Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Carolina Vieira De Almeida and Version 2 by Lindsay Dong.
The skin microbiota is a pivotal contributor to the maintenance of skin homeostasis by protecting it from harmful pathogens and regulating the immune system. An imbalance in the skin microbiota can lead to pathological conditions such as eczema, psoriasis, and acne. This imbalance can be triggered by different elements and dynamics such as changes in pH levels, exposure to environmental toxins, and the use of certain skincare products. Some research suggests that certain probiotic strains and their metabolites (postbiotics) may provide benefits such as improving the skin barrier function, reducing inflammation, and improving the appearance of acne-prone or eczema-prone skin.
- postbiotics
- probiotics
- skin
- skincare
1. Introduction
The last decade has seen an explosion in microbiota research, which has enabled a better understanding of its structure and function, leading to potential opportunities to develop next-generation microbiome-based drugs and diagnostic biomarkers. These studies have demonstrated that trillions of microbes live within our bodies in a deeply symbiotic relationship. They have provided evidence that microbial populations vary across body sites, driven by differences in the environment, immunological factors, and interactions between microbial species [1]. To better understand the function of the microbiome, it is fundamental to consider how microbes that live on body superficies can influence systemic performances.
The skin is the primary physical barrier that protects our bodies from potential invasion by pathogens or toxic substances, but skin does not act alone: microorganisms that live in symbiosis with us and occupy a broad array of skin niches help to protect our body against harmful situations. Microorganisms from the skin can act directly to defend the host against pathogens, control inflammation, and modulate the adaptive immune pathways [2][3][4][2,3,4].
 The skin is also known as ‘acid mantle’ [7], and consists of a lipid- and protein-laden cornified layer dotted with hair follicles and glands that secrete lipids, antimicrobial peptides (AMPs), enzymes, salts, and many other compounds. Over the SC, the pH is gradual, but in general, the natural skin surface, when in good conditions, presents an average pH below 5.0. This acidity is essential to maintain the balance of skin microbiota, as well as to support important physiological processes, such as the formation of the lipid barrier and SC homeostasis. In addition, the skin surface is a high salt, desiccated, and aerobic environment [2][8][9][2,8,9]. These odd characteristics of the skin surface make the skin physically and chemically distinct from another microbe-rich barrier sites such as the small and large intestines which are characterized by a polysaccharide-rich [10] and neutral pH surface [11].
