Intersphincteric resection is an anus-preserving technique for low rectal cancers described by Schiessel et al. in 1994 as a combination of two techniques: the intersphincteric rectal excision for inflammatory bowel disease and the coloanal anastomosis for low rectal resections.
- advanced rectal cancer
- intersphincteric resection
- minimally invasive surgery
- anus-preserving surgery
- laparoscopic surgery
- robotic surgery
- local recurrence
- anorectal function
- low rectal cancer
- abdominoperineal resection
1. Intersphincteric resection (ISR)
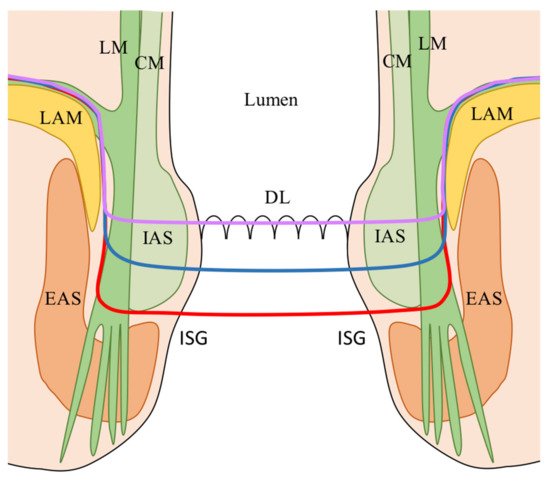
Intersphincteric resection (ISR) is characterized by two distinct phases: abdominal and perineal. ISR allows extension of the caudal dissection plane to allow a safe distal margin for very low-lying rectal cancer without excising the sphincter complex (external anal sphincter (EAS)/levator ani muscle (LAM)) as in the abdominoperineal resection. The oncological safety of the ISR derives from the knowledge that lymphatic spread of low rectal cancers occurs especially in the oral direction within the mesorectum with local spread present only in few millimeters [39,40].
2. Indication of ISR
|
Authors, year |
| Authors, Year |
|---|
Indications |
| Indications |
|---|
Contraindications |
| Contraindications |
|---|
|
Schiessel, 1994-2012 [18,19,39] |
- T1-T3 LRC - Tumor diameter >1 cm - Big villous adenomas - Mucosectomy/RT residual tumors - Low carcinoids/hemangiomas |
- Undifferentiated tumors - EAS infiltration - T4 stage - Preop. insufficient sphincter fx - Distant metastases |
|
Vorobiev, 2004 [58] |
- T2-3 (EUS) - Well/moderately diff. adenoca. - Fecal continence |
- EAS/LAM infiltration - N+ (EUS) - M+ |
|
Rullier, 2005 [45] |
- ≤ 4.5 cm AV - Distant metastases |
- EAS/LAM infiltration - Fixed tumors (except partial vaginal fixity) - Fecal incontinence >6 months before diagnosis |
|
Hohenberger, 2005 [46] |
- ≥0.5 cm from DL (rectoscopy) - T1-2 (EUS) - T3 (above puborectal sling) - G1-2 - Patients with possibly distinct invasion of the pelvic floor musculature underwent prior nCRT |
- EAS infiltration - Fecal incontinence |
|
Chin, 2006 [47] |
- T2 - T3-4 (after nCRT) - ≤ 5 cm (maximal diameter) - 1-3 cm from DL |
- Distant metastases |
|
Chamlou, 2007 [48] |
- T1-3 - T4 if invasion is distant from the tumor’s lowest part/sphincter, and is resectable - Resectable distant metastases - uT1 with adverse pathologic features after transanal local excision |
- EAS/LAM infiltration - Fecal incontinence |
|
Krand, 2009 [59] |
- (Study on ISR with partial IAS) - Distal excision at the DL or 1-2 mm distal to it - T2-3 - Well/moderately diff. adenoca. |
- Total IAS for achieving acceptable DRM - Fecal incontinence - EAS/LAM infiltration - Poorly diff. adenoca. - Distant metastases (except resectable liver metastases) |
|
Han, 2009 [60] |
- T1-2 (IAS) - T1-T2 after nCRT - Tumor diameter >1 cm but <5 cm - Well/moderately diff. adenoca. - Sufficient anal fx (DRE, manometry) |
