The ketogenic diet has been shown to have a multifaceted effect on the prevention and treatment of cardiovascular diseases (CVD). Among other aspects, it has a beneficial effect on the blood lipid profile, even compared to other diets. It shows strong anti-inflammatory and cardioprotective potential, which is due, among other factors, to the anti-inflammatory properties of the state of ketosis, the elimination of simple sugars, the restriction of total carbohydrates and the supply of omega-3 fatty acids. In addition, ketone bodies provide “rescue fuel” for the diseased heart by affecting its metabolism. They also have a beneficial effect on the function of the vascular endothelium, including improving its function and inhibiting premature ageing. The ketogenic diet has a beneficial effect on blood pressure and other CVD risk factors through, among other aspects, weight loss. The evidence cited is often superior to that for standard diets, making it likely that the ketogenic diet shows advantages over other dietary models in the prevention and treatment of cardiovascular diseases.
- ketogenic diet
- cardiovascular disease
- prevention
- treatment
- KD
- CVD
- heart
1. Introduction
2. The Ketogenic Diet and Blood Lipid Profile
2.1. Lipid Profile and Cardiovascular Diseases
The blood lipid profile is most commonly studied in the form of four parameters, i.e., total cholesterol (TC), low-density lipoprotein (LDL), high-density lipoprotein (HDL) and triglycerides (TG). Abnormalities in these parameters (dyslipidemia) are considered one of the main risk factors for cardiovascular diseases [21][18]. The World Health Organization lists high total cholesterol as one of the risk factors for these diseases [1][2]. A 2022 publication summarizing selected studies in this area found a relationship between higher TC levels and increased cardiovascular mortality [22][19]. Another prospective 10-year cohort study showed the highest risk of ischemic heart disease at total cholesterol levels <155 mg/dL and >185 mg/dL [23][20]. However, there are large discrepancies between the results of different studies due to the different methodological selections. A prospective cohort study of 12.8 million adults found that the lowest mortality from any cause was associated with total cholesterol levels of 210–249 mg/dL. This was true for every age–gender group except men and women aged 18–34 years (180–219 mg/dL for men and 160–199 mg/dL for women) and women aged 35–44 years (180–219 mg/dL) [24][21]. Similar results were presented by the British Heart Foundation and the World Health Organization as early as 2005, based on data from 164 countries from around the world. They showed that the lowest mortality from any cause was associated with TC concentrations between 200 mg/dL and 240 mg/dL. The lowest mortality from cardiovascular diseases was presented in the range of approximately 190–225 mg/dL [25][22]. Low-density lipoprotein (LDL) is considered the so-called “bad cholesterol” and an even more significant risk factor than TC [27,28,29][23][24][25]. A 2023 publication showed that the effect of the LDL cholesterol concentration on the risk of sudden cardiac arrest (SCA) followed a “U” shape, i.e., the highest risk occurred at the lowest and highest LDL concentrations [30][26]. It further appears that the lowest and highest LDL concentrations are also associated with the overall risk of cardiovascular death. However, it is worth noting that very low LDL concentrations are additionally strongly associated with the risk of death from any cause [31][27]. High-density lipoprotein (HDL) is considered the so-called “good cholesterol” and, contrary to LDL, an increase in its concentration is considered a beneficial effect [33][28]. Publications show that it is inversely correlated with CVD mortality [22][19], although both too low and too high concentrations of it may be unfavorable, according to some studies [34,35][29][30]. High triglyceride levels are also considered to increase CVD risk [36][31]. A 10-year-long cohort study from 2021 showed that there was a significant, linear association of triglyceride concentrations with ischemic stroke. However, it appears that here, too, excessively low concentrations (<80 mg/dL) may be associated with an increased risk of death from any cause [23][20].2.2. The Effect of the Ketogenic Diet on the Blood Lipid Profile
The impact of the ketogenic diet on the blood lipid profile is undoubtedly controversial. There are many conflicting data, which may be due to a misunderstanding of certain facts and research methodologies. The high-fat (with frequent high cholesterol) nature of this dietary model contributes to this. As is well known, there is a great deal of controversy about the impact of the amount and type of fat and cholesterol consumed on the blood lipid profile. For a detailed and thorough analysis of the effect of the ketogenic diet on the lipid profile, it is worth discussing recent randomized controlled trials (RCTs) and contrasting them with previous publications on the topic. The authors of a 2022 RCT compared the effect of the ketogenic diet (KD) vs. the standard diabetes diet (SDD) in overweight or obese patients recently diagnosed with type 2 diabetes. Considering the lipid profile, it appeared that the ketogenic diet showed a greater benefit. There was a greater reduction in total cholesterol (from 4.54 ± 0.69 mmol/L to 4.02 ± 0.43 mmol/L vs. from 4.56 ± 0.67 mmol/L to 4.23 ± 0.47 mmol/L in those in the SDD group), triglycerides (from 1.76 ± 0.59 mmol/L to 1. 44 ± 0.26 mmol/L vs. from 1.81 ± 0.78 mmol/L to 1.66 ± 0.46 mmol/L in SDD subjects) and LDL fraction cholesterol (from 2.75 ± 0.65 mmol/L to 2.34 ± 0.45 mmol/L vs. from 2.77 ± 0.69 mmol/L to 2.59 ± 0.58 mmol/L in SD subjects). In addition, HDL fraction cholesterol changed more favorably (increasing from 1.08 ± 0.11 mmol/L to 1.21 ± 0.23 mmol/L vs. from 1.09 ± 0.19 mmol/L to 1.12 ± 0.20 mmol/L in those in the SDD group) [43][32]. It is important that despite the assumption of the same calorie consumption in both groups (1500 ± 50 kcal), the body weights of participants using KD decreased on average from 78.32 ± 15.27 to 70.26 ± 14.79 over 12 weeks. In comparison, the body weights of participants using SDD did not change (from an average of 77.95 ± 14.76 kg to 77.34 ± 13.28 kg). On the one hand, this is an argument in favor of the ketogenic diet; on the other hand, it should be noted that greater benefits in the form of changes in the lipid profile may also result directly from weight loss among participants using KD. In addition, it could also have been influenced by the composition of the diet itself, in which there was a significant share of unsaturated fatty acids from olive oil, avocado and fish. Given the totality of the evidence of the effect of the ketogenic diet on the blood lipid profile, there is certainly a preponderance of evidence of a beneficial effect. There is little evidence to suggest that the ketogenic diet has a worse effect on the overall lipid profile compared to other diets. Often, even if it does not show any greater benefits, it has a comparably beneficial effect to the control diet. This is all the more optimistic given that studies suggesting the cholesterol hypothesis in the context of cardiovascular risk do not meet the Bradford Hill criteria for causality [26][33]. However, the results of the studies are inconclusive and this should be noted. In many studies, there is a reduction in the LDL cholesterol fraction. On the other hand, however, even when it is increased in other studies, the correlation of LDL with cardiovascular diseases does not necessarily imply causality. It has even been shown that people with the highest LDL fraction cholesterol concentrations live as long as or, in most cases, longer than those with normal or low LDL concentrations [63,64][34][35]. Nevertheless, no clear consensus can be formed on the basis of the available research results, although the available scientific evidence mostly shows a positive effect of the ketogenic diet on the blood lipid profile.3. Anti-Inflammatory Potential of the Ketogenic Diet in Cardiovascular Diseases
