Neuralgic amyotrophy, also called Parsonage–Turner syndrome, in its classic presentation is a brachial plexopathy or a multifocal neuropathy, involving mainly motor nerves of the upper limb with a monophasic course. Recently, a new radiological entity was described, the hourglass constriction, which is characterized by a very focal constriction of a nerve, or part of it, usually associated with nerve thickening proximally and distally to the constriction. Another condition, which is similar from a radiological point of view to hourglass constriction, is nerve torsion. The pathophysiology of neuralgic amyotrophy, hourglass constriction and nerve torsion is still poorly understood, and a generic role of inflammation is proposed for all these conditions.
- hourglass-like constriction
- nerve torsion
- neuralgic amyotrophy
- radial nerve palsy
- anterior interosseous nerve palsy
- posterior interosseous nerve palsy
- neurolysis
1. Introduction
2. NA, Hourglass Constriction and Nerve Torsion
Some authors recently hypothesized that some cases of NA, after a first phase characterized by nerve inflammation and swelling, in particular anatomical conditions, could evolve into hourglass constriction and/or in nerve torsion [8,20][5][6] (Figure 1).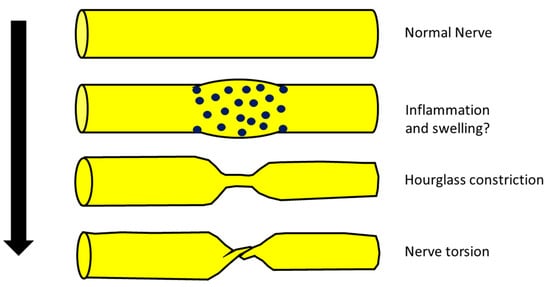
- (a)
-
Typical NA is characterized by brachial plexus involvement, while hourglass constriction and nerve torsion are mainly found in the radial nerve, PIN and AIN [21,22,23][7][8][9]. Hence, the topography of typical involvement is clearly different.
- (b)
-
The classic clinical phenotype of NA is characterized by strong and invalidating pain that, on the other hand, is not the main feature of hourglass constriction (some pain or sensory symptoms are usually present but not invalidating) [2,24][2][10].
- (c)
-
From a neurophysiological point of view, the typical picture of NA is the main or exclusive involvement of motor fibers, even in the case of mixed nerve involvement. On the other hand, hourglass constriction/nerve torsion usually affects both motor and sensory fibers at the same time and with the same severity. Motor fibers are exclusively included only in the case of pure motor nerve involvement (e.g., PIN and AIN) [25,26][11][12].
- (d)
-
Classic NA is historically associated with a spontaneous and quite good prognosis, while hourglass constriction/nerve torsion is usually associated with a bad prognosis, unless neurosurgical treatment is undergone [8,27][5][13].
3. Best Diagnostic Approach for These Conditions
3.1. Neuroimaging
It is now well accepted that nerve imaging is necessary for identifying hourglass constrictions/nerve torsion pre-surgically in patients with acute mononeuropathy/plexopathy. Ultrasound (US) is a very reliable and cost-effective technique which carries a high rate of identification and localization of the constriction [30][14]. It is a useful tool for diagnosis, and it is consistent with intraoperative findings, as shown in Figure 2.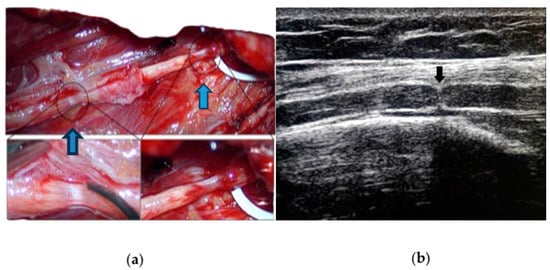 Figure 2. (a) Intraoperative appearance of spontaneous (blue arrows) double left radial nerve constriction; (b) preoperative ultrasound of the same nerve (black arrow) showing a typical hourglass constriction, with the indentation of the hyperechoic epifascicular epineurium.In hourglass constriction when following the nerve course with a transverse scan, there is a sudden and usually marked reduction in the nerve cross-sectional area, usually accompanied by the hyperechoic aspect of the nerve with loss of fascicular structure. Proximally and distally to this site, the cross-sectional area of the nerve is usually increased. At this level, the fascicles are usually increased in size with an aspect varying from hypo- to hyperechoic, probably according to the prevalence of oedema and fibrosis.Longitudinal scans show the typical appearance of an hourglass-like lesion [31,32][15][16]. Nevertheless, US may fail to identify the constriction if the involved nerve is too deep or located under the bones or other body structures blocking the ultrasound beam. Moreover, the assessment is highly operator-dependent. MRI, particularly 1.5 and 3 Tesla scanning, has an important role [33][17], although it is more expensive, more time-consuming and not widely available in clinical practice. As in the case of US, MRI is highly operator-dependent, especially when it comes to the choice of the appropriate protocol (this can also be quite time-consuming) and imaging interpretation. It can immediately show, proximal to the constriction site, peripheral signal hyperintensity and central hypointensity on intermediate-weighted FSE and/or fat-suppressed imaging, orthogonal to the longitudinal axis of the nerve (“bullseye sign”) [34][18].
