Melanomas of the skin are poorly circumscribed lesions, very frequently asymptomatic but unfortunately with a continuous growing incidence. In this landscape, one can distinguish melanomas originating in the mucous membranes and located in areas not exposed to the sun, namely the vulvo-vaginal melanomas. By contrast with cutaneous melanomas, the incidence of these types of melanomas is constant, being diagnosed in females in their late sixties. While hairy skin and glabrous skin melanomas of the vulva account for 5% of all cancers located in the vulva, melanomas of the vagina and urethra are particularly rare conditions. The location in areas less accessible to periodic inspection determines their diagnosis in advanced stages, often metastatic.
- vulvar melanoma
- vaginal melanoma
- targeted therapy
- gynecological cancer
- melanoma treatment
1. Introduction
2. Risk Factors
Melanoma, like most neoplastic pathologies, is a multifactorial disease, its occurrence being related to interactions between environmental and host factors, thus appearing as a consequence of genetic and epigenetic modifications that eventually lead to alteration of regulatory processes [23][27]. Although a number of risk factors involved in the etiopathogenesis of the disease have been identified for cutaneous melanoma, such as intermittent exposure with increased intensity to ultraviolet (UV) radiation, history of sunburns (more common at high latitudes), the presence of atypical nevi, specific skin phenotype (lightly pigmented skin, with light eyes, blond or reddish hair, presence of freckles), family history with specific genetic changes that alter the ultraviolets repair of melanocytes subjected to UV radiation, the use of Psoralen and Ultraviolet A therapy (PUVA) for a long time (over 15 years after exposure), the etiopathogenic mechanisms for vulvar and vaginal melanomas are not yet elucidated, and no specific factors involved in their occurrence have been identified [17][24][25][26][27][28][17,28,29,30,31,32]. Moreover, in a study published by Heinzelmann-Schwartzet et al., the onset of vulvar melanoma was regarded as spontaneous, de novo, with changes in a single melanocyte cell being enough to trigger the process of oncogenesis and determine the formation of melanoma [17]. However, there are studies that show a greater association between mucosal melanomas in general, and vaginal and vulvar melanomas in particular, and certain factors: Sex. The female gender appears to be a risk factor for mucosal melanomas in general, which are twice as common as in men, compared to cutaneous melanomas whose distribution is similar between the two sexes [29][33]. Age. Vulvar melanoma is a disease that has an average age of onset of 68 years old, the risk of onset increasing with age (the number of cases increases from 0.11/1 million inhabitants for 15–29 years range, to 3.5/1 million inhabitants for those over 60 years old [30][31][34,35]). In contrast, cutaneous melanoma has a maximum incidence around the fourth decade of life [31][35]. Family history of cutaneous melanoma appears to be a risk factor for vulvar melanoma [32][36]. Ethnicity also seems to play an important role in the evolution of melanomas with genital localization and in their prognosis. Even if the association is not as strong as in the case of cutaneous melanomas, vulvar and vaginal melanomas are three times more common in the white race (p < 0.001) [22]. However, the prognosis has an inverse association, the mortality being much higher among the African population [33][37]. Lichen sclerosus is a precursor lesion of squamous cell carcinoma of the genital area which appears in its evolution in a percentage of approximately 5%, the causal link between the two pathologies being well known. Regarding the occurrence of vulvar melanoma in patients with lichen sclerosus, while a causal link has not been clearly established, although the number of reported cases is quite small, an increased incidence of vulvar melanoma has been observed among these patients (relative risk = 341) [34][35][38,39]. UV radiation. Though vulvar melanoma does not occur in photo-exposed areas, some studies suggest the indirect