An indispensable element in the development of cardiovascular diseases is the involvement of inflammation, as demonstrated in a number of studies [65,66,67,68,69,70][36][37][38][39][40][41]. Inflammation has been shown to initiate the early stages of the atherosclerotic process. In addition, as pro-inflammatory cytokines increase, the risk of developing CVD increases. It appears that innate immunity plays a key preventive role here [65,71][36][42]. However, excessive inflammation influences endothelial dysfunction and, as a result, a number of processes (including increased lipoprotein permeability) that result in far-reaching consequences related to, among other outcomes, the development of atherosclerosis [72][43]. Furthermore, psychological stress also initiates inflammation, contributing to an increased risk of developing CVD. This is mediated by an increase in sympathetic nervous system activity as a result of a number of changes occurring related, inter alia, to an increase in the metabolic activity of specific brain areas [73,74,75,76,77][44][45][46][47][48]. This is well supported by the fact that the increased metabolic activity of these areas alone makes it possible to predict the development of coronary heart disease, irrespective of standard risk factors for this disease [78][49]. Importantly, the ageing process itself is also associated with low-grade inflammation, which consequently increases the risk of developing an atherosclerotic process [72][43]. Taking into account the proven anti-inflammatory effects of the ketogenic diet, its beneficial effects on the prevention or treatment of cardiovascular diseases seem reasonable. There are many potential mechanisms through which the ketogenic diet demonstrates its anti-inflammatory potential. However, four main factors can be identified. Firstly, the ketogenic diet places the body into a state of nutritional ketosis (associated, in turn, with a number of different biochemical and physiological mechanisms). The processes occurring during the state of ketosis exert a systemic anti-inflammatory effect, which in turn has a direct bearing on cardiovascular diseases. The second most important factor is the elimination of pro-inflammatory simple sugars from the diet. This is directly reflected within CVD. A high-fat, well-composed ketogenic diet is also rich in omega-3 fatty acids, and their anti-inflammatory and cardioprotective effects are well known, as described in Section 3.4. The main factors are also illustrated in Figure 1.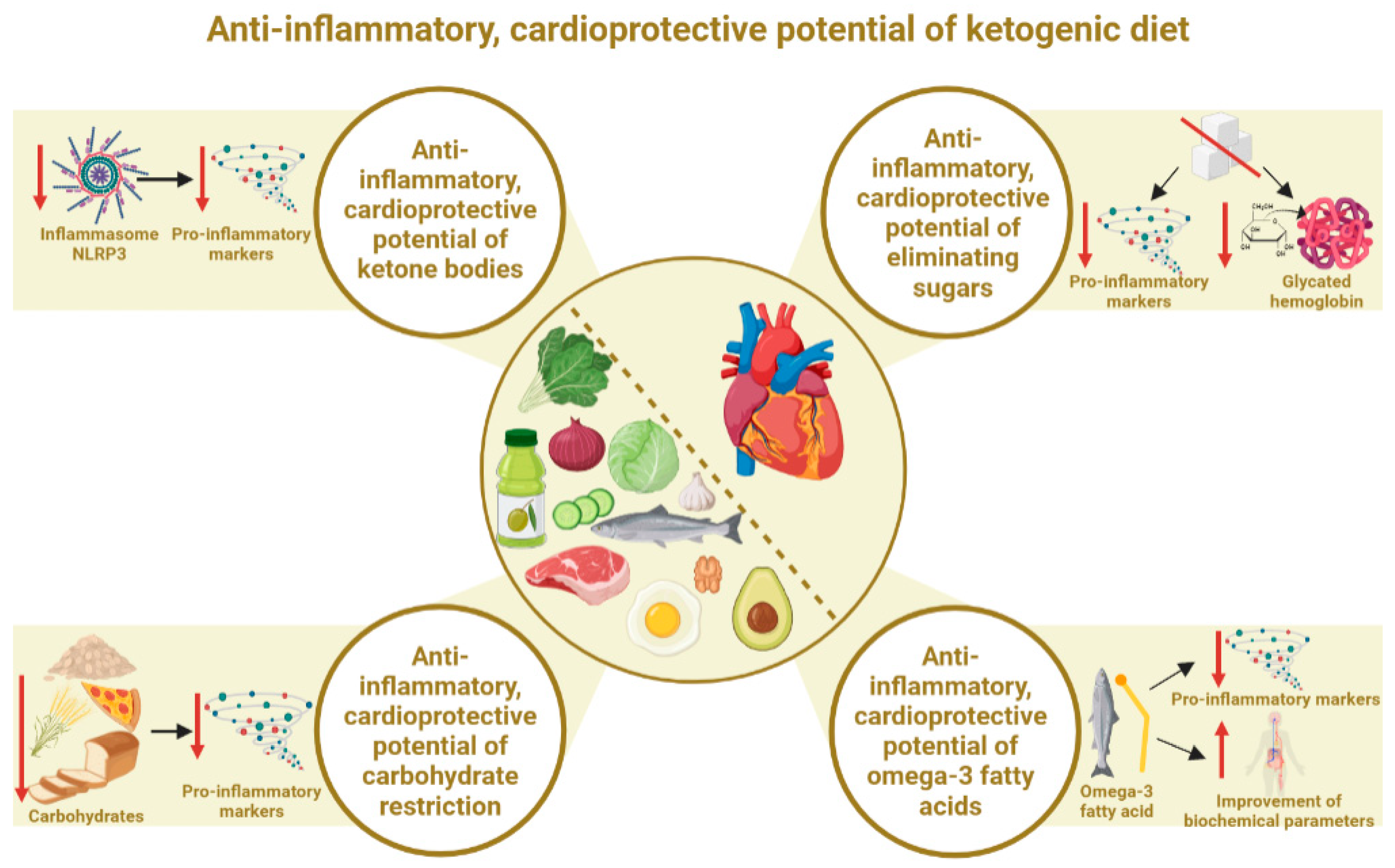
3.1. Anti-Inflammatory, Cardioprotective Potential of the State of Ketosis (Ketone Bodies)
3.2. Anti-Inflammatory, Cardioprotective Effects of Elimination of Simple Sugars
The ketogenic diet involves limiting the total supply of carbohydrates, most often to a maximum of 50 g per day. In view of this, simple sugars are marginalized and, in fact, can often even be considered to be completely eliminated. This is important to minimize frequent increases in serum glucose and insulin, which inhibit the achievement of the full desired state of ketosis [19,99][16][61]. It is well known that simple sugars are one of the key pro-inflammatory dietary factors [100[62][63][64],101,102], which applies mainly to all simple sugars (by the manufacturer, consumer or food preparer). Concerns about the negative effects of simple sugars on CVD date back to the 1960s [103][65]. At the same time, however, low-fat diets were promoted for the prevention of CVD. Increasing the proportion of carbohydrates (including simple sugars) in the diet consequently led to worsening parameters related to cardiovascular health. It was only decades later that this was proven not to be a useful approach in the fight against increasing heart disease [104,105,106,107,108,109][66][67][68][69][70][71]. Too much added sugar in the diet can be one of the greatest threats to cardiovascular health. It exacerbates chronic inflammation, increasing the risk of developing CVD [110][72]. It should be clearly noted that the source of simple sugars often plays an important role. Free sugars are the most pro-inflammatory (including fructose in the form of sugar sweetened beverages (SSB), not necessarily from fruit). Kelly et. al. showed that replacing 5% of the energy from free sugars with non-free sugars was associated with a lower risk of total CVD (0.95; 0.92–0.98; p-trend = 0.001) and total stroke (0.91; 0.86–0.97; p-trend = 0.005) [112][73]. Studies show that the simple sugars present in fruit are unlikely to have a pro-inflammatory effect. A diet rich in fruits and vegetables may even help to reduce inflammation as they are a rich source of antioxidants and other bioactive substances [113][74]. It is known that a diet with excess fructose is pro-inflammatory, increasing the risk of metabolic syndrome or gout. Elevated levels of fructose metabolites (including uric acid and lactate) are closely related to oxidative stress and local inflammatory reactions in tissues and organs [114,115][75][76]. Glycated hemoglobin (HbA1c), which reflects the average serum glucose concentration over the past 3 months, is also one of the most important CVD risk factors [119][77]. Importantly, high HbA1c levels are strongly associated with CVD risk in people both with and without diabetes [120,121][78][79]. HbA1c has been shown to be positively correlated with CVD, such as carotid and coronary atherosclerosis, ischemic heart disease, ischemic stroke and hypertension, among others. The author of the publication also points out that HbA1c causes dyslipidemia, hyperhomocysteinemia and hypertension. In addition, it increases C-reactive protein (CRP) levels, oxidative stress and blood viscosity. All of these may eventually lead to the development of CVD [122][80]. It appears that HbA1c is an independent risk factor for the development of CVD and death from these diseases, even in people without diabetes. This shows the remarkable relevance of this marker for the general population [121][79]. However, the ketogenic diet has been shown to have HbA1c-lowering properties, through which it can also benefit CVD prevention and therapy. The efficacy of KD in lowering HbA1c is supported by a number of meta-analyses and other publications.3.3. Anti-Inflammatory, Cardioprotective Effects of Total Carbohydrate Restriction
The beneficial above-mentioned effects of ketogenic diets on the values of inflammatory markers and CVD risk factors may also be due to the reduction of the total carbohydrate pool, not simply the elimination of simple sugars. This may be supported by an extensive meta-analysis from 2022, which did not look strictly at the ketogenic diet but precisely at the effect of reducing the percentage of carbohydrates in the diet. It examined the effect of reducing the percentage of energy from carbohydrates from 55–65% to 10% on cardiometabolic risk factors in people with type 2 diabetes mellitus (T2DM). It was shown that each 10% reduction in carbohydrate energy percentage reduced the HbA1c concentration (by an average of 0.20 HbA1c%), fasting blood glucose (by an average of 0.34 mmol/L), triglyceride concentration (by an average of 0.12 mmol), body weight (by an average of 1.44 kg) and even systolic blood pressure (by an average of 1.79 mmHg). These values decreased linearly with a decrease in carbohydrate intake from 55–65% to 10%. These results reflected a 6-month period. When the indices were rechecked 12 months after baseline, HbA1c values continued their linear downward trend (by an average of 0.11 HbA1c%), as did triglyceride levels (a reduction of 0.12 mmol on average) [127][81]. At the same time, a U-shaped effect was observed at 6 months of follow-up for total and LDL cholesterol, where the greatest benefits occurred when reducing the amount of carbohydrates to 40% of energy, and for body weight at 12 months of observation (greatest benefits at 35% of carbohydrates within total energy). It should be taken into account that the source of total carbohydrates itself is extremely important. Some studies do not take into account the source, while this certainly influences the subsequent results of the study. It is clear that a diet based on refined carbohydrates will be significantly worse compared to a diet based on unprocessed, whole grain carbohydrate sources. Given these relationships, in addition to achieving a state of ketosis and eliminating simple sugars, the ketogenic diet may also show beneficial anti-inflammatory cardioprotective potential as a result of limiting the total carbohydrate supply, especially if processed carbohydrates are subjected to this restriction.3.4. Anti-Inflammatory, Cardioprotective Effects of Omega-3 Fatty Acids