Figure 2. (a) Intraoperative appearance of spontaneous (blue arrows) double left radial nerve constriction; (b) preoperative ultrasound of the same nerve (black arrow) showing a typical hourglass constriction, with the indentation of the hyperechoic epifascicular epineurium.In hourglass constriction when following the nerve course with a transverse scan, there is a sudden and usually marked reduction in the nerve cross-sectional area, usually accompanied by the hyperechoic aspect of the nerve with loss of fascicular structure. Proximally and distally to this site, the cross-sectional area of the nerve is usually increased. At this level, the fascicles are usually increased in size with an aspect varying from hypo- to hyperechoic, probably according to the prevalence of oedema and fibrosis.Longitudinal scans show the typical appearance of an hourglass-like lesion [31,32][15][16]. Nevertheless, US may fail to identify the constriction if the involved nerve is too deep or located under the bones or other body structures blocking the ultrasound beam. Moreover, the assessment is highly operator-dependent. MRI, particularly 1.5 and 3 Tesla scanning, has an important role [33][17], although it is more expensive, more time-consuming and not widely available in clinical practice. As in the case of US, MRI is highly operator-dependent, especially when it comes to the choice of the appropriate protocol (this can also be quite time-consuming) and imaging interpretation. It can immediately show, proximal to the constriction site, peripheral signal hyperintensity and central hypointensity on intermediate-weighted FSE and/or fat-suppressed imaging, orthogonal to the longitudinal axis of the nerve (“bullseye sign”) [34][18].3.2. Neurophysiology
Neurophysiology should be performed in all cases and is necessary to confirm the clinical diagnosis in terms of location of the damage and type of nerve damage (demyelination vs. axonal vs. conduction block). Moreover, a broad examination can detect subclinical involvement of more nerves, guiding the diagnosis toward vasculitis or a genetic or inflammatory neuropathy. The correct identification of the pathology and type of damage is of the uttermost importance for the prognosis and guiding treatment as well. The neurophysiological correlate of hourglass constriction is still not so clear and in many works is not well specified. This is probably related to the absence of a focus on this aspect in many works that are not reported by neurologists or neurophysiologists.