- Infiltration of pelvic floor - Tumor diameter >5 cm - Poorly diff. adenoca. - Insufficient anal fx (DRE, manometry) - Distant metastases - Intestinal obstruction |
|
Kuo, 2011 [62] |
- T1-3 |
- Infiltration EAS/LAR (even if submitted to nCRT with radiological clearance) |
|
Martin, 2012 [69] (Review) |
- ≤1 cm from anorectal ring |
- T4 tumors - EAS/LAM infiltration - Fixed tumors at DRE - Poorly diff. adenoca. - Fecal incontinence - Distant metastases |
|
Tokoro, 2013 [52] |
- T1-3 - Resectable metastases |
- T4 tumors - Poorly diff. adenoca. - Infiltrating gross appearance - Fecal incontinence |
|
Akagi, 2013 [53] |
- T1-3 (mobile tumors) - ≤4 cm from AV - Well/moderately diff. adenoca. - ECOG PS 0-2 - Good anal function |
- T4 tumor - Fixed tumors - Untreatable distant metastases - Poorly diff. adenoca. - Psychiatric disease - Poor anal function (no discernable tone at DRE or the maximum squeeze pressure <50 mmHg before operation) - Liver cirrhosis, renal dysfunction, cardiac failure, and respiratory dysfunction |
|
Akagi, 2013 [41] (Review) |
- T1-3 tumors - 30-35 mm from AV - Independently to IAS invasion |
- As for Schiessel et al. |
|
Saito, 2014 [64] |
- T1-4 - ≤5 cm from AV |
- EAS/LAM infiltration - Fecal incontinence |
|
Shirouzu, 2017 [70] (Review)
|
- T1-3 - 1-5 cm AV - Well-moderately diff. adenoca. |
- T4 - Fixed tumors - EAS/LAM infiltration - Untreatable distant metastases - Poorly diff. adenoca. - Poor anal fx - Severe preoperative pathologies (cardiac failure, liver cirrhosis, renal dysfunction, respiratory dysfunction) - Psychiatric disease |
|
Park, 2019 [56] |
- Tumor’s response to nCRT on restaging MRI - Evaluation of ymrT stage and ymrCRM status |
- Poor nCRT responders |
|
Piozzi, 2021 [57] |
- ≤4 cm from AV - After nCRT for cT3-T4 - (y)cT4 if curative resection is technically feasible at the pre-operative MRI - Conversion from an ultra-low AR in case of involvement/threatening of the distal gross margin in the resected specimen or in case of stapler failure for any reason |
- EAS/LAM infiltration (at restaging MRI after nCRT) - Abundant mucinous component - Anal canal involvement below DL (requiring total ISR) - Fecal incontinence - Patient's refusal |
| Schiessel, 1994–2012 [18,19,39] | -T1–T3 LRC -Tumor diameter >1 cm -Big villous adenomas -Mucosectomy/RT residual tumors -Low carcinoids/hemangiomas |
-Undifferentiated tumors -EAS infiltration -T4 stage -Preoperative insufficient sphincter function -Distant metastases |
| Vorobiev, 2004 [58] | T2–3 (EUS) Well/moderately diff. adenoca. Fecal continence |
-EAS/LAM infiltration -N+ (EUS) -M+ |
| Rullier, 2005 [45] | -≤4.5 cm AV -Distant metastases |
-EAS/LAM infiltration -Fixed tumors (except partial vaginal fixity) -Fecal incontinence > 6 months before diagnosis |
| Hohenberger, 2005 [46] | -≥0.5 cm from DL (rectoscopy) -T1–2 (EUS) -T3 (above puborectal sling) -G1–2 -Patients with possibly distinct invasion of the pelvic floor musculature underwent prior nCRT |
-EAS infiltration -Fecal incontinence |