A properly composed ketogenic diet is abundant in anti-inflammatory fatty acids from the omega-3 group. In this respect, it may show an advantage over other diets, especially low-fat diets. This is because it is much easier to provide the correct amounts of fatty acids, as one of the main foods is oily fish (which is the main source of omega-3). It is a high-fat diet, so there is much less concern about exceeding the percentage of energy from fats than with other diets. Omega-3 fatty acids exhibit systemic anti-inflammatory effects, although, in the context of cardiovascular health, they are of particular importance. Indeed, it has been shown that omega-3 PUFAs, by competing with omega-6 PUFAs and displacing arachidonic acid in membrane phospholipids, exert anti-inflammatory properties by reducing the production of pro-inflammatory eicosanoids. Simonetto et al., in a publication, indicated that omega-3 PUFA supplementation may reduce the risk of various phenotypes of atherosclerosis and cardiovascular diseases [134][82]. A 2023 systematic review indicated and confirmed that omega-3 also improves the blood lipid profile [135][83]. The cardioprotective effect of omega-3 fatty acids is therefore firmly established in the literature and further confirmed by a number of recent publications, including meta-analyses [136,137,138,139,140][84][85][86][87][88].4. Ketone Bodies and Cardiac Energy Metabolism
The influence of the ketogenic diet on cardiac energy metabolism is increasingly being studied and described in scientific publications. This is due to the specific state of ketosis, in which there is increased induction of ketone body production. The main ketone body found in the blood, β-hydroxybutyrate, is seen to have the potential to affect myocardial metabolism and function. Of all the organs, the heart has the highest energy requirement. This is due to the need to work continuously, from fetal life until death. Thus, the cells of the heart muscle (cardiomyocytes) are characterized by the highest concentrations of mitochondria, i.e., “cellular power plants”, in the body. Indeed, mitochondria are the energy centers of the cells, as they are responsible for the production of energy in the form of adenosine triphosphate (ATP) [144,145][89][90]. It is known that in order to obtain ATP, the heart can use acetyl-coenzyme A (acetyl-CoA) from glucose (via glycolysis) or lipids (via β-oxidation). Under normal conditions, acetyl-CoA from fatty acids is the preferred substrate for ATP production in the heart. However, in patients with HFrEF, the contribution of ketone oxidation to myocardial ATP production increases from 6.4% (in control subjects) to 16.4% [146][91]. It appears that ketone bodies are therefore a very good, and, in many cases, perhaps better, energy substrate for the acquisition of ATP [97,147][92][93]. In the early stages of heart disease, the organ shifts its energy preference from fatty acids towards glucose, which is associated with a loss of metabolic flexibility [98,148][94][95]. However, it is still difficult to determine whether metabolic abnormalities occur due to the onset of heart disease or whether heart disease occurs as a result of metabolic abnormalities [149][96]. The fact is, however, that this eventually leads to heart failure, resulting in the further reprogramming of the heart’s metabolism towards the uptake and use of ketone bodies as an energy source. The fact that this may be an adaptive response offers a convincing argument for the relevance of ketone bodies to the metabolism of this organ. This is supported by a number of publications that show higher concentrations of ketone bodies and greater uptake of ketone bodies, among others, when heart failure occurs [150,151,152,153,154][97][98][99][100][101]. The heart prefers ketone bodies to glucose under conditions where both substrates are available. This was shown in a study by Gormsen et al., in which increasing the concentration of ketone bodies to 3.8 mM resulted in a 50% reduction in myocardial glucose uptake. This occurred despite maximal insulin stimulation and sufficient glucose [155][102]. It appears that the increased oxidation of ketone bodies is of particular use to the heart (and brain), as hyperketonemia does not affect glucose and fatty acid uptake in other organs [156,157][103][104].5. The Ketogenic Diet and the Vascular Endothelium
Endothelial cells are extremely important in maintaining the function of the cardiovascular system and, by extension, the whole body. They regulate vascular tone by, among other actions, producing nitric oxide, endothelin and prostaglandins. They produce and respond to various cytokines and adhesion molecules. In addition, they are key immunoreactive cells, and their dysfunction results in a number of pathological changes. In addition, they play an extremely important role in many other processes [176,177][105][106]. It appears that the ketogenic diet, via ketone bodies, can also affect endothelial cells. These cells are intimately involved in the transport of ketone bodies. Importantly, they are able to take them up and use them to generate biomass and ATP, as they express succinyl-CoA:3-oxoacid-CoA transferase (SCOT) (an enzyme that oxidizes ketone bodies). This was demonstrated in a 2022 publication showing that cardiac endothelial cells are capable of oxidizing ketone bodies, which increases proliferation, cell migration and vascular sprouting. Additionally, in a mouse model of cardiac hypertrophy, the ketogenic diet prevented vasodilation. In view of this, the ketogenic diet may play a beneficial role in heart disease [178][107]. The publication by Nasser et al. adds further evidence of the protective effect of ketone bodies. Ketone bodies (mainly BHB) in low concentrations (achievable with a ketogenic diet) have been shown to potentially improve endothelial and vascular function in metabolic disease. At the same time, excess ketone bodies resulting from diabetic ketoacidosis have been shown to affect diabetic vasculopathy and the vascular complications of diabetes [97][92]. However, diabetic ketoacidosis is known to occur with simultaneous excess concentrations of ketone bodies and glucose, with such high levels of ketone bodies not usually achievable through a ketogenic diet [19][16]. Unsurprisingly, diabetic patients experiencing ketoacidosis are at risk of not only vascular complications but even death from them [179,180,181][108][109][110]. However, ketone bodies in nutritional ketosis concentrations (induced by a ketogenic diet) exert direct beneficial effects on vascular endothelial modulation, showing anti-inflammatory effects in the endothelium, among others [97][92]. Gormsen et al. further demonstrated that hyperketonemia induced by Na-3-hydroxybutyrate infusion increased myocardial blood flow by up to 75% and heart rate by approximately 25%. The authors concluded that ketone bodies reduce myocardial glucose uptake and increase myocardial blood flow. They thus suggested that ketone bodies are important vasodilators and an important source of fuel for the heart. This affects the overall therapeutic potential of ketone bodies in CVD [155][102]. Another randomized controlled trial showed that the infusion of 3-hydroxybutyrate increased the cardiac minute volume by 2 L/min (40%), with an absolute improvement in the left ventricular ejection fraction (8%). Importantly, an effect on vasodilation was noted. This was accompanied by stable systemic and pulmonary pressure [167][111].6. The Ketogenic Diet and Blood Pressure
Taking into account the nature of the ketogenic diet, it seems reasonable to consider how this dietary intervention affects blood pressure. Indeed, there are several mechanisms by which it is able to affect this parameter. On the one hand, it is known that the ketogenic diet reduces insulin concentrations because it provides a low amount of carbohydrates [82][53]. Insulin, on the other hand, is responsible for the retention of sodium in the body by stimulating its reabsorption, and this is also related to the retention of water in the body. With a decrease in insulin concentrations, there is then the increased removal of water and sodium from the body [190,191][112][113]. This in turn leads to the removal of more of the other electrolytes, e.g., potassium, with the urine [192,193][114][115]. Magnesium or calcium may also decrease. However, it has been shown that electrolyte loss only occurs during the first period of the ketogenic diet (first week) and is due to natural adaptations to the state of ketosis [19,194,195][16][116][117]. It is known that adequate electrolyte levels are an essential factor in maintaining normal blood pressure [196][118]. On the other hand, it is also known that the vascular endothelium has an extremely important influence on blood pressure [197[119][120],198], which can be affected by the ketogenic diet. In addition, it may beneficially affect the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system (SNS) [199,200][121][122]. Another possible mechanism for the effect on blood pressure may include the effect of the ketogenic diet on the renin–angiotensin–aldosterone (RAA) system, as discussed in two publications from 2023 [201,202][123][124]. Weight loss is a significant, simple mechanism involved in the influence of the ketogenic diet on blood pressure. A caloric deficit used simultaneously with the ketogenic diet, and weight loss itself (and an improvement in body composition), can indirectly improve blood pressure parameters [203,204,205][125][126][127]. A number of potential mechanisms for the effects of the ketogenic diet on blood pressure make it worthwhile to consider publications examining actual blood pressure changes that have occurred in people using this dietary intervention. The authors of a 2021 publication indicate that the ketogenic diet is able to provide a reduction in blood pressure but does not produce significant changes compared to non-ketogenic diets. They also indicate that this is largely due to weight and fat loss and improvements in CVD risk parameters [203,204,205][125][126][127].7. The Ketogenic Diet and Weight Loss as a Factor in CVD Prevention and Therapy
