Coronavirus disease 2019 (COVID-19) is caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which appeared in late 2019, generating a pandemic crisis with high numbers of COVID-19-related infected individuals and deaths in manifold countries worldwide. Lessons learned from COVID-19 can be used to prevent pandemic threats by designing strategies to support different policy responses, not limited to the health system, directed to reduce the risks of the emergence of novel viral agents, the diffusion of infectious diseases and negative impact in society.
- COVID-19
- coronavirus infections
- infectious diseases
- viral agents
- public health capacity
- resili-ence
- risk assessment
- crisis management
- bounded rationality
- country monitoring
- pandemic re-sponse
- preventing transmission
- preparedness
1. Introduction
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which appeared in late 2019 [1]. SARS-CoV-2 and its mutations have generated a pandemic with high numbers of infected individuals and deaths in manifold countries worldwide [2,3]. In this context, it is important to design strategies of crisis management to cope with/prevent pandemics of novel infectious diseases similar to COVID-19. The concept of strategy has a critical role in a framework of crisis management [4]. Strategy is a current mode of cognition and action to enable individuals and/or organizations to take advantage of important opportunities or to cope with consequential problems and/or environmental threats in society, such as pandemics, earthquakes, etc. Nations and their institutions have to prepare long-run strategies and specific plans of crisis management for pandemic threats to guide timely processes of decision-making to support the application of effective actions and interventions for solving consequential problems in society [4,5]. Strategies of crisis management should deal with pandemic threat before the emergence and in the presence of an unforeseen pandemic, they have to reduce negative effects in society [6]. The main goal of these strategies is to reduce hazards and risks that certain factors pose to public health and the environment, and solve the problems of pandemic crises with effective and rapid decisions directed to policy responses for reducing uncertainty and supporting, as soon as possible, the recovery of socioeconomic systems. In particular, strategies of countries for unforeseen pandemic crisis can be [7–9]:
- Responsive, based on the application of a previous plan of interventions ready to be used that endeavors to solve all consequential problems of pandemic crisis.
- Preventive, based on the planned interventions directed to reduction of risk factors associated with the emergence and diffusion of pandemics, and the design ex-ante of effective solutions for problems generated by a pandemic threat/crisis, preparing rapid strategic actions to stop or reduce negative effects in society.
The logical structure of these strategies of crisis management is based on the following vital aspects:
- Analysis of the causes, hazards, risk factors and effects of pandemic threat (problem) in society, and possible solutions.
- Analysis of a limited number of variables associated with proposed solutions for achieving and sustaining specific goals given by the reduction of hazards and risk factors of the emergence of pandemics or negative effects in the presence of ongoing pandemic in society.
- Analysis of different solutions to pandemic threats and crises, and evaluation of pros and cons.
- Choice of the satisfying solution in the context of limited rationality and a turbulent environment.
- Application of the critical decision of problem solving for achieving the goals, evaluating expected results in a short period of time to refine and improve the decision-making process with continuous learning processes.
- Str
- An
- a
- lysis of
- tegies of Crisis Management in the Presence of Pandemic Similar to COVID-19
- he causes, hazards, risk factors and effects of pandemic threat (problem) in society, and possible solutions.
- Analysis of a limited number of variables associated with proposed solutions for achieving and sustaining specific goals given by the reduction of hazards and risk factors of the emergence of pandemics or negative effects in the presence of ongoing pandemic in society.
- Analysis of different solutions to pandemic threats and crises, and evaluation of pros and cons.
- Choice of the satisfying solution in the context of limited rationality and a turbulent environment.
- Application of the critical decision of problem solving for achieving the goals, evaluating expected results in a short period of time to refine and improve the decision-making process with continuous learning processes.
2. Strategies of Crisis Management in the Presence of Pandemic Similar to COVID-19
Nicoll and Coulombier ([10], p. 3ff) describe two main strategies to cope with pandemics:
- Containment strategies that endeavor to stop the diffusion of pandemics and epidemics in society. These interventions are directed to prevent vast chains of transmission and outbreaks, with public policies of quarantine and full lockdown associated with an accurate tracing of infections, isolation of infected people and timely treatments of patients [11] (cf., Figure 1).
Mitigation strategies based on social distancing, school closures, facemasks wearing, etc. that endeavor to decrease the pandemic diffusion and the pressure of high hospitalization and admission to intensive care units as well as protecting elderly and other people with high vulnerability (e.g., having cancer and other serious diseases).
