Heart failure (HF) is a worldwide health problem with important consequences for the overall wellbeing of affected individuals as well as for the healthcare system. Numerous pieces of evidence have demonstrated that the associated gut microbiota represent an important component of human physiology and metabolic homeostasis, and can affect one’s state of health or disease directly, or through their derived metabolites. The advances in human microbiome studies shed light on the relationship between the gut microbiota and the cardiovascular system, revealing its contribution to the development of heart failure-associated dysbiosis. HF has been linked to gut dysbiosis, low bacterial diversity, intestinal overgrowth of potentially pathogenic bacteria and a decrease in short chain fatty acids-producing bacteria. An increased intestinal permeability allowing microbial translocation and the passage of bacterial-derived metabolites into the bloodstream is associated with HF progression. A more insightful understanding of the interactions between the human gut microbiome, HF and the associated risk factors is mandatory for optimizing therapeutic strategies based on microbiota modulation and offering individualized treatment.
- heart failure
- gut microbiota
- metabolites
- dysbiosis
- immune modulation
1. Introduction
2. Gut-Associated Microbiome Composition and Function in Healthy Individuals
The human gut microbiome is considered to be an organ on its own with major interactions within the human organism, playing an active role in various immunological, neuronal, metabolic and endocrine responses [13][7]. The highest concentration and diversity of microorganisms from the human body lies in the gastrointestinal tract, consisting of more than 500 distinct species of bacteria, viruses, fungi and protozoa [14,15][8][9]. The GI microbiota are represented by five primary bacterial phyla: the Firmicutes (synonym Bacillota) and Bacteroides (synonym Bacteroidota) phyla predominate the microbiome and represent more than 90% of total bacterial communities, while the Proteobacteria (synonym Pseudomonadota), Actinobacteria (synonym Actinomycetota), and Verrucomicrobia phyla are represented in smaller proportions [13,16][7][10]. Although the Bacillota phylum consists of more than 200 different genera such as Bacillus, Lactobacillus, Enterococcus, Ruminococcus and Clostridium, and the Clostridium genus represents 95% of the phylum. The Bacteroidota phylum is predominated by the Prevotella and Bacteroides genera. The Actinomycetota phylum is significantly less abundant than Bacteroidota phylum and the Bifidobacterium genus is its main representative [17][11]. The microbiome is not inherited, but acquired, and its composition is changing through different stages of each individual’s life, with a unique composition and microbial diversity [19,20][12][13]. Its development starts early, in prenatal life, and continues during birth and through senescence [21,22][14][15]. The following interfere with microbiome composition, leading the way to health or disease: sex; genetics; the mother’s influence during pregnancy and birth; feeding practices in early childhood; dietary habits; antibiotics; tobacco and alcohol use; a sedentary lifestyle associated with the socioeconomic conditions; household pets; pollution; and geographical distribution [15,21,22,23,24][9][14][15][16][17]. Whereas each individual’s gut microbiota are characterized by a specific combination of bacterial species, due to inter-individual and intra-individual variations throughout human life, the human gut microbiota’s functions are highly preserved between individuals [13][7]. In addition to one’s genetic susceptibility, the diversity of the microbiome’s composition plays a key role in each individual’s personalized response to different environmental exposures such as diet, xenobiotics and medical treatments [2]. The GI mucosa represents the site of the human–external environment interaction. The GI microbiota and the intestinal barrier have bidirectional communication and form a complex network influencing the human state of health and disease [14][8]. Besides its function as an organ used for digestion and absorption, the GI tract acts as an immune organ, the human body’s largest immune organ [25][18]. “Healthy” gut microbiota have the capacity for: preserving the stability of the intestinal wall and its barrier function; tight epithelial junctions and a normal mucosal immunity; and preventing pathogen proliferation [2]. The gut-associated microbiota can regulate the inflammatory response directly, inducing either innate or adaptive immune responses, or it can alter the immune cells’ function using active metabolites, including short-chain fatty acids (SCFAs), trimethylamine N-oxide (TMA-O) and indoleacetic acid (IAA) [26,27,28][19][20][21].3. Impaired Gut Barrier Function and Inflammation in Heart Failure
The “gut hypothesis” in HF suggests that there is a strong relationship between the gut microbiota, its metabolites and HF pathogenesis, as illustrated in Figure 1 [2,31][2][22]. Although this bidirectional communication is not fully understood, evidence indicates that this bacterial translocation appears in HF as a consequence of various mechanisms leading to structural and functional alterations of the GI tract, from splanchnic congestion to the host’s immunological defense system [7][23].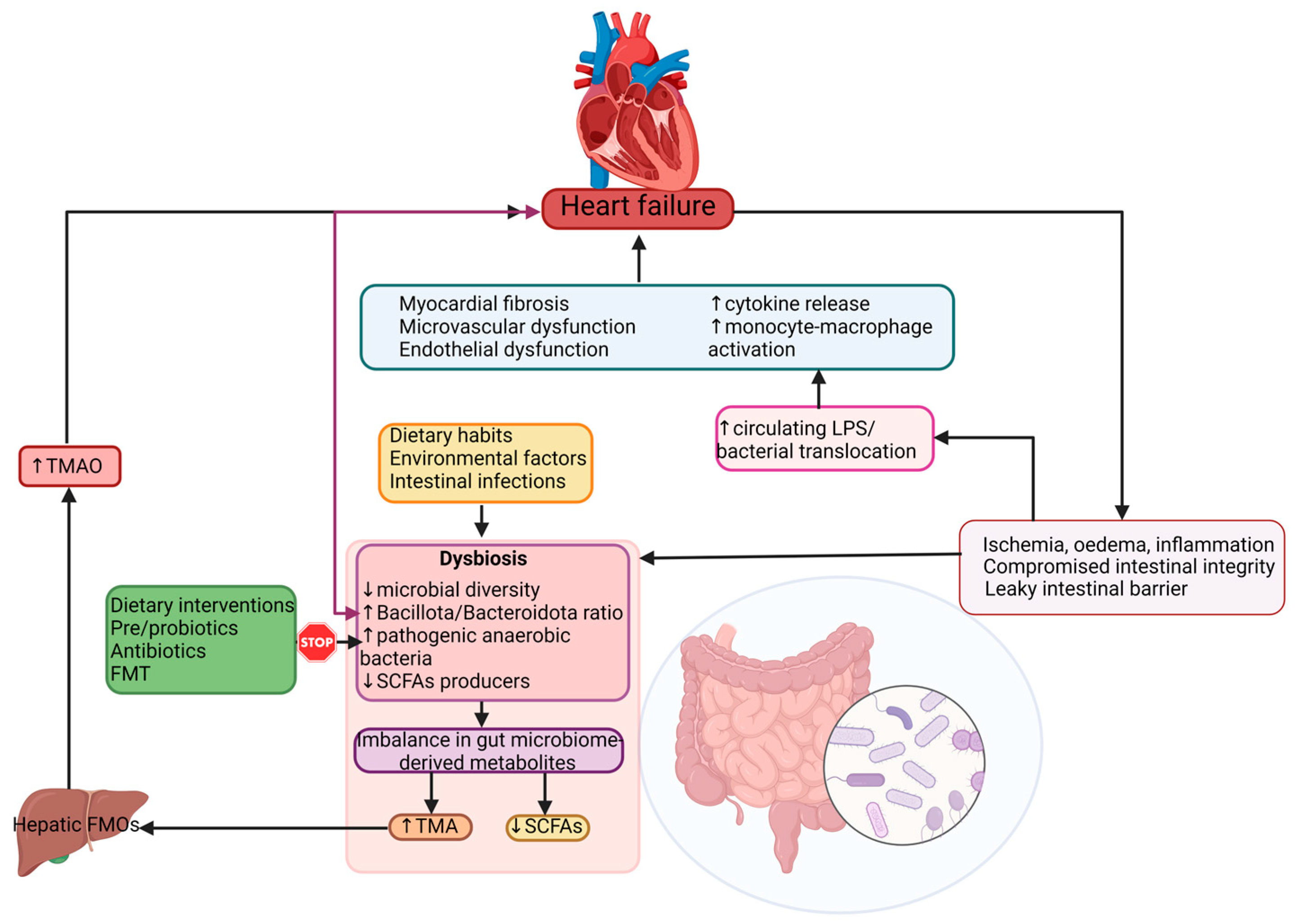
4. Dysbiosis in Heart Failure
5. Risk Factors for HF and Gut Microbiota
5.1. Dietary Choices
The Western diet (WD) is characterized by high sugar and refined carbohydrate intake with a high glycemic index; content that inhibits nitric oxide synthase, resulting in myocardial oxidative dysfunction, cardiac hypertrophy and cardiomyocyte remodeling, all known to be predisposing factors for HF [77][45]. This diet rich in fast-food aliments and glucose leads to dysbiosis state characterized by elevated Pseudomonadota and Bacillota levels, which increases the levels of TMAO and ceramides, promotes cholesterol accumulation in macrophages and promotes atherosclerosis development [78][46]. The WD also leads to lipid accumulation in the myocardium, chronic inflammation and obesity [79][47]. Increased levels of salt and dietary additives used in fast-food alimentary processing, including nitrites and phosphates, have been associated to an increased risk of HF. They alter the Bacillota to Bacteroidota ratio [80][48].5.2. Obesity
Savji and colleagues [81][49] in their study reported that obesity and its associated dysmetabolism, including hyperlipidemia, hyperglycemia and insulin resistance, are strongly correlated with HF [81][49]. A pro-inflammatory environment characterized by elevated levels of pro-inflammatory cytokines is promoted by obesity and its associated cardiometabolic factors (insulin resistance, dyslipidemia and abdominal adiposity) [82][50]. The endothelial dysfunction and the nitric oxide unavailability might lead to left ventricular hypertrophy and systolic and diastolic dysfunction in HFpEF [82,83][50][51].5.3. Type II Diabetes Mellitus
Type II diabetes mellitus (T2DM) is a strongly associated risk factor for HF and other CVD. Patients known to have T2DM present a decreased level of bacterial genera such as Faecalibacterium, Bifidobacterium, Akkermansia, Bacteroides and Roseburia. Roseburia, Bacteroides and Akkermansia have anti-inflammatory effects. Bacteroides and Akkermansia in decreased levels lead to an under expression of tight junctions’ genes, elevated “leaky gut”, and, in consequence, endotoxemia [89][52].5.4. Hypertension