Because it is always exposed to possible pathogens and is subject to sterile inflammation, comprising tumor immunity, allergy, and autoimmune responses, an appropriate functioning of skin defense based on complex action of a variety of complementary systems is fundamental. Complementary to the physical barrier, there is an active synthesis of gene-encoded host defense molecules such as proteases, lysozymes, antimicrobial peptides (AMPs), cytokines, and chemokines that serve as activators of the cellular and adaptive immune responses [2].
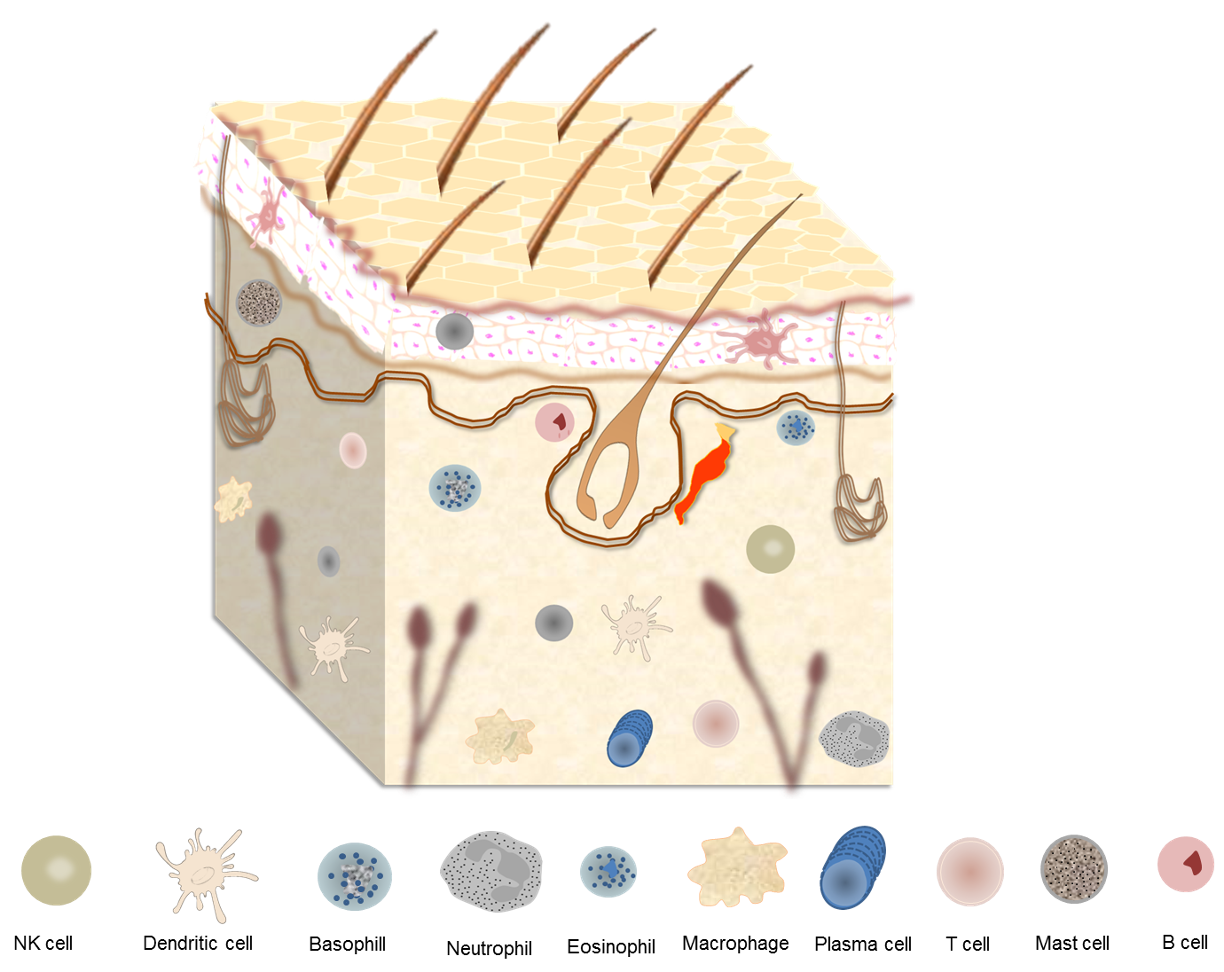
Maintenance of skin homeostasis upon inflammatory challenges requires various types of immune cells that are resident in skin or are recruited (Figure 1). For instance, in the epidermis, keratinocytes produce AMPs that exhibit direct bacteriostatic or bactericidal activity, promoting the recruitment of immune cells such as Langerhans cells (LCs) [4]. These cells are a subset of tissue-resident macrophages that reside between keratinocytes and, upon further differentiation, acquire dendritic cell (DC)-like phenotype and functions [12]. On the other hand, in the dermis, several types of innate immune cells, including dermal DCs, macrophages, mast cells, γδ T cells, and innate lymphoid cells (ILCs) are found [13].
The skin is also known as ‘acid mantle’ [7], and consists of a lipid- and protein-laden cornified layer dotted with hair follicles and glands that secrete lipids, antimicrobial peptides (AMPs), enzymes, salts, and many other compounds. Over the SC, the pH is gradual, but in general, the natural skin surface, when in good conditions, presents an average pH below 5.0. This acidity is essential to maintain the balance of skin microbiota, as well as to support important physiological processes, such as the formation of the lipid barrier and SC homeostasis. In addition, the skin surface is a high salt, desiccated, and aerobic environment [2][8][9][2,8,9]. These odd characteristics of the skin surface make the skin physically and chemically distinct from another microbe-rich barrier sites such as the small and large intestines which are characterized by a polysaccharide-rich [10] and neutral pH surface [11].
Because it is always exposed to possible pathogens and is subject to sterile inflammation, comprising tumor immunity, allergy, and autoimmune responses, an appropriate functioning of skin defense based on complex action of a variety of complementary systems is fundamental. Complementary to the physical barrier, there is an active synthesis of gene-encoded host defense molecules such as proteases, lysozymes, antimicrobial peptides (AMPs), cytokines, and chemokines that serve as activators of the cellular and adaptive immune responses [2].