3.3. Differential Diagnosis of Acute Mononeuropathies and Related Examinations
Acute mononeuropathies are usually caused by compression (increased risk in cases of diabetes, hypothyroidism, weight loss or gain, alcoholism, acromegaly); all these pathologies should be considered. The evidence of neurophysiological and neuroimaging signs of nerve sufferance in a typical site of entrapment should suggest this diagnosis. There are, however, other pathologies that can cause isolated mononeuropathy, e.g., in some cases, the early manifestation of multineuropathy. Among these, there are systemic and non-systemic vasculitis, infectious diseases (leprosy, HIV), inflammatory diseases (sarcoidosis, MMN, CIDP variants) and toxic, metabolic (diabetes) and hereditary diseases (HNPP, hereditary neuralgic amyotrophy). Peripheral nervous system impairment is frequent in most necrotizing vasculitis, with an ischemic–hypoxic mechanism due to arterial vessel occlusion secondary to vessel wall necrosis, mainly causing multineuropathies. This can occur both in primary forms (such as polyarteritis nodosa, Churg–Strauss syndrome, Wegener’s granulomatosis) and secondary forms (in the course of neoplasms, infectious diseases such as HCV, connective tissue diseases such as SLE, rheumatoid arthritis, Sjogren’s syndrome, scleroderma, rheumatic fever, amphetamines use) [38,39][19][20]. Infectious disease can cause direct nerve involvement, as in the case of leprosy [40][21]. Leprosy neuropathy is the second most common neuropathy in the world (after diabetic neuropathy), and it is due to direct invasion of the skin and nerves by M. leprae. Leprosy is endemic in tropical and subtropical regions; in other areas, it is suspected in people from or who have stayed in endemic areas. The diagnosis is confirmed by histological examination of the cutaneous lesions with evidence of acid-resistant bacteria. Opportunistic CMV infection in HIV causes lumbosacral polyneuropathy but can also cause predominantly sensitive multineuropathy with pain and dysesthesia. Lyme disease can manifest as multineuropathy, mononeuropathy or brachial plexopathy, which can mimic brachial neuritis [41][22]. Chronic hepatitis from HCV (and HBV) carries a risk of developing predominantly axonal sensory and sensorimotor poly- and multineuropathies usually associated with cryoglobulinemia (the presence of serum immunoglobulins which precipitate at low temperatures and solubilize at 37°) or autoimmune vasculitis [42][23]. Other rare causes are possible. Sarcoidosis is a chronic multisystem inflammatory granulomatosis, which in 5–10% of cases can affect the nervous system and in 1% the peripheral nervous system [43,44][24][25]. Radiculopathies or mono-multineuropathies due to granulomatous infiltration, usually slowly progressive, may occur. Multifocal motor neuropathy (MMN) may present initially as mononeuropathy and is neurophysiologically characterized by the presence of conduction blocks [45,46][26][27]. In multiple myeloma, there may rarely be multineuropathy caused either by infiltration of malignant plasma cells or by interstitial deposition of paraprotein or light chains [47,48][28][29]. Diabetes is the most frequent cause of neuropathy, and the main risk factors are the duration of the disease and the blood sugar level [49][30]. It can cause different clinical pictures. While the typical and more common symmetrical polyneuropathy has a predominantly toxic–metabolic etiology, the rarer mono-multineuropathic forms are due to vascular alterations in the vasa nervorum. The cranial nerves can be affected, particularly the third, but peripheral nerves of the limbs and trunk can also be impacted; in both cases, the genesis is ischemic. Environmental and occupational exposure to lead, which is still widespread in developing countries, can cause axonal motor neuropathy, mainly of the radial nerve (with hand drop) but also of the tibialis anterior (foot drop). Acute intermittent porphyria is the most common of the hepatic porphyrias. It is caused by a deficiency of the porphobilinogen synthetase enzyme and manifests as attacks of abdominal pain associated with fever, vomiting and leukocytosis. Sometimes there is neurological involvement with acute onset motor deficits and a multineuropathic distribution [50][31]. Hereditary neuropathy with liability to pressure palsies (HNPP), a rare autosomal dominant hereditary neuropathy caused by deletion of the PMP22 gene, is a polyneuropathy conferring an increased susceptibility to acute damage from the compression or entrapment of peripheral nerves. It manifests usually as acute transient peripheral paralysis with a mononeuropathic distribution that is not usually accompanied by strong pain. The nerve damage can regress spontaneously within a few days or weeks or persist for a long time. NA can sometimes be hereditary (hereditary neuralgic amyotrophy). This autosomal dominant hereditary form of neuralgic amyotrophy is caused by mutations in the SEPT9 gene, leading to recurrent episodes of typical brachial neuritis [53,54][32][33]. In order to make a correct diagnosis, a full anamnesis could be very helpful. Diabetes, a history of rheumatic diseases, staying in or coming from areas at risk for infectious pathologies and exposure to industrial toxicants could indicate diagnosis.4. Best Treatment Approach for These Conditions