| Chin, 2006 [47] | -T2 -T3–4 (after nCRT) -≤5 cm (maximal diameter) -1–3 cm from DL |
-Distant metastases |
| Chamlou, 2007 [48] | -T1–3 -T4 if invasion is distant from the tumor’s lowest part/sphincter, and is resectable -Resectable distant metastases -uT1 with adverse pathologic features after transanal local excision |
-EAS/LAM infiltration -Fecal incontinence |
| Krand, 2009 [59] | -(Study on ISR with partial IAS) -Distal excision at the DL or 1–2 mm distal to it -T2–3 -Well/moderately diff. adenoca. |
-Total IAS for achieving acceptable DRM -Fecal incontinence -EAS/LAM infiltration -Poorly diff. adenoca. -Distant metastases (except resectable liver metastases) |
| Han, 2009 [60] | -T1–2 (IAS) -T1-T2 after nCRT -Tumor diameter > 1 cm but <5 cm -Well/moderately diff. adenoca. -Sufficient anal function (DRE, manometry) |
-Infiltration of pelvic floor -Tumor diameter > 5 cm -Poorly diff. adenoca. -Insufficient anal function (DRE, manometry) -Distant metastases -Intestinal obstruction |
| Kuo, 2011 [62] | -T1–3 | -Infiltration EAS/LAR (even if submitted to nCRT with radiological clearance) |
| Martin, 2012 [69] (Review) | -≤1 cm from anorectal ring | -T4 tumors -EAS/LAM infiltration -Fixed tumors at DRE -Poorly diff. adenoca. -Fecal incontinence -Distant metastases |
| Tokoro, 2013 [52] | -T1–3 -Resectable metastases |
-T4 tumors -Poorly diff. adenoca. -Infiltrating gross appearance -Fecal incontinence |
| Akagi, 2013 [53] | -T1–3 (mobile tumors) -≤4 cm from AV -Well/moderately diff. adenoca. -ECOG PS 0–2 -Good anal function |
-T4 tumor -Fixed tumors -Untreatable distant metastases -Poorly diff. adenoca. -Psychiatric disease -Poor anal function (no discernable tone at DRE or the maximum squeeze pressure < 50 mmHg before operation) -Liver cirrhosis, renal dysfunction, cardiac failure, and respiratory dysfunction |
| Akagi, 2013 [41] (Review) | -T1–3 tumors -30–35 mm from AV -Independently to IAS invasion |
-As for Schiessel et al. |
| Saito, 2014 [64] | -T1–4 -≤5 cm from AV |
-EAS/LAM infiltration -Fecal incontinence |
| Shirouzu, 2017 [70] (Review) |
-T1–3 -1–5 cm AV -Well-moderately diff. adenoca. |
-T4 -Fixed tumors -EAS/LAM infiltration -Untreatable distant metastases -Poorly diff. adenoca. -Poor anal function -Severe preoperative pathologies (cardiac failure, liver cirrhosis, renal dysfunction, respiratory dysfunction) -Psychiatric disease |
| Park, 2019 [56] | -Tumor’s response to nCRT on restaging MRI -Evaluation of ymrT stage and ymrCRM status |
-Poor nCRT responders |
| Piozzi, 2021 [57] | -≤4 cm from AV -After nCRT for cT3-T4 -(y)cT4 if curative resection is technically feasible at the pre-operative MRI -Conversion from an ultra-low AR in case of involvement/threatening of the distal gross margin in the resected specimen or in case of stapler failure for any reason |
-EAS/LAM infiltration (at restaging MRI after nCRT) -Abundant mucinous component -Anal canal involvement below DL (requiring total ISR) -Fecal incontinence -Patient’s refusal |