Maintenance of skin homeostasis upon inflammatory challenges requires various types of immune cells that are resident in skin or are recruited (Figure 1). For instance, in the epidermis, keratinocytes produce AMPs that exhibit direct bacteriostatic or bactericidal activity, promoting the recruitment of immune cells such as Langerhans cells (LCs) [4]. These cells are a subset of tissue-resident macrophages that reside between keratinocytes and, upon further differentiation, acquire dendritic cell (DC)-like phenotype and functions [12]. On the other hand, in the dermis, several types of innate immune cells, including dermal DCs, macrophages, mast cells, γδ T cells, and innate lymphoid cells (ILCs) are found [13].
2. The Skin
The human skin comprises a variety of unique and uneven regions, with lines, ridges, and invaginations from skin appendages unevenly distributed over its surface (Figure 1). The outermost layer of epidermis is the stratum corneum (SC), which consists of piles of dead keratinocytes (corneocytes) and intercellular lipids. Due to a specific and unique type of functional cell death named corneoptosis, keratinocytes are converted into corneocytes, which remain functional in the SC and act as a functional barriers. This barriers protect the body against mechanical stresses, dehydration, toxic substances, and pathogen invasion, enabling terrestrial vertebrates succeed survive in nonaquatic environments [5][6][5,6].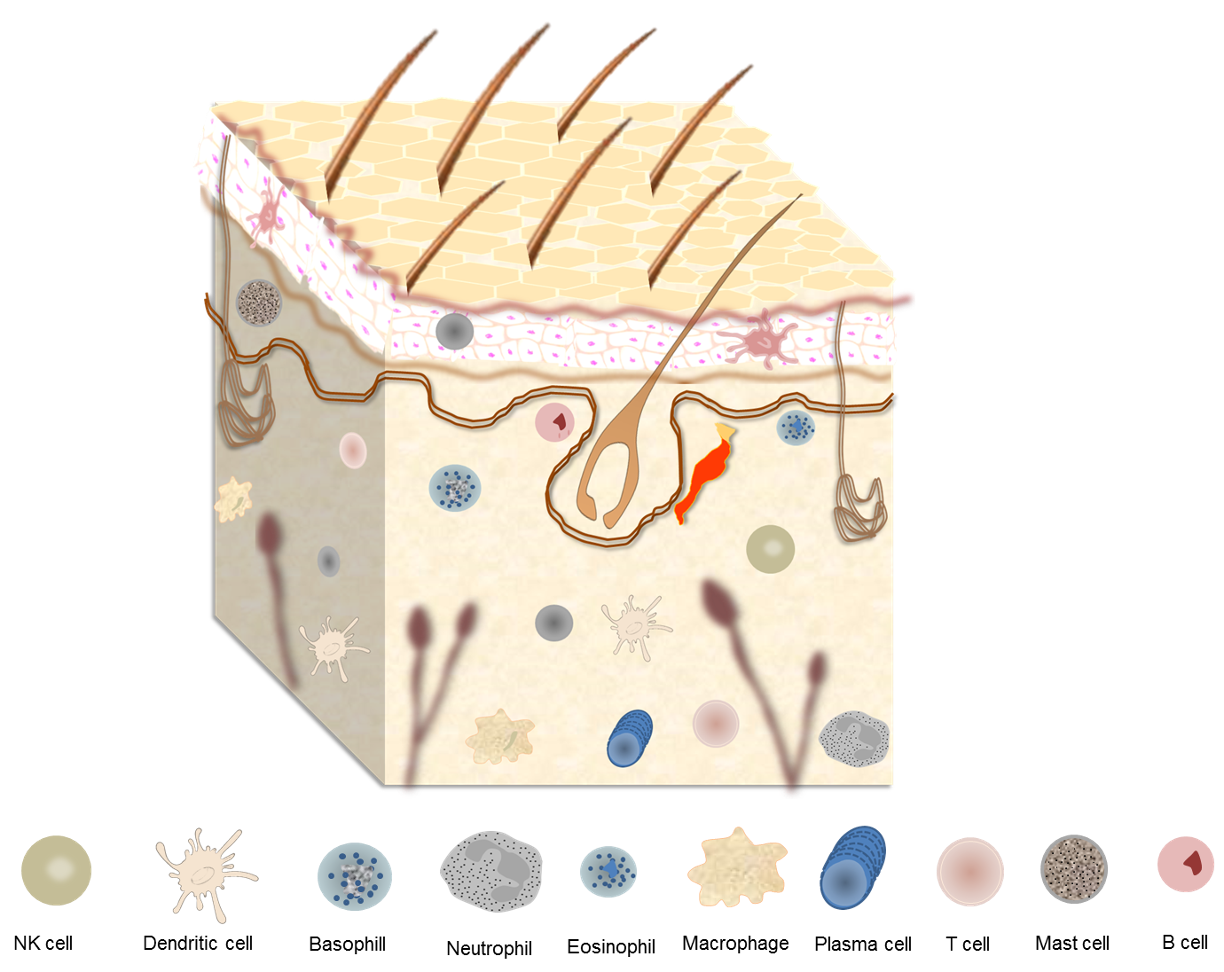
Figure 1.
