2.2.1. TACE
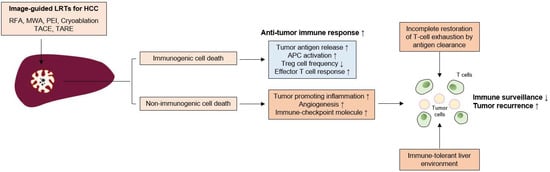
TACE is the preferred method for treating intermediate-stage, unresectable HCCs. Despite procedural advancement, the clinical outcome has not been satisfactory and the median OS, which is affected by tumor size, tumor markers, liver function, and vascular invasion, was 19.9 months based on a recent report
[37][84]. Similar to local ablative treatments, immune dysfunction may remain even after successful treatment. Furthermore, in a previous study with human samples, PD-1
+-exhausted CD8
+ T cells in the tumor were more increased in stage II or III patients than in stage I patients
[16][64], indicating that T-cell exhaustion is more advanced in patients receiving TACE than in patients receiving local ablation treatments. As TACE is not a curative treatment and a small number of tumor cells can remain in circulation and within the liver, surveillance and clearance by immune cells and their augmentation using ICBs could have clinical benefit
[38][13] and clinical trials are ongoing.
The changes in the composition or function of immune cells after TACE remain to be elucidated, and whether the peripheral T cell population might be affected by TACE has been investigated in only a few studies. Growing evidence indicates that tumor necrosis caused by TACE induces immunological activation. For example, the inflammatory cytokine IL-6 significantly increased early after TACE
[39][85]. However, Th2 cytokines (IL-4, IL-5, or suppressive cytokine IL-10) were also increased in the late phase after TACE, indicating that the immunological changes caused by TACE are complicated processes.
Immunologic cell death markers, such as high mobility group box 1 (HMGB1) and soluble receptor for advanced glycation end products (sRAGE), inducers of PD-L1 in tumor cells, are increased by TACE in HCC patients
[40][41][86,87]. In a previous report, the peripheral CD4
+/CD8
+ T cell ratio was significantly lower in patients with HCC prior to TACE than in healthy volunteers and was increased 1 month after TACE
[42][43][88,89], although its effect on anti-tumor immunity was not investigated in those studies. However, in another study, TACE increased the frequency of tumor-specific CD4
+ T cells, which was associated with improved clinical outcomes
[44][90]. Notably, a recent report showed that baseline PD-L1 expression within peripheral blood mononuclear cells was significantly higher in poor TACE responders, which were defined as SD or PD by RECIST criteria, and patients with high PD-L1 expression of PBMCs after TACE showed poor OS
[45][91]. Additionally, TACE increases PD-1 expression in peripheral mononuclear cells
[45][91]. These findings indicate that targeting the PD-1-PD-L1 axis might benefit the clinical outcome after TACE in terms of response rate and survival, although the effects of PD-1 expression on anti-tumor immunity before and after TACE remain unclear.
Several studies have indicated that TACE also affects Treg cells. Peripheral Treg cells were significantly increased in HCC patients and decreased by TACE
[42][46][88,92]; their reduction was associated with improved clinical outcomes
[47][93]. Among Treg cells, the effector Treg population, which exerts suppressive function, was also decreased by TACE, and post-TACE frequency in this population was associated with clinical outcome
[46][92]. As Treg cells also highly express PD-1 in HCC patients
[48][94], ICBs including PD-1 or CTLA-4 inhibitors might also be beneficial for HCC patients following TACE via further Treg reduction. Taken together, partial immune reconstitution due to TACE can occur, and targeting immune checkpoint molecules and immune-suppressive components, including Treg cells, would further augment anti-tumor immune responses and tumor surveillance even after successful TACE.
2.2.2. Transarterial Radioembolization (TARE)
Transarterial radioembolization (TARE) using yttrium-90 (Y90) is an emerging option for treating locally advanced HCC that is not eligible for surgical resection. The method delivers Y90 via tumor-supplying arteries and provides tumor-restricting effects without damaging the non-malignant liver
[49][95], although its long-term clinical outcome has yet to be determined. Similar to TACE, TARE also activates pro-inflammatory cytokines such as IL-6 and IL-8
[50][96], and baseline values of these cytokines are associated with liver function and survival
[51][97].
A recent in-depth analysis using CyTOF in resected HCC samples who underwent TARE before resection showed that TARE induces the activation of local immune cells, including CD8
+ T cells, CD56
+ NK cells, and CD8
+CD56
+ NKT cells
[52][98]. Notably, TARE also induces peripheral T-cell function and increases APCs
[52][98]. Furthermore, PD-1
+TIM-3
+CD8
+ T cells were observed in TARE responders, indicating that further enhancement of T cell responses might be feasible by using ICBs following TARE.