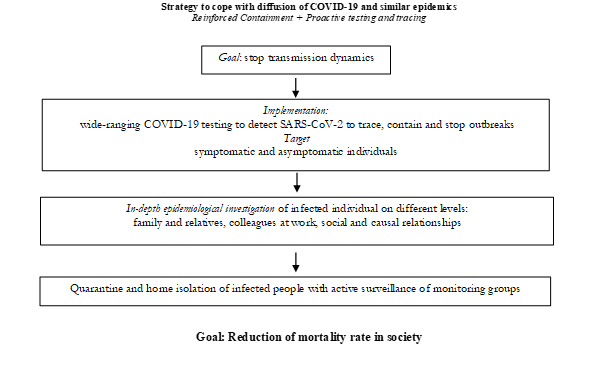
Figure 1. Containment strategy to support policy responses directed to cope with COVID-19 pandemic crisis and similar epidemics in future. Source: author’s own figure.
During the COVID-19 crisis and similar pandemics, many countries initially proposed a containment policy (quarantine and general lockdown) and subsequently mitigation measures, such as social distancing, disinfection of buildings, face masks wearing, travel restrictions, etc. [12–14]. The study by Renardy et al. [15] shows that a longer duration of lockdown that postpones the reopening of stores and the circulation of people does not decrease confirmed cases of infections and inter-related negative effects on public health, but a longer duration of lockdown only defers these problems in a not-too-distant future. Instead, specific mitigation policies directed to diminish contacts among people in specific places can effectively lower the peak of pandemic waves and consequential negative effects in society.
Migone [16] discusses the correlation between national policy characteristics and the success in “flattening the curve” of COVID-19. This study shows that the best correlation is found when looking at the pattern of choice related to either proactive or reactive approaches to the implementation of containment measures. This result is stronger for countries having either very low or very high infection rates per million people. Instead, in the presence of intermediate rates, a variety of institutional, political, and socioeconomic variables intervene in the process. Scholars also maintain that specific public places create groups of people for social activities that generate a high risk of infection (e.g., pub, bar, cafeteria, gym, etc.) [17]. A selected strategy to control the groups of people in these public places by the application of non-pharmaceutical measures of protection (e.g., facemasks wearing, social distancing) are more effective strategies to reduce confirmed cases than full lockdown of overall social and economic activities [17].
In general, non-pharmaceutical measures are health policies having the goal of lowering the peak of the pandemic wave and the high load on health system [18,19]. However, Brooks et al. [20] report: “negative psychological effects of quarantine including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma.” Marazziti and Stahl [21] argue that the COVID-19 pandemic has generated several disorders of psychiatric interest and relevance. Wang et al. [22] analyzed the deterioration of physical and psychological health during the COVID-19 pandemic and revealed that the subjective deterioration of psychological health was significantly associated with avoiding crowded places and wearing a facemask. Moreover, subjective deteriorations of physical and psychological health are positively associated with general anxiety. Xiong et al. [23] also have shown that the COVID-19 pandemic is associated with highly significant levels of psychological distress that, in many cases, would meet the threshold for clinical relevance. In this context, psychological disorders are also associated with a systematic deterioration of economic system because of containment policies based on a longer duration of lockdown in society that generates high unemployment [11]. Mitigating the hazardous effects of containment policies to cope with infectious diseases (e.g., COVID-19) on mental health should be also a public health priority. In addition, Puci et al. [24] highlight the importance of psychological and psychiatric support services during the COVID-19 pandemic. These services can support the psychological well-being of health care professionals and promote precautionary behaviors among them.
- Strategies for the Prevention of Pandemics
3. Strategies for the Prevention of Pandemics
Specific strategies can reduce the hazards and risk factors of pandemic threats, prevent the emergence of pandemics and reduce negative effects in society. This perspective focuses on health, environmental and institutional strategies [25,26].
3.1. Health Strategies
Daszak et al. [27] highlight some critical aspects for designing strategies directed to the prevention of pandemics, such as:
- control among wildlife to detect the transportation of dangerous pathogens;
- control of the interaction between the population and wildlife to detect, as soon as possible, spillover effects;
- control wildlife trade for enhancing biosecurity in domestic and international markets.
