, and create a sustained release of antigens over time. In the future, the usage of such next-generation nano-delivery systems in vaccine technology is expected continue with sufficient safety and stability. Herein, we discuss the use of several representative nanoplatforms (LNPs and polymer particles) in delivery systems that enhance vaccine efficacy. We also review nanotechnology-based adjuvants that enhance the intensity and quality of cellular and humoral immune responses for the development of vaccines.
4. Treatment
The development of effective antiviral agents is essential for treating or alleviating severe symptoms and preventing death in infected patients. Timely antiviral therapy is an important measure to reduce the burden on the health care system. A variety of synthetic and natural antiviral agents have been developed, including chemical compounds, peptides, and essential oils. These agents exhibit antiviral activity against various types of viruses
[54][139]. Other FDA-approved therapeutics, such as oseltamivir, zanamivir, and abacavir, are being utilized in antiviral therapy for influenza and HIV infection
[55][140]. Remdesivir is now being used for the treatment of COVID-19, and its usage is associated with a significant reduction in the mortality of infected patients
[56][141]. Despite the contributions of antiviral agents, there are several challenges associated with their usage, such as limited efficacy because of poor solubility, low biostability, and toxicity. Additionally, improvements can be made regarding the therapeutic effects of antiviral agents, which mostly block viral proteins and cellular receptors involved in viral infection pathways, such as site-specific delivery of antiviral agents to enhance efficacy and reduce off-target effects. Thus, there is a need for efficient delivery of antiviral agents
[57][142].