Persistently elevated blood pressure (BP) patients present a higher (up to five-fold) Bacillota-to-Bacteroidota ratio in comparison to normotensive controls [93][53]. Moreover, the intestinal microbiota is dominated by lactate-producing genera (e.g., Turicibacter and Streptococcus), while SCFA-producing ones appear to be reduced (such as Clostridiaceae, Bacteroides and Akkermansia) when hypertension is present [94,95][54][55]. Some of these associated perturbations in gut microbiota homeostasis are partially related to HF pathogenesis and increase the risk of HF progression.6. Gut-Derived Metabolites as Possible Biomarkers Related to Intestinal Dysbiosis in HF
A biomarker is defined as a biological compound that is easily accessible and measurable in the body. Biomarkers can be classified as molecular, cellular or imaging. Their role is to help in identifying the disease or provide therapeutic guidance. Natriuretic Peptides (NP), brain-type natriuretic peptide (BNP), N-terminal prohormone of BNP and cardiac troponin measurements—classic HF biomarkers—have already been included in the guidelines for HF diagnosis and treatment by the European Society of Cardiology (ESC) [96][56] and the American Heart Association (AHA) [97][57]. The addition of other diagnostic and prognostic biomarkers that could be associated to such a complex disease would be of benefit for both patients and medical practitioners. Gut microbial-derived metabolites can also play a significant role in the pathogenesis of HF. It appears that the gut microbiome acts similarly to an endocrine organ. By generating active biometabolites including short-chain fatty acids (SCFAs), trimethylamine (TMA)/trimethylamine N-oxide (TMAO), and bile acids, the gut microbiome influences the host physiology. Several studies described the association of the gut’s microbiome metabolites and different pathologies including hypertension, atherosclerosis, HF, obesity, chronic kidney disease, and T2DM [2,7,98,99,100,101][2][23][58][59][60][61]. These metabolites can be considered as biomarkers of intestinal dysbiosis and can predict inflammation in patients known with HF [101][61]. These patients with elevated plasma levels of phenylalanine display increased levels of inflammatory cytokines (IL-8, IL-10), C-reactive protein (CRP) and associate higher mortality [102][62], whereas glycine manifest anti-inflammatory effects and seem to offer protection to the cells and heart [103][63]. Alterations of gut microbiota composition, especially elevated N-oxidetrimethylamine (TMAO) levels are correlated with the risk of developing HF [106][64]. TMAO is a metabolite produced by gut bacteria including Bacillota and Pseudomonadota, obtained from choline, phosphatidylcholine, and L-carnitine fermentation [2]. Chen and colleagues [106][64] reported that an elevated level of TMAO resulted from a diet high in saturated fat and sugar can lead to fibrosis, myocardial inflammation and to impaired diastolic function [106][64]. Individuals with an increased abundance of Ruminococcus, Prevotella and Clostridium genera and the Lachnospiraceae family, and decreased levels of Bacteroidota, revealed higher levels of TMAO in their plasma [107,108][65][66]. HF–associated dysbiosis is characterized by high levels of circulating TMAO, that are able to stimulate cardiac remodeling through promoting myocardial fibrosis and pro-inflammatory effects [2,77,109,110][2][45][67][68]. HF patients display elevated plasma levels of TMAO when compared to healthy individuals. Increased TMAO levels can be used as a prognostic biomarker in both acute and chronic HF, independently of B-type natriuretic peptide (BNP) and traditional risk factors, as TMAO levels are predictive of an augmented risk of mortality in these patients [80,81][48][49]. Elevated TMAO plasma values correspond with advanced stages of left ventricular diastolic dysfunction [80][48]. TMAO can also be considered a prognostic predictor of HFeEF and a marker of risk stratification for this particular category of patients [112,113][69][70]. The SCFAs are represented by acetate, propionate and butyrate, and they are generated by gut bacteria including Bacteroides, Bifidobacterium and Faecalibacterium spp. [53][71]. They are the most important metabolites produced through colon bacteria fermentation of resistant starch and dietary fibers [101][61]. Most evidence sustains the fact that SCFAs have a protective role against HF and play a major role in maintaining the integrity of the intestinal barrier: in mucus production and they are active in anti-inflammation protection [67][72].7. Interactions between the Gut Microbiome and Cardiovascular Drugs