According to a Cochrane review, there are limited conservative treatment options in NA, and there is no evidence from randomized trials to support any particular form of treatment. In particular, some evidence suggests that early corticosteroid therapy may be effective against pain and lead to an earlier recovery, but there is no evidence of significant long-term improvement if compared with patients not treated with corticosteroids [55][34]. There is no consensus on hourglass constriction treatment either. Conservative options include observation, resting and physical therapy to cope with muscle weakness, along with medications to control pain, nonsteroidal anti-inflammatory drugs and steroids, but there is no evidence of the effectiveness of these approaches. Some authors have suggested treating patients conservatively for 3 to 6 months, and afterward considering surgery if no improvements occur [56,57][35][36]. The type of surgical treatment implemented also varies in the literature. The most adopted is internal neurolysis, which allows a decompression of the internal components of the nerve promoting recovery [59][37]. Resection of the affected segment with direct neurorrhaphy, or with the interposition of an autologous nerve graft, has also been reported. The use of more complex surgical techniques, such as tendon transfers, is sporadic [60][38]. This technique should be limited to cases without any chance of spontaneous recovery, such as after failed neurosurgical treatment, or when severe chronic muscle atrophy and fibrotic substitution are observed (meaning at least after more than 1 year after the onset) [61][39]. The prognosis is generally favorable after surgery, with a high rate of good motor recovery. Surprisingly, overall, the surgical technique seemed to not influence the clinical outcome. This finding might simply signify that the chosen surgical treatment was appropriate for the nerve lesion, but still, the literature lacks the elements necessary to correlate the grade of nerve lesion to the best possible treatment, and both to the outcome. More data regarding the correlation between a common severity grading and the postoperative outcome are needed, as well as further parameters to predict the clinical outcome. The parameters that should be considered for this purpose could be the entity of constriction, the presence on the same nerve of more sites of constriction (as described in some cases) and the severity of nerve damage, assessed through neurophysiology. In compressive neuropathies, prolonged compression may lead to demyelination and axonal loss, as well as nerve fascicle swelling, leading to epineural fibrosis. In these cases, which share similarities with cases of hourglass constriction, ultrasound-guided hydrodissection with different injectates (for example, normal saline, corticosteroids, local anesthetics, dextrose and platelet-rich plasma) has been demonstrated to provide not only a mechanical effect of releasing and decompressing the entrapped nerves but also a pharmacological effect relieving pain and promoting nerve healing through numerous mechanisms [25,37][11][40]. Since hourglass constriction and nerve torsion have a different treatment and prognosis than other cases of acute mononeuropathy/plexopathy without evidence of nerve constriction or torsion, it is of the uttermost importance to perform a correct diagnosis
References
- Smith, C.C.; Bevelaqua, A.C. Challenging pain syndromes: Parsonage-Turner syndrome. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 265–277.
- Van Eijk, J.J.; Groothuis, J.T.; Van Alfen, N. Neuralgic amyotrophy: An update on diagnosis, pathophysiology, and treatment. Muscle Nerve 2016, 53, 337–350.
- Seror, P. Neuralgic amyotrophy: An update. Jt. Bone Spine 2017, 2, 153–158.
- Farr, E.; D’Andrea, D.; Franz, C.K. Phrenic Nerve Involvement in Neuralgic Amyotrophy (Parsonage-Turner Syndrome). Sleep Med. Clin. 2020, 15, 539–543.
- Glorioso, D.; Palestini, R.; Cuccagna, C.; Lauretti, L.; Padua, L. Nerve Torsion as a Pattern of Parsonage-Turner Syndrome: Literature Review and Two Representative Cases. J. Clin. Med. 2023, 12, 4542.
- Sneag, D.B.; Urban, C.; Li, T.Y.; Colucci, P.G.; Pedrick, E.G.; Nimura, C.A.; Feinberg, J.H.; Milani, C.J.; Tan, E.T. Hourglass-like constrictions on MRI are common in electromyography-confirmed cases of neuralgic amyotrophy (Parsonage-Turner syndrome): A tertiary referral center experience. Muscle Nerve 2023. early view.