The ketogenic calorie deficit diet is often used to reduce excess body weight. Taking into account its nature, for many people, it is a more effective weight loss strategy compared to standard diets. Taking into consideration that obesity is one of the primary risk factors for CVD, weight loss in itself will significantly reduce the risk of these diseases. Obesity, therefore, simultaneously is the effect of other risk factors, i.e., poor diet and physical inactivity, while at the same time being another risk factor on its own [1,6,59,213,214][2][3][128][129][130]. In addition, it affects other risk factors, e.g., dyslipidemia, hypertension, type 2 diabetes and sleep disorders, among others. Furthermore, an increased waist circumference can be considered as an independent risk factor for CVD, independent of BMI. Excessive visceral obesity is also an independent indicator and has been linked to poor cardiovascular outcomes. Losing excessive body weight thereby improves cardiovascular function, resulting in a reduction in CVD risk [215][131]. In addition to these mechanisms, the ketogenic diet improves CVD risk factors and, in addition, often reduces body weight (often the main reason for its use). Thus, it decreases the risk factor of obesity/overweight and, at the same time, nullifies other risk factors that arise from excess body weight. A meta-analysis by Bueno et al. showed that the ketogenic diet may be a more effective option for long-term weight loss (and improvements in some CVD risk factors), compared to low-fat diets [212][132]. The superiority of ketogenic diets over low-fat diets was also shown in a meta-analysis by Choi et al. It was shown that, compared to low-fat diets, the ketogenic diet was more effective in improving metabolic parameters related to, among other factors, body weight, lipid profile and glycemic control in patients with excess body weight (overweight or obesity), particularly in diabetic patients [125][133].8. The Effect of the Ketogenic Diet among Patients with CVD and Healthy People
Some studies often present greater benefits of the ketogenic diet among CVD patients than among healthy and often physically active people. These differences may be due to certain mechanisms. Firstly, people suffering from CVD frequently also have excessive body weight (which is much less common in healthy people), so a greater weight loss effect is observed among people affected by CVD. Additionally, it is known that weight loss alone provides a marked improvement in parameters related to CVD risk [215][131]. This is shown e.g., in publications by Li et. al, Schiavo et. al. and Michalczyk et. al., in which people using the ketogenic diet lost significantly more body weight compared to the control group, thus improving the values of parameters such as total cholesterol, LDL, HDL and triglycerides [43][32]. This aspect is described in more detail in Section 7. The other mechanism is the fact that people suffering from CVD have, by definition, an abnormal lipid profile, which is not present to such an extent in healthy and physically active people. An example is a study in which, in healthy, young and trained women, the ketogenic diet did not improve their lipid profiles, and the authors even concluded that it deteriorated [47][134], which is in opposition to a number of studies described (in Section 2.2) in which the ketogenic diet reduced CVD risk parameters among patients with and without overweight. Another argument for the greater benefits of the ketogenic diet among people suffering from or at risk of CVD is the composition of the current diet. The composition of the diet of these people is often inappropriate, particularly regarding the content of many processed products. A Western-style diet alone worsens CVD risk parameters, thereby increasing the risk of developing the disease. Therefore, the act of switching to an unprocessed diet (which, as a rule, should be a ketogenic diet) should reduce this risk. An example was given in a publication that compared the adoption of an unprocessed ketogenic diet to the continuation of a standard Western model of nutrition (which certainly had a significant impact on the body weight of the surveyed women and dysregulation of the lipid profile, insulin or glucose levels). Women who switched to a ketogenic diet showed significantly improvements in their overall health and CVD risk parameters [50][135].9. Conclusions
Summarizing the extensive scientific evidence, the ketogenic diet is a promising nutritional model in the context of cardiovascular disease prevention and therapy. Through its pleiotropic properties, it is able to influence the cardiovascular system on multiple levels. Scientific evidence mostly confirms its beneficial (even more beneficial compared to other diets) effects on the lipid profile and other CVD risk factors. However, there is a lack of strong evidence of the CVD risk from dyslipidemia due to the ketogenic diet. A potential advantage of the ketogenic diet is the strong anti-inflammatory effect that interacts with the cardioprotective properties. In addition, the effect on cardiomyocyte metabolism and the increased uptake of ketone bodies in cardiac disorders means that ketone bodies can be described as “rescue fuel” for the heart. The multifaceted effects of the ketogenic diet may also be confirmed by the effect of ketone bodies on the vascular endothelium, modulating vascular endothelial cells, improving their function or delaying their ageing. This also confirms the beneficial effect of the ketogenic diet on blood pressure values and other indirect CVD risk factors, i.e., reduction in excess body weight. A number of these factors contribute to the overall cardioprotective potential of the ketogenic diet in the prevention and treatment of cardiovascular diseases. This is confirmed by an increasing number of recent scientific studies.References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report from the American Heart Association. Circulation 2022, 145, e153–e639, Erratum in Circulation 2022, 146, e141.
- Available online: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on 4 March 2023).
- Available online: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/heart-disease-stroke.htm (accessed on 4 March 2023).
- Vancheri, F.; Longo, G.; Vancheri, E.; Henein, M.Y. MentalStress and Cardiovascular Health—Part I. J. Clin. Med. 2022, 11, 3353.
- Cosentino, N.; Campodonico, J.; Milazzo, V.; De Metrio, M.; Brambilla, M.; Camera, M.; Marenzi, G. Vitamin D and Cardiovascular Disease: Current Evidence and Future Perspectives. Nutrients 2021, 13, 3603.
- Muzaffar, R.; Khan, M.A.; Mushtaq, M.H.; Nasir, M.; Khan, A.; Haq, I.U.; Muhammad, J. Hyperhomocysteinemia as an Independent Risk Factor for Coronary Heart Disease. Comparison with Conventional Risk Factors. Braz. J. Biol. 2021, 83, e249104.
- Khan, M.S.; Saeedullah, A.; Andrews, S.C.; Iqbal, K.; Qadir, S.A.; Shahzad, B.; Ahmed, Z.; Shahzad, M. Adolescent Afghan Refugees Display a High Prevalence of Hyperhomocysteinemia and Associated Micronutrients Deficiencies Indicating an Enhanced Risk of Cardiovascular Disease in Later Life. Nutrients 2022, 14, 1751.
- Xiao, K.; Chen, Y.; Xiao, L.; Sun, H.; He, Z.; Huang, G.; Chen, L.; Xv, L.; Peng, L.; Li, J.; et al. The relationship between hyperhomocysteinemia and total coronary artery occlusion: A cross-sectional study from Southwest China. Coron. Artery Dis. 2023, 34, 138–145.
- Tyrovola, D.; Soulaidopoulos, S.; Tsioufis, C.; Lazaros, G. The Role of Nutrition in Cardiovascular Disease: Current Concepts and Trends. Nutrients 2023, 15, 1064.
- Kahleova, H.; Levin, S.; Barnard, N.D. Vegetarian Dietary Patterns and Cardiovascular Disease. Prog. Cardiovasc. Dis. 2018, 61, 54–61.
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, 596–646.
- Mitrou, P.N.; Kipnis, V.; Thiébaut, A.C.; Reedy, J.; Subar, A.F.; Wirfält, E.; Flood, A.; Mouw, T.; Hollenbeck, A.R.; Leitzmann, M.F.; et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH–AARP diet and health study. Arch. Intern. Med. 2007, 167, 2461–2468.