In addition, an intense activity of prevention has to be directed to control and apply biosafety protocols in public and private laboratories of virology that analyze viruses, pathogens and novel viral agents to minimize the possibility of accidental diffusion in the environment and society with consequential socioeconomic issues. In this context, the scientific collaboration among international laboratories plays a critical role in supporting the sharing of vital data and information for helping policymakers to apply plans to prevent/reduce the hazards and risk factors of pandemic threats that can create problems worldwide [1]. This strategy of prevention can be driven by increasing levels of investments in the health sector and R&D, as well as higher levels of health expenditure per capita. In fact, preventive measures and new technology can control the emergence of pandemics and negative effects in society of future pandemics similar to COVID-19 [28]. In the presence of local epidemic outbreak, a rapid contact tracing is a basic strategy within the epicenter to limit human-to-human transmission outside of outbreak areas, also applying appropriate isolation of cases [29]. Hellewell et al. [30] show that the probability of control decreases with long delays from symptom onset to isolation. Contact tracing achieves the early detection and isolation of secondary cases, which play an important role given that the peak in infectiousness occurs during the pre-symptomatic phase. Moreover, the early detection achieved by contact tracing accelerates the rate at which infected individuals receive medical care to improve their chance of recovery. In short, contact tracing is a vital strategy for controlling infectious diseases, such as COVID-19, but protocols apply “forward-trace” to notify people who were recently exposed. Bradshaw et al. [31] found that “bidirectional” tracing to identify infector individuals and their other infectees robustly improves outbreak control. In addition, Kucharski et al. [32] claim that the isolation of cases and contact tracing can be less effective for COVID-19 because infectiousness starts before the onset of symptoms (cf., [33]). Yalaman et al. [34] suggest that comprehensive contact tracing is an instrumental approach not only for curtailing transmission but also to reduce case fatality rates. In fact, the combination of reduced transmission and more rapid recovery reduces the burden on healthcare system, which can save resources for individuals that are infected in the future. According to Kapitsinis [35], investments in the health sector can support these just-mentioned strategies and develop hospital efficiency in admissions of infected people, innovative treatments for novel infectious diseases and new technology driven by R&D labs to foster scientific and technological advances directed to new vaccines, antivirals and other innovative drugs that can avoid and/or control future pandemic threats in countries [1,5,36–42]. Williams et al. [43] argue that effective responses to public health emergencies should rely on translating rapidly emerging research and technology into timely, evidence-informed new policies and best practices, etc., such as appropriate strategies of vaccinations with new mRNA vaccines directed to achieve herd immunity for supporting a drastic reduction in the number of COVID-19-related infected individuals and deaths. In fact, the alarming levels of spread and severity of COVID-19 and novel infectious diseases support the development of new technologies and innovative drugs, such as vaccines based on messenger RNA, known as mRNA vaccines for high levels of protection by preventing COVID-19 (and likely also against its variants) among people that are vaccinated [4]. The mRNA vaccines are based on accumulated knowledge that the infective process itself is effective in raising an immune response; as a consequence, genetic engineering can be utilized to construct virus-like particles from the capsid and envelope proteins of viruses [44,45]. Moreover, mRNA vaccines eliminate a lot of phases in the manufacturing process for the development of new drugs because rather than having viral proteins injected, the human body uses the instructions to manufacture viral proteins itself. In short, R&D investments in new technologies have developed mRNA vaccines that are produced and manufactured by chemical rather than biological synthesis; in this case, the process of technological development is much faster than conventional vaccines to be redesigned, scaled up and mass-produced [24,46]. Manifold public agencies in the United Kingdom, the USA, Europe and other countries for protecting and promoting the health of people through control and supervision confirm that mRNA vaccines for COVID-19 can be effective and safely tolerated in populations [46–50].
3.2. Environmental Strategies
Studies have found that sustainable environment plays a vital role to reduce risk factors of epidemics and prevent pandemics similar to COVID-19 [1,51]. Scholars maintain that a low rate of fatality is associated with a low level of air pollution [1,51–54]. Studies have also shown that countries with 72% of the population exposed to levels exceeding the WHO guideline value of air pollution have lower fatality rates of COVID-19 than countries with 98% population exposed to similar levels of air pollution [55]. Coccia [1] demonstrates that polluted cities should not exceed 48 days per year of high levels of air pollution, in the presence of climate conditions having little wind, because when the annual period of air pollution is higher than 100 days, the reduction of air quality and other factors can damage the health of the population and support the transmission dynamics of infectious diseases in society with consequential socioeconomic problems [53,56].