involvement of UV radiation in the pathogenesis of vulvar melanoma, through alterations of the immune response that favor modifications of the pathways involved in oncogenesis. However, it is important to note that the role of radiation in the pathogenesis of the disease is significantly lower than in skin melanoma [30][34]. Although the Human Papilloma Virus (HPV) is known for its roles in the development of benign (condyloma acuminata) and malignant tumors (invasive squamous cell carcinoma, anorectal cancers, penile cancers, squamous vaginal cancers) with genital localization, there is yet no mechanism to demonstrate its involvement in melanoma. There is no evidence that the HPV infection elevates the risk of vulvar or vaginal melanomas [28][36][37][38][32,40,41,42].3. Clinical Manifestations
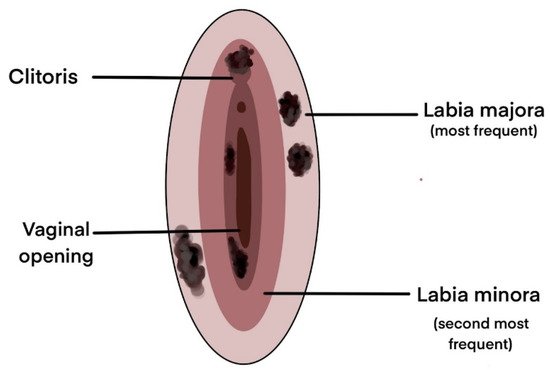
Unlike cutaneous melanoma which is most frequently distributed on photo-exposed areas (face, trunk, lower limbs) making it possible to diagnose it from early stages, vulvar and vaginal melanomas have origins that are generally overlooked by frequent inspection, the anatomical position of the lesion being the main reason for its late diagnosis and poor prognosis [39][43]. Melanomas of the vulvar region can occur in a variety of sites starting from the hairy skin of the labium majus to the introitus (Figure 1). The most common sites are the clitoris, the labia majora, and the labia minora, and in most cases, multiple tumors can be detected [30][40][41][34,44,45]. Vulvar and vaginal melanomas are pigmented lesions with variable diameters (generally over 7 mm), with macular (most frequently), papular or nodular appearance, most often asymmetrical and with an inhomogeneous appearance in terms of pigmentation [40][42][43][44,46,47]. There are also reports in the literature of cases with amelanotic manifestations of genital melanomas, especially at the vaginal level [20][44][20,48]. The first case of genital melanoma was described in 1861 in a 35-year-old patient who presented with multiple pigmentary lesions and evolved with neurological and digestive symptoms in the context of multiple secondary determinations and, subsequently, exitus [45][49]. Since then, multiple cases of vulvar and vaginal melanomas with various clinical, dermatoscopic aspects, and symptoms have been depicted in the literature (for additional details see [16][20][16,20]). As it is a rare pathology, most of the clinical data presented in the literature are obtained from isolated case presentations or case series, most of which highlight the presence of genital bleeding, a palpable, white-gray color mass, itching, dyspareunia, yellow genital secretions, and local pain [46][47][48][49][50][50,51,52,53,54]. Cases that mention the presence of painless masses are also reported [51][55]. Most of the cases presented depict the tumor in the labia minora. The diagnosis is generally late, with half of the patients being diagnosed in advanced stages, with the invasion of deep structures [52][56]. Although not so numerous and generally on small patient samples, there are prospective or retrospective clinical studies and meta-analyses that have highlighted the main clinical manifestations and the most common sites of vulvar and vaginal melanomas, which are further illustrated in Table 1.| Number of Patients |
Tumor Localisation | Main Signs and Symptoms |
Others Signs and Symptoms |
References |
|---|---|---|---|---|
| 51 | Labia minora | Pain, Palpable mass, Genital bleeding, Pruritus | Dysuria, Ulceration | [53][57] |
| 20 | Labia majora | Genital bleeding, Pruritus, Palpable mass | Pain, Dysuria, Unhealing sore, Urinary difficulties | [32][36] |
| 10 | Labia majora | Pruritus | - | [43][47] |
| 11 | Not specified | Pruritus, Pain, Genital bleeding | - | [56][26] |
| 14 | Labia minora | Pruritus | - | [54][58] |
| 31 | Vagina | Genital bleeding, Pain, Palpable mass | Abnormal vaginal secretion, Urinary difficulties | [55][59] |
| 33 | Not specified | Palpable mass, Genital bleeding, Pain, Pruritus | Abnormal vaginal secretion, Dysuria, Dyspareunia, Ulceration | [57][60] |
| 198 | Unilateral, Clitoris | Genital bleeding, Pain, Pruritus | - | [15] |