- Fung, T.T.; Rexrode, K.M.; Mantzoros, C.S.; Manson, J.E.; Willett, W.C.; Hu, F.B. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation 2009, 119, 1093–1100.
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco Mejia, S.; Rahelić, D.; Kahleová, H.; Salas-Salvadó, J.; Kendall, C.W.; Sievenpiper, J.L. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 338.
- Eckel, R.H.; Jakicic, J.M.; Ard, J.D.; de Jesus, J.M.; Miller, N.H.; Hubbard, V.S.; Lee, I.M.; Lichtenstein, A.H.; Loria, C.M.; Millen, B.E.; et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. J. Am. Coll. Cardiol. 2014, 63, 2960–2984.
- Wilson, J.; Lowery, R. The Ketogenic Bible; Victory Belt Publishing Inc.: Las Vegas, NV, USA, 2017; ISBN 13:978-1-628601-04-6.
- Gardner, C.D.; Vadiveloo, M.K.; Petersen, K.S.; Anderson, C.A.M.; Springfield, S.; Van Horn, L.; Khera, A.; Lamendola, C.; Mayo, S.M.; Joseph, J.J. American Heart Association Council on Lifestyle and Cardiometabolic Health. Popular Dietary Patterns: Alignment with American Heart Association 2021 Dietary Guidance: A Scientific Statement from the American Heart Association. Circulation 2023, 147, 1715–1730.
- Du, Z.; Qin, Y. Dyslipidemia and Cardiovascular Disease: Current Knowledge, Existing Challenges, and New Opportunities for Management Strategies. J. Clin. Med. 2023, 12, 363.
- Jung, E.; Kong, S.Y.; Ro, Y.S.; Ryu, H.H.; Shin, S.D. Serum Cholesterol Levels and Risk of Cardiovascular Death: A Systematic Review and a Dose-Response Meta-Analysis of Prospective Cohort Studies. Int. J. Environ. Res. Public Health 2022, 19, 8272.
- Dong, J.; Yang, S.; Zhuang, Q.; Sun, J.; Wei, P.; Zhao, X.; Chen, Y.; Chen, X.; Li, M.; Wei, L.; et al. The Associations of Lipid Profiles With Cardiovascular Diseases and Death in a 10-Year Prospective Cohort Study. Front. Cardiovasc. Med. 2021, 8, 745539.
- Yi, S.W.; Yi, J.J.; Ohrr, H. Total cholesterol and all-cause mortality by sex and age: A prospective cohort study among 12.8 million adults. Sci. Rep. 2019, 9, 1596.
- BHF-HEART STATS and WHO-MORTALITY (Adapted). Total Cholesterol Levels vs Mortality Data from 164 Countries, 2005. Available online: https://renegadewellness.files.wordpress.com/2011/02/cholesterol-mortality-chart.pdf (accessed on 23 July 2023).
- Borén, J.; Chapman, M.J.; Krauss, R.M.; Packard, C.J.; Bentzon, J.F.; Binder, C.J.; Daemen, M.J.; Demer, L.L.; Hegele, R.A.; Nicholls, S.J.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: Pathophysiological, genetic, and therapeutic insights: A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2020, 41, 2313–2330.
- Peng, K.M.; Li, X.; Wang, Z.; Li, M.M.; Yang, Y. Association of low-density lipoprotein cholesterol levels with the risk of mortality and cardiovascular events: A meta-analysis of cohort studies with 1,232,694 participants. Medicine 2022, 101, e32003.
- Bhargava, S.; de la Puente-Secades, S.; Schurgers, L.; Jankowski, J. Lipids and lipoproteins in cardiovascular diseases: A classification. Trends Endocrinol. Metab. 2022, 33, 409–423.
- Kim, Y.G.; Jeong, J.H.; Han, K.D.; Roh, S.Y.; Min, K.; Lee, H.S.; Choi, Y.Y.; Shim, J.; Choi, J.I.; Kim, Y.H. Association between low-density lipoprotein cholesterol and sudden cardiac arrest in people with diabetes mellitus. Cardiovasc. Diabetol. 2023, 22, 36.
- Rong, S.; Li, B.; Chen, L.; Sun, Y.; Du, Y.; Liu, B.; Robinson, J.G.; Bao, W. Association of Low-Density Lipoprotein Cholesterol Levels with More than 20-Year Risk of Cardiovascular and All-Cause Mortality in the General Population. J. Am. Heart Assoc. 2022, 11, e023690.
- Nicholls, S.J.; Nelson, A.J. HDL and cardiovascular disease. Pathology 2019, 51, 142–147.
- Trimarco, V.; Izzo, R.; Morisco, C.; Mone, P.; Virginia Manzi, M.; Falco, A.; Pacella, D.; Gallo, P.; Lembo, M.; Santulli, G.; et al. High HDL (High-Density Lipoprotein) Cholesterol Increases Cardiovascular Risk in Hypertensive Patients. Hypertension 2022, 79, 2355–2363.
- Cho, Y.K.; Jung, C.H. HDL-C and Cardiovascular Risk: You Don’t Need to Worry about Extremely High HDL-C Levels. J. Lipid Atheroscler. 2021, 10, 57–61.
- Farnier, M.; Zeller, M.; Masson, D.; Cottin, Y. Triglycerides and risk of atherosclerotic cardiovascular disease: An update. Arch Cardiovasc. Dis. 2021, 114, 132–139.
- Li, S.; Lin, G.; Chen, J.; Chen, Z.; Xu, F.; Zhu, F.; Zhang, J.; Yuan, S. The effect of periodic ketogenic diet on newly diagnosed overweight or obese patients with type 2 diabetes. BMC Endocr. Disord. 2022, 22, 34.
- Ravnskov, U.; de Lorgeril, M.; Diamond, D.M.; Hama, R.; Hamazaki, T.; Hammarskjöld, B.; Hynes, N.; Kendrick, M.; Langsjoen, P.H.; Mascitelli, L.; et al. LDL-C does not cause cardiovascular disease: A comprehensive review of the current literature. Expert Rev. Clin. Pharmacol. 2018, 11, 959–970.
- Ravnskov, U.; Diamond, D.M.; Hama, R.; Hamazaki, T.; Hammarskjöld, B.; Hynes, N.; Kendrick, M.; Langsjoen, P.H.; Malhotra, A.; Mascitelli, L.; et al. Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: A systematic review. BMJ Open 2016, 6, e010401.
- Ravnskov, U.; de Lorgeril, M.; Diamond, D.M.; Hama, R.; Hamazaki, T.; Hammarskjöld, B.; Harcombe, Z.; Kendrick, M.; Langsjoen, P.H.; McCully, K.S.; et al. The LDL paradox: Higher LDL-cholesterol is associated with greater longevity. Ann. Epidemiol. Public Health 2020, 3, 1040–1047.
- Sorriento, D.; Iaccarino, G. Inflammation and Cardiovascular Diseases: The Most Recent Findings. Int. J. Mol. Sci. 2019, 20, 3879.
- Fiordelisi, A.; Iaccarino, G.; Morisco, C.; Coscioni, E.; Sorriento, D. NFkappaB is a Key Player in the Crosstalk between Inflammation Cardiovascular Diseases. Int. J. Mol. Sci. 2019, 20, 1599.
- Liccardo, D.; Cannavo, A.; Spagnuolo, G.; Ferrara, N.; Cittadini, A.; Rengo, C.; Rengo, G. Periodontal Disease: A Risk Factor for Diabetes and Cardiovascular Disease. Int. J. Mol. Sci. 2019, 20, 1414.
- Mercurio, V.; Lobasso, A.; Barbieri, L.; Parrella, P.; Ciervo, D.; Liccardo, B.; Bonaduce, D.; Tocchetti, C.G.; De Paulis, A.; Rossi, F.W. Inflammatory, Serological and Vascular Determinants of Cardiovascular Disease in Systemic Lupus Erythematosus Patients. Int. J. Mol. Sci. 2019, 20, 2154.
- Varricchi, G.; Loffredo, S.; Borriello, F.; Pecoraro, A.; Rivellese, F.; Genovese, A.; Spadaro, G.; Marone, G. Superantigenic Activation of Human Cardiac Mast Cells. Int. J. Mol. Sci. 2019, 20, 1828.
- Brigant, B.; Metzinger-Le Meuth, V.; Rochette, J.; Metzinger, L. TRIMming down to TRIM37: Relevance to Inflammation, Cardiovascular Disorders, and Cancer in MULIBREY Nanism. Int. J. Mol. Sci. 2018, 20, 67.
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131.