Skin surface, skin appendages, and major components of skin immune system.
3. The Skin Microbiota
The skin ecosystems are composed of diverse microorganisms that interact with the human body, including host epithelial and immune cells, as well as with other microorganisms sharing the same niche [14][34]. To establish the microbiota, the skin provides essential nutrients, such as amino acids from the hydrolysis of proteins, fatty acids from the stratum corneum, sweat, lipid hydrolysis or sebum, and lactic acids from sweat [15][35]. Since this symbiotic relationship between the host and commensals is crucial for several physiological processes, commensal-specific T cells distinguish resident microorganisms from pathogens to promote commensal tolerance [16][17][36,37]. Microbiota colonization begins at birth and its composition is influenced by several intrinsic (skin site, age, ethnicity, gender, intra- and interpersonal variability) and extrinsic (lifestyle, cosmetic use, use of antibiotics, hygiene routine, climate, seasonality, and geographical location) factors [18][38]. During puberty, it is possible to observe a decrease in the abundance of Firmicutes, including Staphylococcus and Streptococcus species, and increased predominance of Corynebacterium and Cutibacterium (previously known as Propionibacterium). On the other hand, the adult microbial composition remains constant over time despite its continuous exposure to the environment [19][20][39,40]. The skin microbiota composition is distinctive to each person as well as to each part of the body; however, Cutibacterium, Corynebacterium, and Staphylococcus represent the three most dominant microorganism genera in the human skin at the genus level [21][41]. The bacterial diversity is heterogeneous across skin regions due to the variety of glands and density of hair follicles, which create complex and distinct physical and chemical niches for microbial growth. Sebaceous sites, for example, have the lipophilic C. acnes and other Cutibacterium as the dominant species. Over moist sites, instead, Staphylococcus and Corynebacterium are primarily the first colonizing genera, while Lactobacillus is predominant across the female genital tract [22][23][24][14,43,44]. Facial skin microbiota is particularly studied due to its role in aging, acne, and rosacea. It is composed mainly by Proteobacteria (32.91%), Firmicutes (28.69%), Actinobacteria (33.07%), and Bacteroidetes (3.08%), with significant age-dependent profile variations. Subjects aged 36–52 years old have the highest Shannon index, which gives an estimate of the species diversity within a community, as recently demonstrated [25][46].4. Skin Dysbiosis and Cutaneous Alterations