- Sneag, D.B.; Rancy, S.K.; Wolfe, S.W.; Lee, S.C.; Kalia, V.; Lee, S.K.; Feinberg, J.H. Brachial plexitis or neuritis? MRI features of lesion distribution in Parsonage-Turner syndrome. Muscle Nerve 2018, 58, 359–366.
- McGraw, I. Isolated spontaneous posterior interosseous nerve palsy: A review of aetiology and management. J. Hand Surg. Eur. Vol. 2019, 44, 310–316.
- Sigamoney, K.V.; Rashid, A.; Ng, C.Y. Management of Atraumatic Posterior Interosseous Nerve Palsy. J. Hand Surg. Am. 2017, 42, 826–830.
- Rubin, D.I. Neuralgic amyotrophy: Clinical features and diagnostic evaluation. Neurologist 2001, 7, 350–356.
- Shi, M.; Qi, H.; Ding, H.; Chen, F.; Xin, Z.; Zhao, Q.; Guan, S.; Shi, H. Electrophysiological examination and high frequency ultrasonography for diagnosis of radial nerve torsion and compression. Medicine 2018, 97, e9587.
- Granata, G.; Coraci, D.; Erra, C.; Tsukamoto, H.; Padua, L.; Luigetti, M. Posterior interosseous nerve syndrome due to radioulnar joint cyst. Muscle Nerve. 2013, 48, 842–843.
- Pan, Y.W.; Wang, S.; Tian, G.; Li, C.; Tian, W.; Tian, M. Typical brachial neuritis (Parsonage-Turner syndrome) with hourglass-like constrictions in the affected nerves. J. Hand Surg. Am. 2011, 36, 1197–1203.
- Deng, H.; Lu, B.; Yin, C.; Xu, Y.; Ding, Y.; Mi, Y.; Xu, P. The Effectiveness of Ultrasonography in the Diagnosis of Spontaneous Hourglasslike Constriction of Peripheral Nerve in the Upper Extremity. World Neurosurg. 2020, 134, e103–e111.
- Heiling, B.; Waschke, A.; Ceanga, M.; Grimm, A.; Witte, O.W.; Axer, H. Not your average Saturday night palsy-High resolution nerve ultrasound resolves rare cause of wrist drop. Clin. Neurol. Neurosurg. 2018, 172, 160–161.
- Lee, C.H.; Jeon, T.; Kim, C.U. Value of ultrasound in diagnosis of radial nerve palsy with hourglass-like constrictions without extrinsic compression: A case report. J. Hand Surg. Eur. Vol. 2018, 43, 445–447.
- Kim, D.H.; Sung, D.H.; Chang, M.C. Diagnosis of Hourglass-Like Constriction Neuropathy of the Radial Nerve Using High-Resolution Magnetic Resonance Neurography: A Report of Two Cases. Diagnostics 2020, 10, 232.
- Sneag, D.B.; Saltzman, E.B.; Meister, D.W.; Feinberg, J.H.; Lee, S.K.; Wolfe, S.W. MRI bullseye sign: An indicator of peripheral nerve constriction in parsonage-turner syndrome. Muscle Nerve 2017, 56, 99–106.
- Chan, J.K.; Kennett, R.; Smith, G. Posterior interosseous nerve palsy in rheumatoid arthritis: Case report and literature review. J. Plast. Reconstr. Aesthet. Surg. 2009, 62, e556–e560.
- Ochi, K.; Horiuchi, Y.; Tazaki, K.; Nishi, K.; Kawashima, H.; Yabe, H. Spontaneous anterior interosseous nerve palsy with Churg-Strauss syndrome. Mod. Rheumatol. 2010, 20, 514–517.
- Khadilkar, S.V.; Patil, S.B.; Shetty, V.P. Neuropathies of leprosy. J. Neurol. Sci. 2021, 420, 117288.
- Sindic, C.J. Infectious neuropathies. Curr. Opin. Neurol. 2013, 26, 510–515.
- Silva, F.; Pinto, C.; Barbosa, A.; Borges, T.; Dias, C.; Almeida, J. New insights in cryoglobulinemic vasculitis. J. Autoimmun. 2019, 105, 102313.