- Henein, M.Y.; Vancheri, S.; Longo, G.; Vancheri, F. The Role of Inflammation in Cardiovascular Disease. Int. J. Mol. Sci. 2022, 23, 12906.
- Sklerov, M.; Dayan, E.; Browner, N. Functional neuroimaging of the central autonomic network: Recent developments and clinical implications. Clin. Auton. Res. 2019, 29, 555–566.
- Kraynak, T.E.; Marsland, A.L.; Gianaros, P.J. Neural Mechanisms Linking Emotion with Cardiovascular Disease. Curr. Cardiol. Rep. 2018, 20, 128.
- Muscatell, K.A.; Dedovic, K.; Slavich, G.M.; Jarcho, M.R.; Breen, E.C.; Bower, J.E.; Irwin, M.R.; Eisenberger, N.I. Greater amygdala activity and dorsomedial prefrontal–amygdala coupling are associated with enhanced inflammatory responses to stress. Brain Behav. Immun. 2015, 43, 46–53.
- Tracey, K.J. The inflammatory reflex. Nature 2002, 420, 853–859.
- Shah, S.M.; Meadows, J.L.; Burg, M.M.; Pfau, S.; Soufer, R. Effects of Psychological Stress on Vascular Physiology: Beyond the Current Imaging Signal. Curr. Cardiol. Rep. 2020, 22, 156.
- Tawakol, A.; Ishai, A.; Takx, R.A.P.; Figueroa, A.L.; Ali, A.; Kaiser, Y.; Truong, Q.A.; Solomon, C.J.E.; Calcagno, C.; Mani, V.; et al. Relation between resting amygdalar activity and cardiovascular events: A longitudinal and cohort study. Lancet 2017, 389, 834–845.
- Pondel, N.; Liśkiewicz, D.; Liśkiewicz, A. Dieta ketogeniczna–mechanizm działania i perspektywy zastosowania w terapii: Dane z badań klinicznych. Postępy Biochem. 2020, 66, 270–286.
- Dyńka, D.; Kowalcze, K.; Paziewska, A. The Role of Ketogenic Diet in the Treatment of Neurological Diseases. Nutrients 2022, 14, 5003.
- Hwang, C.Y.; Choe, W.; Yoon, K.-S.; Ha, J.; Kim, S.S.; Yeo, E.-J.; Kang, I. Molecular Mechanisms for Ketone Body Metabolism, Signaling Functions, and Therapeutic Potential in Cancer. Nutrients 2022, 14, 4932.
- Dyńka, D.; Kowalcze, K.; Ambrozkiewicz, F.; Paziewska, A. Effect of the Ketogenic Diet on the Prophylaxis and Treatment of Diabetes Mellitus: A Review of the Meta-Analyses and Clinical Trials. Nutrients 2023, 15, 500.
- Kong, C.; Yan, X.; Liu, Y.; Huang, L.; Zhu, Y.; He, J.; Gao, R.; Kalady, M.F.; Goel, A.; Qin, H.; et al. Ketogenic diet alleviates colitis by reduction of colonic group 3 innate lymphoid cells through altering gut microbiome. Signal Transduct. Target. Ther. 2021, 6, 154.
- Field, R.; Pourkazemi, F.; Rooney, K. Effects of a Low-Carbohydrate Ketogenic Diet on Reported Pain, Blood Biomarkers and Quality of Life in Patients with Chronic Pain: A Pilot Randomized Clinical Trial. Pain Med. 2022, 23, 326–338.
- Alkhorayef, N.; Almutery, F.T.; Rasheed, Z.; Althwab, S.A.; Aljohani, A.S.M.; Alhawday, Y.A.N.; Salem, T.; Alharbi, A.M.; Wahaq, A.A.A.B.; Alharbi, F.S.; et al. Regulatory effects of ketogenic diet on the inflammatory response in obese Saudi women. J. Taibah Univ. Med. Sci. 2023, 18, 1101–1107.
- Mohammadifard, N.; Haghighatdoost, F.; Rahimlou, M.; Rodrigues, A.P.S.; Gaskarei, M.K.; Okhovat, P.; de Oliveira, C.; Silveira, E.A.; Sarrafzadegan, N. The Effect of Ketogenic Diet on Shared Risk Factors of Cardiovascular Disease and Cancer. Nutrients 2022, 14, 3499.
- Mezzaroma, E.; Toldo, S.; Farkas, D.; Seropian, I.M.; Van Tassell, B.W.; Salloum, F.N.; Kannan, H.R.; Menna, A.C.; Voelkel, N.F.; Abbate, A. The inflammasome promotes adverse cardiac remodeling following acute myocardial infarction in the mouse. Proc. Natl. Acad. Sci. USA 2011, 108, 19725–19730.
- Tong, Y.; Wang, Z.; Cai, L.; Lin, L.; Liu, J.; Cheng, J. NLRP3 Inflammasome and Its Central Role in the Cardiovascular Diseases. Oxid. Med. Cell. Longev. 2020, 2020, 4293206.
- Zheng, Y.; Xu, L.; Dong, N.; Li, F. NLRP3 inflammasome: The rising star in cardiovascular diseases. Front. Cardiovasc. Med. 2022, 9, 927061.
- Westman, E.C.; Feinman, R.D.; Mavropoulos, J.C.; Vernon, M.C.; Volek, J.S.; Wortman, J.A.; Yancy, W.S.; Phinney, S.D. Lowcarbohydrate nutrition and metabolism. Am. J. Clin. Nutr. 2007, 86, 276–284.
- Ma, X.; Nan, F.; Liang, H.; Shu, P.; Fan, X.; Song, X.; Hou, Y.; Zhang, D. Excessive intake of sugar: An accomplice of inflammation. Front. Immunol. 2022, 13, 988481.
- Della Corte, K.W.; Perrar, I.; Penczynski, K.J.; Schwingshackl, L.; Herder, C.; Buyken, A.E. Effect of Dietary Sugar Intake on Biomarkers of Subclinical Inflammation: A Systematic Review and Meta-Analysis of Intervention Studies. Nutrients 2018, 10, 606.
- O’Connor, L.; Imamura, F.; Brage, S.; Griffin, S.J.; Wareham, N.J.; Forouhi, N.G. Intakes and sources of dietary sugars and their association with metabolic and inflammatory markers. Clin. Nutr. 2018, 37, 1313–1322.
- McGandy, R.B.; Hegsted, D.M.; Stare, F.J. Dietary fats, carbohydratesand atherosclerotic vascular disease. N. Engl. J. Med. 1967, 277, 186–192.
- Carbone, S.; Billingsley, H.E.; Lavie, C.J. The Effects of Dietary Sugars on Cardiovascular Disease and Cardiovascular Disease-Related Mortality: Finding the Sweet Spot. Mayo Clin. Proc. 2019, 94, 2375–2377.
- Howard, B.V.; Van Horn, L.; Hsia, J.; Manson, J.E.; Stefanick, M.L.; Wassertheil-Smoller, S.; Kuller, L.H.; LaCroix, A.Z.; Langer, L.D.; Lasser, N.L.; et al. Low-fat dietary patternand risk of cardiovascular disease: The Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006, 295, 655–666.
- Billingsley, H.E.; Carbone, S.; Lavie, C.J. Dietary fats and chronicnoncommunicable diseases. Nutrients 2018, 10, 1385.
- Huang, C.; Huang, J.; Tian, Y.; Yang, X.; Gu, D. Sugar sweetened beverages consumption and risk of coronary heart disease: A metaanalysis of prospective studies. Atherosclerosis 2014, 234, 11–16.
- Li, Y.; Hruby, A.; Bernstein, A.M.; Ley, S.H.; Wang, D.D.; Chiuve, S.E.; Sampson, L.; Rexrode, K.M.; Rimm, E.B.; Willett, W.C.; et al. Saturated fats comparedwith unsaturated fats and sources of carbohydrates in relationto risk of coronary heart disease: A prospective cohort study. J. Am. Coll. Cardiol. 2015, 66, 1538–1548.
- Yang, Q.; Zhang, Z.; Gregg, E.W.; Flanders, W.D.; Merritt, R.; Hu, F.B. Added sugar intake and cardiovascular diseases mortalityamong US adults. JAMA Intern. Med. 2014, 174, 516–524.
- Available online: https://www.health.harvard.edu/heart-health/the-sweet-danger-of-sugar (accessed on 23 July 2023).
- Kelly, R.K.; Tong, T.Y.N.; Watling, C.Z.; Reynolds, A.; Piernas, C.; Schmidt, J.A.; Papier, K.; Carter, J.L.; Key, T.J.; Perez-Cornago, A. Associations between types and sources of dietary carbohydrates and cardiovascular disease risk: A prospective cohort study of UK Biobank participants. BMC Med. 2023, 21, 34.