Age, sex, nutritional status, disease states, along with genetic and environmental exposures are factors that can explain how individuals will respond to drug therapies [121][73]. The human microbiome is known for its involvement in drug metabolism and pharmacological efficacy, but among them there is bidirectional communication, as drugs can also influence microbiota composition. Drug absorption is an elaborate process, depending on many factors such as their solubility and stability in GI fluids, their pH, GI transit period, permeability through epithelial membranes and the drugs’ interaction with the host and microbial enzymes [122][74]. The human gut microbiota is genetically capable of producing enzymes involved in oral drugs’ metabolism, facilitating their absorption across the gut and through the bloodstream [121][73]. Dysbiosis of the gut’s bacterial communities can further alter drug pharmacokinetics; the activation of prodrugs can contribute to the production of unwanted toxic metabolites and the inactivation of drugs [123][75]. Variation in drug response can also be present in a “healthy” gut, due to inter-individual differences in intestinal bacterial species [13][7]. Related to the cardiovascular medication used in HF patients, metagenomic sequencing of stool samples from HF patients revealed that the use of several pharmaceutical agents such as statins, beta-blockers, angiotensin-converting enzyme inhibitors and platelet aggregation inhibitors has an important influence on gut microbial composition [124][76]. Despite the fact that specific underlying mechanisms are unknown, partial results of thise study were reproduced by another British group of researchers [125][77].7.1. Cardiac Glycosides
Digoxin, a drug frequently recommended in HF is a good example of microbiota influencing drug bioavailability. Some strains of Eggerthella lenta are responsible for converting digoxin into an inactive microbial metabolite, limiting the quantity of active drug absorbed into the systemic bloodstream in an important 10 percent of patients [126,133][78][79].7.2. Blood Thinners and Gut Microbiota
Aspirin is a non-steroidal anti-inflammatory drug (NSAIDS) commonly used to decrease the risk of cerebrovascular and cardiovascular disorders [133][79]. Existing evidence demonstrates its ability to disrupt the gut’s microbiota composition. Patients using aspirin present variations of Ruminococcaceae, Prevotella, Barnesiella and Bacteroides bacterial levels in comparison to individuals not using or using other types of NSAIDs. Furthermore, the gut’s bacterial communities’ composition seems to exert influence on aspirin metabolism. While oral antibiotic administration can decrease the gut microbiota’s metabolic activity by slowing its degradation, increasing its bioavailability and prolonging its anti-thrombotic action, probiotics containing Bifidobacterium breve Bif195 bacteria can protect against an aspirin intake adverse reaction, such as intestinal wall damage and aspirin-induced gastric ulcers [135,136][80][81].7.3. The Effects of Beta-Blockers, ACEi, and ARBs on Gut Microbiota
The effects of antihypertensive medications have been investigated on several occasions, both in animal and human studies. Despite expectations, the association between the use of beta-blockers, angiotensin receptor blockers (ARBs) and angiotensin converting enzyme inhibitors (ACE inhibitors) can modify the composition of gut microbiota.7.4. Statins and Gut Microbiota