How homeostasis is maintained and shaped by the skin microbiota is still not clear; however, it is well established that the balance between members of skin microbial communities plays a pivotal role in guarding against cutaneous disorders. Changes in composition and the lack of balance among microbial communities is referred to as dysbiosis, a condition that may lead to the onset or progression of diseases. Pronounced dysbiosis on skin may result in several cutaneous diseases including atopic dermatitis (AD), seborrheic dermatitis (SD), rosacea, alopecia areata (AA), and acne [22][26][27][14,51,52]. AD affects 15–20% of children and 2–10% of adults, and results from a complex interaction between genetic susceptibility, barrier dysfunction, innate and adaptive immunity, and microbiota [28][29][53,54]. When compared to healthy controls, AD patients present a loss of diversity with increased abundance of S. aureus and depletion of S. epidermidis and Corynebacterium spp. [30][31][55,56]. Disease severity is also associated with decreased gut microbiome diversity [32][33][57,58]. A dysbiotic scenario with significant alterations of bacteria populations on the scalp skin of SD patients, another common dermatological disorder, was also demonstrated. SD symptoms include skin erythema, flaking, and pruritus. Patients with SD show reduction of Corynebacterium spp. and domination at taxa level by Firmicutes, while at genus level by Pseudomonas spp., Staphylococcus spp., and Micrococcus spp. [34][59].5. Skincare and Skin Microbiota
Skin aging is a complex biological process influenced by the combination of endogenous (intrinsic) and exogenous (extrinsic) factors. The main intrinsic factors are genetics, cellular metabolism, hormones, and metabolic processes, while the main extrinsic factors are chronic light exposure, pollution, ionizing radiation, chemicals, and toxins [35][68]. Skin suffers progressive morphologic and physiologic decrement with increasing age and provides the first obvious evidence of the aging process. A daily skincare routine is essential to enhance smoothness, regenerate it, give strength and elasticity, as well as to prevent the degradation of collagen and elastin, which reduce the formation of wrinkles [36][37][69,70]. Moreover, various studies have examined whether cosmetics could affect skin microbiota composition and balance and have demonstrated that certain bacteria can grow by metabolizing some cosmetic ingredients [38][39][71,72]. It has been demonstrated that even with regular showering, many molecules from personal skincare and hygiene products can last on the skin for weeks after their first use. In this way, a single application of these products may alter the skin chemistry and microbiota for long periods [38][71]. After analyzing the effects of daily use of skincare products, a recent study has suggested that