- Hosseini, B.; Berthon, B.S.; Saedisomeolia, A.; Starkey, M.R.; Collison, A.; Wark, P.A.B.; Wood, L.G. Effects of fruit and vegetable consumption on inflammatory biomarkers and immune cell populations: A systematic literature review and meta-analysis. Am. J. Clin. Nutr. 2018, 108, 136–155.
- Cheng, H.; Zhou, J.; Sun, Y.; Zhan, Q.; Zhang, D. High fructose diet: A risk factor for immune system dysregulation. Hum. Immunol. 2022, 83, 538–546.
- Lubawy, M.; Formanowicz, D. High-Fructose Diet–Induced Hyperuricemia Accompanying Metabolic Syndrome–Mechanisms and Dietary Therapy Proposals. Int. J. Environ. Res. Public Health 2023, 20, 3596.
- Rawal, G.; Yadav, S.; Kumar, R.; Singh, A. Glycosylated hemoglobin (HbA1C): A brief overview for clinicians. IP Indian J. Immunol. Respir. Med. 2016, 1, 33–36.
- Goto, A.; Noda, M.; Matsushita, Y.; Goto, M.; Kato, M.; Isogawa, A.; Takahashi, Y.; Kurotani, K.; Oba, S.; Nanri, A.; et al. JPHC Study Group. Hemoglobin a1c levels and the risk of cardiovascular disease in people without known diabetes: A population-based cohort study in Japan. Medicine 2015, 94, e785.
- Sinning, C.; Makarova, N.; Völzke, H.; Schnabel, R.B.; Ojeda, F.; Dörr, M.; Felix, S.B.; Koenig, W.; Peters, A.; Rathmann, W.; et al. Association of glycated hemoglobin A1c levels with cardiovascular outcomes in the general population: Results from the BiomarCaRE (Biomarker for Cardiovascular Risk Assessment in Europe) consortium. Cardiovasc. Diabetol. 2021, 20, 223.
- Prasad, K. Does HbA1cc Play a Role in the Development of Cardiovascular Diseases? Curr. Pharm. Des. 2018, 24, 2876–2882.
- Jayedi, A.; Zeraattalab-Motlagh, S.; Jabbarzadeh, B.; Hosseini, Y.; Jibril, A.T.; Shahinfar, H.; Mirrafiei, A.; Hosseini, F.; Bidar, S.S. Dose-dependent effect of carbohydrate restriction for type 2 diabetes management: A systematic review and dose-response meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2022, 116, 40–56.
- Simonetto, M.; Infante, M.; Sacco, R.L.; Rundek, T.; Della-Morte, D. A Novel Anti-Inflammatory Role of Omega-3 PUFAs in Prevention and Treatment of Atherosclerosis and Vascular Cognitive Impairment and Dementia. Nutrients 2019, 11, 2279.
- Liu, Y.-X.; Yu, J.-H.; Sun, J.-H.; Ma, W.-Q.; Wang, J.-J.; Sun, G.-J. Effects of Omega-3 Fatty Acids Supplementation on Serum Lipid Profile and Blood Pressure in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Foods 2023, 12, 725.
- Rodriguez, D.; Lavie, C.J.; Elagizi, A.; Milani, R.V. Update on Omega-3 Polyunsaturated Fatty Acids on Cardiovascular Health. Nutrients 2022, 14, 5146.
- Fatahi, S.; Sohouli, M.H.; da Silva Magalhães, E.I.; da Cruz Silveira, V.N.; Zanghelini, F.; Rahmani, P.; Kord-Varkaneh, H.; Sharifi-Zahabi, E.; Shidfar, F. Comparing the effects of docosahexaenoic and eicosapentaenoic acids on cardiovascular risk factors: Pairwise and network meta-analyses of randomized controlled trials. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 11–21.
- Yang, B.; Tseng, P.T.; Hu, X.; Zeng, B.Y.; Chang, J.P.; Liu, Y.; Chu, W.J.; Zhang, S.S.; Zhou, Z.L.; Chu, C.S.; et al. Comparative efficacy of omega-3 polyunsaturated fatty acids on major cardiovascular events: A network meta-analysis of randomized controlled trials. Prog. Lipid Res. 2022, 88, 101196, Erratum in Prog. Lipid Res. 2022, 101206.
- Yokoyama, Y.; Kuno, T.; Morita, S.X.; Slipczuk, L.; Takagi, H.; Briasoulis, A.; Latib, A.; Bangalore, S.; Heffron, S.P. Eicosapentaenoic Acid for Cardiovascular Events Reduction- Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. J. Cardiol. 2022, 80, 416–422.
- Jiang, H.; Wang, L.; Wang, D.; Yan, N.; Li, C.; Wu, M.; Wang, F.; Mi, B.; Chen, F.; Jia, W.; et al. Omega-3 polyunsaturated fatty acid biomarkers and risk of type 2 diabetes, cardiovascular disease, cancer, and mortality. Clin. Nutr. 2022, 41, 1798–1807.
- Stoll, S.; Leimena, C.; Qiu, H. Mitochondria and Heart Disease; InTech: London, UK, 2018.
- Brown, D.A.; Perry, J.B.; Allen, M.E.; Sabbah, H.N.; Stauffer, B.L.; Shaikh, S.R.; Cleland, J.G.F.; Colucci, W.S.; Butler, J.; Voors, A.A.; et al. Expert consensus document: Mitochondrial function as a therapeutictarget in heart failure. Nat. Rev. Cardiol. 2017, 14, 238–250. Available online: https://www.researchgate.net/publication/327299198_Mitochondria_and_Heart_Disease (accessed on 24 April 2023).
- Murashige, D.; Jang, C.; Neinast, M.; Edwards, J.J.; Cowan, A.; Hyman, M.C.; Rabinowitz, J.D.; Frankel, D.S.; Arany, Z. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science 2020, 370, 364–368.
- Nasser, S.; Vialichka, V.; Biesiekierska, M.; Balcerczyk, A.; Pirola, L. Effects of ketogenic diet and ketone bodies on the cardiovascular system: Concentration matters. World J. Diabetes 2020, 11, 584–595.
- Abdul Kadir, A.; Clarke, K.; Evans, R.D. Cardiac ketone body metabolism. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165739.
- Yurista, S.R.; Chong, C.R.; Badimon, J.J.; Kelly, D.P.; de Boer, R.A.; Westenbrink, B.D. Therapeutic Potential of Ketone Bodies for Patients with Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 77, 1660–1669.
- Sack, M.N.; Rader, T.A.; Park, S.; Bastin, J.; McCune, S.A.; Kelly, D.P. Fatty acid oxidation enzyme gene expression is downregulated in the failing heart. Circulation 1996, 94, 2837–2842.
- Carley, A.N.; Taegtmeyer, H.; Lewandowski, E.D. Matrix revisited: Mechanisms linking energy substrate metabolism to the function of the heart. Circ. Res. 2014, 114, 717–729.
- Horton, J.L.; Davidson, M.T.; Kurishima, C.; Vega, R.B.; Powers, J.C.; Matsuura, T.R.; Petucci, C.; Lewandowski, E.D.; Crawford, P.A.; Muoio, D.M.; et al. The failing heart utilizes 3-hydroxybutyrate as a metabolic stress defense. JCI Insight 2019, 4, e124079.
- Bedi, K.C.; Snyder, N.W.; Brandimarto, J.; Aziz, M.; Mesaros, C.; Worth, A.J.; Wang, L.L.; Javaheri, A.; Blair, I.A.; Margulies, K.B.; et al. Evidence for intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation 2016, 133, 706–716.
- Aubert, G.; Martin, O.J.; Horton, J.L.; Lai, L.; Vega, R.B.; Leone, T.C.; Koves, T.; Gardell, S.J.; Krüger, M.; Hoppel, C.L.; et al. The Failing Heart Relies on Ketone Bodies as a Fuel. Circulation 2016, 133, 698–705.
- Lommi, M.D.J. Blood ketone bodies in congestive heart failure. J. Am. Coll. Cardiol. 1996, 28, 665–672.
- Voros, G.; Ector, J.; Garweg, C.; Droogne, W.; Van Cleemput, J.; Peersman, N.; Vermeersch, P.; Janssens, S. Increased cardiac uptake of ketone bodies and free fatty acids in human heart failure and hypertrophic left ventricular remodeling. Circ. Heart Fail. 2018, 11, e004953.