- Tavee, J. Peripheral neuropathy in sarcoidosis. J. Neuroimmunol. 2022, 368, 577864.
- Fritz, D.; van de Beek, D.; Brouwer, M.C. Clinical features, treatment and outcome in neurosarcoidosis: Systematic review and meta-analysis. BMC Neurol. 2016, 16, 220.
- Nobile-Orazio, E.; Cappellari, A.; Meucci, N.; Carpo, M.; Terenghi, F.; Bersano, A.; Priori, A.; Barbieri, S.; Scarlato, G. Multifocal motor neuropathy: Clinical and immunological features and response to IVIg in relation to the presence and degree of motor conduction block. J. Neurol. Neurosurg. Psychiatry 2002, 72, 761–766.
- Beadon, K.; Guimarães-Costa, R.; Léger, J.M. Multifocal motor neuropathy. Curr. Opin. Neurol. 2018, 31, 559–564.
- Lucchetta, M.; Padua, L.; Granata, G.; Luigetti, M.; Campagnolo, M.; Dalla Torre, C.; Coraci, D.; Sabatelli, M.; Briani, C. Nerve ultrasound findings in neuropathy associated with anti-myelin-associated glycoprotein antibodies. Eur. J. Neurol. 2015, 22, 193–202.
- Rison, R.A.; Beydoun, S.R. Paraproteinemic neuropathy: A practical review. BMC Neurol. 2016, 16, 13.
- Ricci, L.; Luigetti, M.; Florio, L.; Capone, F.; Di Lazzaro, V. Causes of chronic neuropathies: A single-center experience. Neurol. Sci. 2019, 40, 1611–1617.
- Gerischer, L.M.; Scheibe, F.; Nümann, A.; Köhnlein, M.; Stölzel, U.; Meisel, A. Acute porphyrias—A neurological perspective. Brain Behav. 2021, 11, e2389.
- Meuleman, J.; Timmerman, V.; Van Broeckhoven, C.; De Jonghe, P. Hereditary neuralgic amyotrophy. Neurogenetics 2001, 3, 115–118.
- Hannibal, M.C.; Ruzzo, E.K.; Miller, L.R.; Betz, B.; Buchan, J.G.; Knutzen, D.M.; Barnett, K.; Landsverk, M.L.; Brice, A.; LeGuern, E.; et al. SEPT9 gene sequencing analysis reveals recurrent mutations in hereditary neuralgic amyotrophy. Neurology 2009, 72, 1755–1759.
- van Alfen, N.; van Engelen, B.G.; Hughes, R.A. Treatment for idiopathic and hereditary neuralgic amyotrophy (brachial neuritis). Cochrane Database Syst. Rev. 2009, 2009, CD006976.
- Qi, W.; Shen, Y.; Qiu, Y.; Jiang, S.; Yu, Y.; Yin, H.; Xu, W. Surgical treatment of hourglass-like radial nerve constrictions. Neurochirurgie 2021, 67, 170–175.
- Hashizume, H.; Nishida, K.; Nanba, Y.; Shigeyama, Y.; Inoue, H.; Morito, Y. Non-traumatic paralysis of the posterior interosseous nerve. J. Bone Jt. Surg. Br. 1996, 78, 771–776.
- Vastamäki, M. Prompt interfascicular neurolysis for the successful treatment of hourglass-like fascicular nerve compression. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2002, 36, 122–124.
- Wu, P.; Yang, J.Y.; Chen, L.; Yu, C. Surgical and conservative treatments of complete spontaneous posterior interosseous nerve palsy with hourglass-like fascicular constrictions: A retrospective study of 41 cases. Neurosurgery 2014, 75, 250–257; discussion 257.
- Burns, J.; Lister, G.D. Localized constrictive radial neuropathy in the absence of extrinsic compression: Three cases. J. Hand Surg. Am. 1984, 9A, 99–103.
- Eder, M.; Schulte-Mattler, W.; Pöschl, P. Neurographic course Of Wallerian degeneration after human peripheral nerve injury. Muscle Nerve 2017, 56, 247–252.