these products might improve skin biophysical parameters such as smoothness and hydration level, while pH and sebum content were maintained. The authors also suggested that a daily skincare routine might improve the microbial health of facial skin and increase the Shannon diversity [40][73]. As is known, high alpha diversity is considered a hallmark of healthy skin microbiota and a balanced skin microbiota is known to play an important role in skin health, as any alterations lead to the overgrowth of pathogenic strains linked to various skin diseases [41][74]. Another study revealed that skin metabolome and microbiome can be altered with changes in the hygiene routine, but that this alteration has responses that are specific to the individual [38][71]. However, as previously cited, the better conditions of skin biophysical parameters, such as barrier function, scaling, and moisturization, are found when its pH average is below 5. Use of products with high pH alkalizes the surface of the skin, which can cause irritability and an increase in dehydration, as well as changes in the microbiota composition by promoting their dispersal from the skin [9][42][9,76]. Therefore, the pH factor should be given due consideration by consumers and cosmetics producers, especially when it comes to sensitive and acne-prone skin.6. Topical Use of Probiotics
The skin microbiota, its interactions with the environment, and the possibility of manipulating it to address cutaneous conditions have opened exciting new paths for dermatological therapies. Therefore, the cosmetic and pharmaceutical industries have been engaged in ordering solutions coming from nature, especially probiotics and postbiotics. The use of probiotics as a potential alternative to antibiotics was previously demonstrated in the treatment of inflammatory bowel disease (IBD) [43][77] and several atopic conditions [44][45][78,79]. Topical probiotics were first proposed as a treatment for cutaneous diseases in 1912 to treat acne and seborrhea [46][80] that involves the transfer of laboratory cultured live bacteria in a dose suitable for skin, to equilibrate the skin microbiota, reestablishing the immune homeostasis [47][81]. Such products rely on the fact that skin immune setting is highly dynamic and can be rapidly remodeled by encounters with specific commensals. In this way, through essential interactions, topical probiotics implement both the establishment and restoration of cutaneous homeostasis [48][82]. It is known that, under specific conditions, probiotics can persist and successfully colonize the skin [49][83], inducing keratinocytes and sebocytes to produce AMPs or other metabolites that can directly inhibit or kill pathogenic microorganisms, shaping microbial communities [50][51][52][84,85,86], and