In fact, polluted cities have to apply an environmental policy to reduce the main sources of air pollution and, at the same time, improve urban ventilation to foster the dispersion of particulate compounds emissions, considering morphological characteristics of the openness of surrounding areas [57], the coverage and heights of buildings that affect the surface roughness, etc. [58,59]. Moreover, countries must support, more and more, sustainable mobility as engine of socioeconomic change and redesign cities for people using urban planning that improves public respiratory health. The hazards of the association between air pollution and viral infectivity in cities have to induce a reduction of the motorization rate of polluting machines with a sustainable transition to new electric vehicles, generating a revolution in society [1]. In short, environmental strategies can foster sustainable mobility by enhancing local, urban and commuter public transport with electric vehicles and creating vast low emission zones within cities. In this context, countries and supranational organizations have to launch a roadmap directed to sustainable growth with the aim of zero emissions in all socioeconomic systems. Wang and Zhu [60] argue that a strategy of renewable energy and sustainable technology facilitates CO2 abatement, reducing air pollution, improving air quality and the health of people. In fact, studies have shown the positive effects of the reduction of air pollution on the health of people in terms of lower premature deaths and related morbidity [61]. Hence, geo-economic regions have to, more and more, apply long-run environmental policies and sustainable strategies to reduce the level of particulate compounds emissions that damage the health of people and may be associated with the diffusion of viral agents, generating socioeconomic issues [53–56].
3.3. Institutional Strategies
Resilient systems to pandemic shocks must have strong institutions and good governance driven by adequate and effective leadership that supports population needs. effective governance has to support preparedness to pandemic threats with constant investments in the health system to reduce mortality, morbidity and stress among the population, and promote socioeconomic recovery [11,53–56,62]. Sagan et al. [63] confirm that in Europe, good governance in countries has played a critical role to support a resilient response of the health system in the presence of the COVID-19 pandemic crisis. In particular, Sagan et al. [63] consider a broad concept of governance, not limited to the health system alone, that creates the institutional background to support economic and social systems of the nation and its government to work properly for preventing and/or coping with pandemic threats and crises. In fact, Sagan et al. [63] pinpoint that the prevention of pandemic threats is based on: (1) appropriate and effective governance of institutions and (2) skilled human capital with interdisciplinary technical capacity of crisis management to respond in a short period of time.
Other factors for effective strategies to prevent and/or reduce risks of future pandemic crises can be:
- Leveraging operational levels based on medical personnel, epidemiologists, biologists, emergency managers, and other professionals for coping with pandemic’s threat.
- Creating a network of innovators with a great variety of expertise and capability in different fields to support policy decisions and their timely implementation [64].
- Fostering academic institutions and leading scholars that play a vital role in supporting rational decisions of governments [65,66].
- Creating stable collaborations across different structures, such as academic and administrative institutions, to accelerate the learning process to prevent and/or cope with pandemic threat/crisis [67].
In this context, the COVID-19 pandemic crisis has pushed the boundaries on what is possible for rapid pandemic responses in several areas, including healthcare system, vaccine research, development, manufacturing, distribution, allocation, and administration. These actions can support learning processes directed to improve preparedness efforts of nations to advance timely public responses in the short term and support R&D for developing efficient pandemic and seasonal influenza vaccines. New strategies of vaccination plans of nations have to be highly responsive, flexible, resilient, scalable, and more effective for reducing the impact of seasonal and pandemic influenza viruses. In general, vaccine roll-out plans have to face distribution and allocation hurdles, and new mutations of SARS-CoV-2, likely more transmissible and resistant to vaccines, can change the equation of herd-immunity, increasing the thresholds of immunization in the population [68–70]. A delay of vaccination plan and of the achievement of optimal threshold within countries does not reduce transmission dynamics and can foster the emergence and diffusion of novel mutations of viral agents, such as in Brazil and India [71–73]. In short, the timely achievement of the optimal threshold of doses administered to population is a critical goal, because an effective vaccination plan can quickly and thoroughly prevent a new mutation of the novel coronavirus from accelerating transmission dynamics in society with consequential socioeconomic issues [74].
Overall, then, success or failure of strategies to prevent pandemic threats and crises depend on effective decision-making in the presence of uncertainty, turbulent environment and highly restricted time [4]. Studies show that the general guidelines for an efficient strategy to cope with pandemic threats have to increase health expenditures and R&D investments for supporting effective policy responses that decrease hazards and risk factors and as a consequence negative effects on population and environment [1,4,56]. Figure 2 shows these critical aspects for preventing and/or controlling the risk factors of future pandemics.