- Gormsen, L.C.; Svart, M.; Thomsen, H.H.; Sondergaard, E.; Vendelbo, M.H.; Chris-tensen, N.; Tolbod, L.P.; Harms, H.J.; Nielsen, R.; Wiggers, H.; et al. Ketone Body Infusion with 3-Hydroxybutyrate Reduces Myocardial Glucose Uptake and Increases Blood Flow in Humans: A Positron Emission Tomography Study. J. Am. Heart Assoc. 2017, 6, e005066.
- Svart, M.; Gormsen, L.C.; Hansen, J.; Zeidler, D.; Gejl, M.; Vang, K.; Aanerud, J.; Moeller, N. Regional cerebral effects of ketone body infusion with 3-hydroxybutyrate in humans: Reduced glucose uptake, unchanged oxygen consumption and increased blood flow by positron emission tomography. A randomized, controlled trial. PLoS ONE 2018, 13, e0190556.
- Lauritsen, K.M.; Søndergaard, E.; Luong, T.V.; Møller, N.; Gormsen, L.C. Acute Hyperketonemia Does Not Affect Glucose or Palmitate Uptake in Abdominal Organs or Skeletal Muscle. J. Clin. Endocrinol. Metab. 2020, 105, 1785–1790.
- Galley, H.F.; Webster, N.R. Physiology of the endothelium. Br. J. Anaesth. 2004, 93, 105–113.
- Nappi, F.; Fiore, A.; Masiglat, J.; Cavuoti, T.; Romandini, M.; Nappi, P.; Avtaar Singh, S.S.; Couetil, J.-P. Endothelium-Derived Relaxing Factors and Endothelial Function: A Systematic Review. Biomedicines 2022, 10, 2884.
- Weis, E.M.; Puchalska, P.; Nelson, A.B.; Taylor, J.; Moll, I.; Hasan, S.S.; Dewenter, M.; Hagenmüller, M.; Fleming, T.; Poschet, G.; et al. Ketone body oxidation increases cardiac endothelial cell proliferation. EMBO Mol. Med. 2022, 14, e14753.
- Devaraj, S.; Cheung, A.T.; Jialal, I.; Griffen, S.C.; Nguyen, D.; Glaser, N.; Aoki, T. Evidence of increased inflammation and microcirculatory abnormalities in patients with type 1 diabetes and their role inmicrovascular complications. Diabetes 2007, 56, 2790–2796.
- White, N.H. Diabetic ketoacidosis in children. Endocrinol. Metab. Clin. North Am. 2000, 29, 657–682.
- Bialo, S.R.; Agrawal, S.; Boney, C.M.; Quintos, J.B. Rare complications of pediatric diabetic ketoacidosis. World J. Diabetes 2015, 6, 167–174.
- Nielsen, R.; Møller, N.; Gormsen, L.C.; Tolbod, L.P.; Hansson, N.H.; Sorensen, J.; Harms, H.J.; Frøkiær, J.; Eiskjaer, H.; Jespersen, N.R.; et al. Cardiovascular Effects of Treatment With the Ketone Body 3-Hydroxybutyrate in Chronic Heart Failure Patients. Circulation 2019, 139, 2129–2141.
- DeFronzo, R.A. The effect of insulin on renal sodium metabolism. A review with clinical implications. Diabetologia 1981, 21, 165–171.
- Brands, M.W. Role of Insulin-Mediated Antinatriuresis in Sodium Homeostasis and Hypertension. Hypertension 2018, 72, 1255–1262.
- Palmer, B.F.; Clegg, D.J. Physiology and pathophysiology of potassium homeostasis. Adv. Physiol. Educ. 2016, 40, 480–490.
- Harvey, C.J.D.C.; Schofield, G.M.; Williden, M. The use of nutritional supplements to induce ketosis and reduce symptomsassociated with keto-induction: A narrative review. PeerJ 2018, 6, e4488.
- Zupec-Kania, B.; Zupanc, M.L. Long-term management of the ketogenic diet: Seizure monitoring, nutrition, and supplementation. Epilepsia 2008, 49 (Suppl. S8), 23–26.
- Cordain, L. Nutritional Deficiencies of Ketogenic Diets. 2018. Available online: https://www.researchgate.net/publication/332098774_Nutritional_Deficiencies_of_Ketogenic_Diets?channel=doi&linkId=5c9f99e2a6fdccd46045868c&showFulltext=true (accessed on 23 July 2023). License CC BY-NC-ND 4.0.
- Iqbal, S.; Klammer, N.; Ekmekcioglu, C. The Effect of Electrolytes on Blood Pressure: A Brief Summary of Meta-Analyses. Nutrients 2019, 11, 1362.
- Gallo, G.; Volpe, M.; Savoia, C. Endothelial Dysfunction in Hypertension: Current Concepts and Clinical Implications. Front. Med. 2021, 8, 798958.
- Kostov, K. The Causal Relationship between Endothelin-1 and Hypertension: Focusing on Endothelial Dysfunction, Arterial Stiffness, Vascular Remodeling, and Blood Pressure Regulation. Life 2021, 11, 986.
- Polito, R.; Messina, G.; Valenzano, A.; Scarinci, A.; Villano, I.; Monda, M.; Cibelli, G.; Porro, C.; Pisanelli, D.; Monda, V.; et al. The Role of Very Low Calorie Ketogenic Diet in Sympathetic Activation through Cortisol Secretion in Male Obese Population. J. Clin. Med. 2021, 10, 4230.
- Polito, R.; Valenzano, A.; Monda, V.; Cibelli, G.; Monda, M.; Messina, G.; Villano, I.; Messina, A. Heart Rate Variability and Sympathetic Activity Is Modulated by Very Low-Calorie Ketogenic Diet. Int. J. Environ. Res. Public Health 2022, 19, 2253.
- Barrea, L.; Verde, L.; Camajani, E.; Šojat, A.S.; Marina, L.; Savastano, S.; Colao, A.; Caprio, M.; Muscogiuri, G. Effects of very low-calorie ketogenic diet on hypothalamic–pituitary–adrenal axis and renin–angiotensin–aldosterone system. J. Endocrinol. Investig. 2023, 46, 1509–1520.
- Belany, P.; Kackley, M.L.; Zhao, S.; Kluwe, B.; Buga, A.; Crabtree, C.D.; Nedungadi, D.; Kline, D.; Brock, G.; Simonetti, O.P.; et al. Effects of Hypocaloric Low-Fat, Ketogenic, and Ketogenic and Ketone Supplement Diets on Aldosterone and Renin. J. Clin. Endocrinol. Metab. 2023, 108, 1727–1739.
- Di Raimondo, D.; Buscemi, S.; Musiari, G.; Rizzo, G.; Pirera, E.; Corleo, D.; Pinto, A.; Tuttolomondo, A. Ketogenic Diet, Physical Activity, and Hypertension—A Narrative Review. Nutrients 2021, 13, 2567.
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Tas k Force for the Management of Arterial Hypertension. J. Hypertens. 2018, 36, 2284–2309.
- Di Raimondo, D.; Musiari, G.; Miceli, G.; Arnao, V.; Pinto, A. Preventive and Therapeutic Role of Muscle Contraction against Chronic Diseases. Curr. Pharm. Des. 2016, 22, 4686–4699.
- Muscogiuri, G.; El Ghoch, M.; Colao, A.; Hassapidou, M.; Yumuk, V.; Busetto, L. Obesity Management Task Force (OMTF) of the European Association for the Study of Obesity (EASO). European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes. Facts. 2021, 14, 222–245.
- Markovikj, G.; Knights, V.; Kljusurić, J.G. Ketogenic Diet Applied in Weight Reduction of Overweight and Obese Individuals with Progress Prediction by Use of the Modified Wishnofsky Equation. Nutrients 2023, 15, 927.
- Muscogiuri, G.; Barrea, L.; Laudisio, D.; Pugliese, G.; Salzano, C.; Savastano, S.; Colao, A. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J. Transl. Med. 2019, 17, 356.
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010.
- Bueno, N.; De Melo, I.; De Oliveira, S.; Da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2013, 110, 1178–1187.
- Choi, Y.J.; Jeon, S.M.; Shin, S. Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2020, 12, 2005.
- Burén, J.; Ericsson, M.; Damasceno, N.R.T.; Sjödin, A. A Ketogenic Low-Carbohydrate High-Fat Diet Increases LDL Cholesterol in Healthy, Young, Normal-Weight Women: A Randomized Controlled Feeding Trial. Nutrients 2021, 13, 814.
- Michalczyk, M.M.; Klonek, G.; Maszczyk, A.; Zajac, A. The Effects of a Low Calorie Ketogenic Diet on Glycaemic Control Variables in Hyperinsulinemic Overweight/Obese Females. Nutrients 2020, 12, 1854.