establishing a synergistic effect which improve the ecology of skin microbial communities [53][87]. Considering that the first step in bacterial colonization that leads to infection is cell adhesion, the ability of probiotics to invade and adhere to keratinocytes, promoting inhibition of pathogen binding to these cells, reinforces that probiotics could be used to reduce adhesion of some pathogens to skin [54][88]. Moreover, the potential antimicrobial use of AMPs produced by probiotics has been shown. Indeed, it has been observed that some coagulase-negative Staphylococcus (CoNS) species, including S. hominis and S. epidermidis, can produce commensal-derived AMPs (phenol-soluble modulins and Sh-lantibiotics), which exert selective antimicrobial activity and cooperate synergistically with host-derived AMPs, such as cathelicidin LL-37, to inhibit survival of skin pathogens [50][55][56][57][84,89,90,91]. It has been proposed that by directly producing AMPs, the microbiome provides the first line of defense against microbial pathogens, synergizing with the host innate immune response as a second potent line of defense [50][84]. This normal microbial defense strategy against colonization and transmission of bacterial pathogens should be exploited for anti-infective therapeutics [55][56][57][89,90,91].7. Topical Use Postbiotics
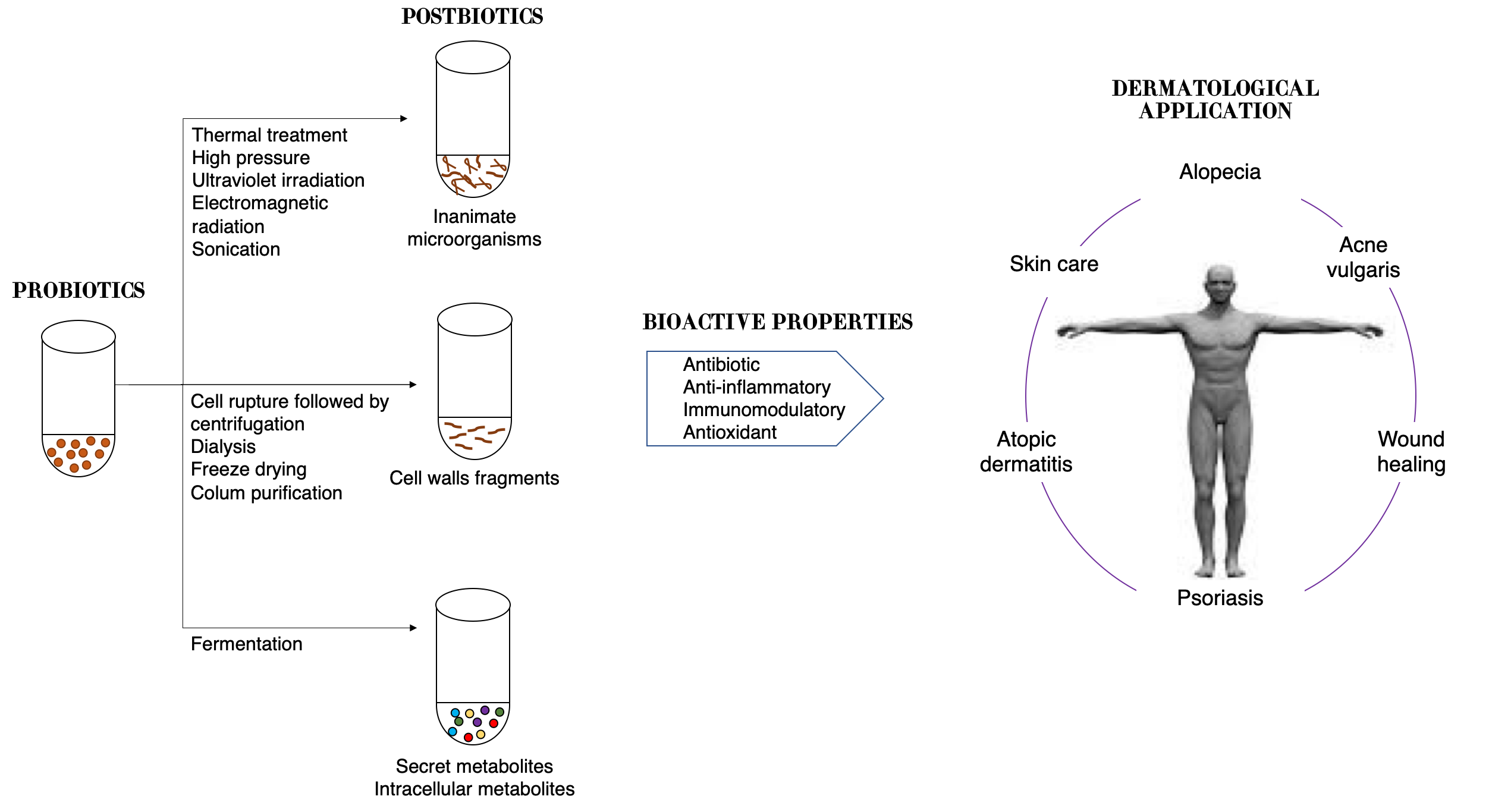
Dead cells present on probiotics are able to produce biological responses as effectively as their live equivalents. In fact, it was demonstrated that in adequate amounts, when administered orally or topically, dead microorganisms confer a benefit on the human or animal consume [58][59][104,105]. However, since they cannot be classified as probiotics, for dead microorganism products new terms have been coined such as postbiotics, paraprobiotics, non-viable probiotics, inactivated probiotics, tyndallized probiotics, or ghost probiotics [60][61][62][106,107,108]. The inactivation of viable cells could be performed by using various mechanical methods, such as sonication, thermal treatment, electromagnetic radiation, high pressure, or ultraviolet irradiation [63][109]. The term postbiotic was recently defined by the International Scientific Association of Probiotics and Prebiotics as “a preparation of inanimate microorganisms and/or their components that confers a health benefit on the host” [64][110]; thus, they cannot colonize the host. Other components that are not required in a postbiotic, such as physiologically active microbial cellular components (cell wall fragments or enzymes) or functional bioactive substances (products or metabolic byproducts) such as vitamins, short-chain fatty acids (SCFAs), proteins and antibiotics, can contribute substantively to the complexity and functionality of the