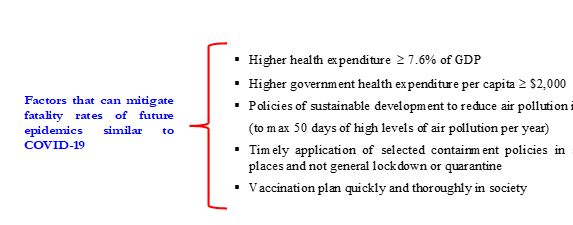
Figure 2. Factors associated with strategies to prevent negative effects of pandemic threats. Source: author’s own figure.
Finally, the proposed ambidexterity strategies of crisis management for more prosperous or less favored countries are [75]:
- Rich countries can focus in the short run on measures of containment of shorter duration because of a stronger healthcare sector based on high expenditures (as % of GDP), whereas in the long run these countries should support environmental policies for reducing air pollution and improving sustainability of ecosystems.
- Developing countries have to focus in the short run on measures of containment of a longer duration because of a weak healthcare sector based on low expenditures (as % of GDP) and in the long run, they have to support public policies for enhancing health system and health of people.
3.4. A Systemic Strategy of Crisis Management to Cope with and/or to Prevent Pandemics Similar to COVID-19
Nations in the presence of a pandemic threat are directed to three strategic goals:
- The application of technological innovations and new technologies for improving actions that prevent the emergence of pandemics and/or contrast the vast diffusion of epidemics or pandemics, such as monitoring, recognition, contact tracing, etc.
- The acceleration of R&D for developing effective vaccines.
- The production, on a vast scale, of new vaccines and innovative drugs to minimize socioeconomic issues and support recovery.
In the next years, countries have to increase R&D investments in equipment, organized infrastructures and education of human resources for improving preparedness activity to react quickly in the presence of inevitable pandemics, also reinforcing international collaboration with key subjects for reducing negative effects on public health between different socioeconomic systems [76].
Hence, in responding to a constant pandemic threat of novel viral agents in the future, the international communities have to reinforce prevention and preparedness in crisis management [4]. In particular, nations and international organizations have to design and implement strategic actions given by improvements of the early warning system and timely containment operations. Moreover, preparedness activities should reinforce the coordination of global science and research to accelerate the R&D and diffusion of effective pandemic vaccines and innovative antiviral drugs.
The strategic actions to prevent pandemic threats can be systematize as follows:
- Reinforce the early warning systems in the international community using existing infrastructure to ensure rapid detection of suspected cases in humans based on rapid and reliable international laboratories that receive all the data and clinical specimens needed for an accurate evaluation of an emergence of pandemic risk.
- Establish rapid containment policies to prevent an increase in the spread of novel viruses in human society and/or, whenever possible, delay its transmission dynamics in the international community. New studies show that selected restrictions in specific places are better policy responses than full lockdown [11,17,77,78]. Health policy should apply a crisis management team to quickly use global and regional stocks of antiviral drugs and other similar drugs to contain negative effects in society in the initial phase of diffusion.
- Verify that all countries have designed and tested pandemic response plans and that international organizations are able to assume a leadership and provide clear guideline to coordinate nations during a pandemic. Developing countries having limited economic resources have to be supported in the development of pandemic plans to reduce gaps in basic capacities for improving an equally and coordinated global response to a pandemic threat or crisis.
- Nations should jointly invest and coordinate global R&D to produce pandemic vaccines and antiviral drugs that are rapidly and widely available as soon as the emergence of a pandemic and/or the diffusion of the novel virus appear. In particular, nations should identify priority research areas and foster funding to public- and private firms involved in R&D of innovative drugs. It is also important to gather and analyze more data on the use of established and new anti-viral drugs and vaccines for a safe administration of treatment and prophylaxis in all of the population. Foster partnerships among governments, regulatory authorities, universities, research laboratories, incumbent and new entrant firms to support R&D of novel drugs and in particular a timely vaccine manufacturing capacity that ensures equitable access across all nations. Moreover, R&D investments have to be directed to new vaccines conferring long-lasting protection against novel viruses and their mutations. Finally, organizations and nations should foster scientific networks and laboratories to ensure that new scientific knowledge about ongoing pandemic and treatments has a rapid and wide-spread communication in real time worldwide.