postbiotic preparation [65][111]. It is important to highlight that purified metabolites and purified cell components have specific chemical names of their own that can be used; thus, they do not fall under the scope of postbiotics, and should be referred to as microbe-derived substances. Therefore, postbiotics can be defined as cell-free supernatants without metabolite specification/individualization, cell wall components and/or intracellular compounds (Figure 2). These compounds have many potential health benefits including anti-inflammatory, antioxidant, immunomodulatory, antimicrobial, and anti-ageing/anti-senescence activities [66][112].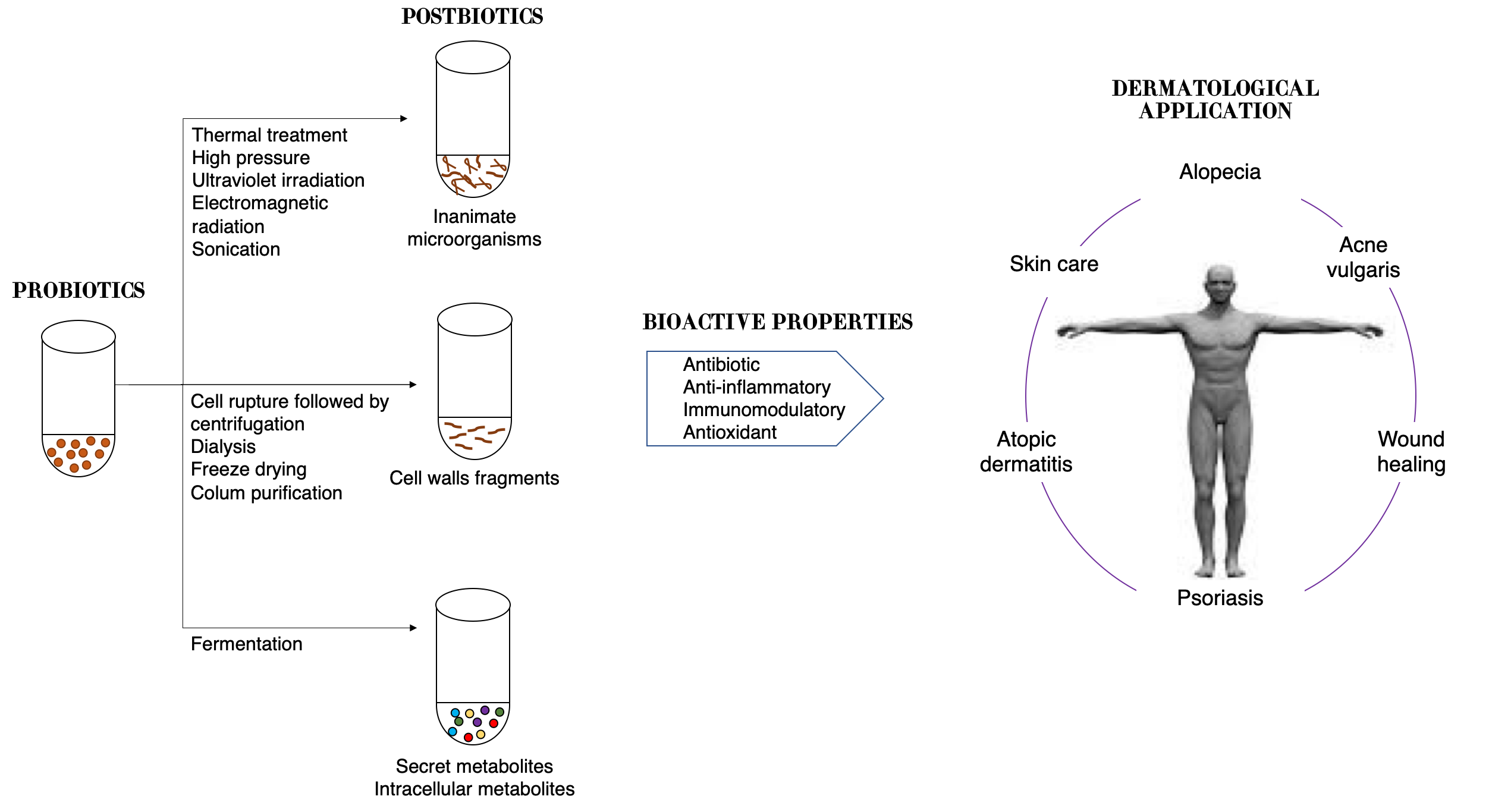
Figure 2.
Schematic representation of approaches in postbiotic production and their benefits to skin health.
Though evidence of microbiota modulation by postbiotics in humans is limited, due to the benefits overcited, the term postbiotic is emerging on commercial products for humans and animals [59][105]. Moreover, great effects on the skin have been seen, such as improved skin moisturizing [67][115], prevention of wrinkle formation [68][116], and amelioration of atopic dermatitis [69][70][117,118].
The topical application of postbiotics from L. fermentum, L. reuteri, and Bacillus subtilis natto, when associated with a cold cream, for example, is being considered as a novel therapeutic approach to accelerate the wound healing process, with an earlier complete epithelization and absence of skin inflammation in the group treated with L. reuteri [71][119]. In vitro antioxidant assays showed significant free radical scavenging activity of a cell-free, casein-free supernatant of L. helveticus strain fermented milk against UVB-induced skin photodamage. The melanin production by melanocytes cells in vitro and the expression of proteins needed for melanin synthesis were inhibited by supernatant.
The topical use of S. thermophiles lysate containing sphingomyelinase, an enzyme that converts sphingomyelin to phosphocholine and ceramide, demonstrated a significant increase in stratum corneum ceramide levels, improved the lipid barrier and reduced water loss [72][122]. A postbiotic from L. plantarum K8 strain lysate was recently suggested as a functional ingredient for moisturizing products, since it was able to increase the mRNA expression levels of moisturizing factors, including HAS2 and AQP3 [73][123].
The LactoSporin® formulation, a cream containing cell-free supernatants of Bacillus coagulans and inactivated cells of Bacillus longum, demonstrated effectiveness in mild-to-moderate acne lesions and other seborrheic conditions in both male and female subjects, due to its ability to reduce sebaceous secretion and oily, greasy nature of the skin even better than benzoyl peroxide [74][128].