These strategic actions have to achieve and sustain the main goal of reducing hazards and risk factors of pandemic threats and, in the presence of pandemic, providing, whenever possible, a vast immunological protection of people before they are exposed to novel viral agents. Tsiotas and Magafas [79], using network analysis, show stability of hubs and instability of medium and low-degree nodes, implying a low probability of meeting maximum (infection) values in the future and high uncertainty in the variability of other values below the average. Hence, the challenge is the design of environmental, health and social policies of prevention, and the production of appropriate and safe vaccines that meet global needs shortly after the emergence of a pandemic in order to provide equitable access between countries. In this context, nations have to support scientific institutions for R&D of new vaccines and the applications of new technologies that could prevent chains of transmission, increase vaccine supplies, timely distribution for a broad-spectrum and enduring protection against pandemics across populations worldwide. All these aspects are basic for a strategic approach to cope with and/or prevent pandemic threats.
- Conclusions and Prospects
4. Conclusions and Prospects
Strategies of crisis management to prevent the COVID-19 pandemic and similar epidemics are based on effective multi-level governance, combining both supranational, national, regional and urban strategies to provide timely policy responses for improving health safety in society [75]. The experience of COVID-19 suggests that future infectious diseases of novel viruses can generate, more and more, a serious pandemic threat to public health of countries and their economies [11,77,80–82]. New pandemics, similar to COVID-19, can emerge and spread rapidly and it is important to ensure timely gathering and sharing of information, and samples of novel viral agents for appropriate interventions to stop the emergence of epidemics/pandemics. The preventive strategies also have to support the process of R&D directed to effective vaccines and subsequent production and distribution as soon as possible across countries to mitigate fatality rates, deterioration of economic growth and overall socioeconomic systems. Nations have to design a crisis management team for managing strenuous situations given by pandemic threats and for taking timely critical decisions to resolve them, as far as possible. Successful crisis management teams understand the specificity of pandemic crisis and are thoroughly prepared for solving all problems and problematic situations. Moreover, in a crisis, leaders are expected to reduce uncertainty, providing an authoritative account of problems, solutions and difficulties. Moreover, leaders have to formulate and guide a strategy to cope with pandemic crises that has to be accepted by other institutional, economic and social parties having different positions and interests. The COVID-19 pandemic crisis has supported new and rapid pandemic responses in several areas, including healthcare system, vaccine research, health technologies, environment as well as the development of innovative vaccines. These strategic actions of pandemic management have triggered learning processes to improve preparedness efforts of countries to advance timely critical decisions and efficient investments in R&D processes of innovative drugs and new pandemic vaccines [5,38,40].
Hence, strategies for pandemic threats have to be, more and more, based on efficiency, flexibility, responsiveness and resiliency for decreasing negative effects of vast infectious diseases in society. Evans and Bahrami [83] suggest actions directed to super-flexibility and resilience [84]. Moreover, complex and unforeseen problems of pandemic crises should be treated with strategies of dissolution directed at eliminating sources of pandemic threats in society and improving the capacity of nations to react [4,77,85]. These strategies to prevent and cope with novel infectious diseases have to apply plans and decisions based on ecological rationality, considering a comparative evaluation of performance with other countries applying alternative interventions. This comparative analysis can improve collective learning processes for effective decision-making across countries in turbulent environments with pandemic crisis [86,87]. In short, the development of these capacities can collectively improve the world’s ability to defend itself against many emerging and epidemic-prone diseases. International experience for the COVID-19 pandemic crisis has shown that well-planned public policies, scientific and economic coordination policies are effective interventions for reducing high-risk aspects before and during an outbreak.
Overall, then, a comprehensive strategy of crisis management for pandemic threats has to be also based on environmental and socioeconomic factors, and new technology, and not only on parameters related to medicine, to help policymakers to evaluate manifold aspects that reduce institutional and social vulnerabilities to epidemics and design appropriate short- and long-run plans to prevent and/or contain the negative impact of future infectious diseases on public health, the economy and society [88–90]. To conclude, in the presence of a constant pandemic threat, a comprehensive strategy to prevent future epidemics similar to COVID-19 has to be designed considering manifold aspects associated with sustainability, environmental and socioeconomic sciences, and not only aspects related to life sciences, such as biology and medicine.