Statins are drugs used for their capacity to decrease low-density-lipoprotein-C (LDL-C) and cholesterol levels. Inter-individual variations in the response to statin treatment are well-known, and are not related to a specific statin agent or dose [124][76]. Studies have proven their action on modulating gut bacterial communities’ composition [121,128][73][82]. Individuals treated with atorvastatin presented an increased level of anti-inflammatory gut bacteria such as Faecalibacterium prausnitzii and Akermansia muciniphila, whereas untreated patients known with hypercholesterolemia displayed an increased level of bacterial species with pro-inflammatory effects, such as Collinsella and Streptococcus [140][83]. LDL-C levels seem to be negatively correlated to the phyla Bacillota and Fusobacteria, while Lentisphaerae and Cyanobacteria spp. were positively associated with LDL-C [128][82].8. Modulation of Dysbiosis as a Potential Target in Heart Failure
Considering that dysbiosis is a key factor in HF pathogenesis and disease progression, targeting the disrupted gut microbiota could be considered an effective therapeutic objective. The possibility of characterizing each patient’s gut microbiota and his disease-associated dysbiosis allows the initiation of a personalized, targeted therapeutic plan. Although there are various ways to manage and modulate the dysbiotic intestinal microbiota, such as dietary interventions (which also include the use of prebiotics, prebiotics and postbiotics) and fecal transplantation, several reports from the available literature place diet modification and probiotic use as the main interventions for microbiota modulation. Diet has always been considered a crucial factor in shaping the structure and function of gut’s associated microbiota. A 5-day adjusted diet has been shown to produce beneficial changes in the number and species of the gut microbiota [145][84]. Often cited in the medical literature, the Mediterranean diet (MD) consists of elevated levels of polyunsaturated fatty acids, dietary fiber, polyphenols, and a small quantity of red meat [77][45]. Among its recognized benefits on human health, an MD provides an increased abundance of probiotics, greater biodiversity, elevated SCFAs, and reduced TMAO [146,147][85][86]. Adherence to an MD was associated with a decreasing HF incidence up to 74% [148][87]. A high-fiber diet has recently been demonstrated to improve gut dysbiosis (described by the Bacilliota and Bacteroidota ratio), reduced blood pressure, improved cardiac function and normalized cardiac hypertrophy in a hypertension-induced HF experimental model [153][88]. Additionally, fermentation of fiber results in augmented SCFA production, with their beneficial actions on human health [150][89]. Related to antibiotic use in modulating the gut microbiota in HF patients, results are controversial. In animal models, oral vancomycin use induced smaller left ventricular infarct size, and improved recovery cardiac function following ischemia/reperfusion experiments in treated, compared to untreated, rats [166][90]. Rifamixin, besides its bactericidal and bacteriostatic effect, also has the capacity to reduce translocation of bacteria and toxicity, has an anti-inflammatory effect and can positively regulate the composition of the intestinal microbiota, promoting the growth of lactobacillus and bifidobacteria [167,168][91][92]. As for human clinical trials, the results are contradictory. The use of a cocktail of tobramicyn and polymixin B, in HF patients, normalized the level of intestinal Gram-negative bacilli, significantly decreased pro-inflammatory cytokines and improved flow-mediated dilation: evidence of endothelial dysfunction [169][93]. Prebiotics are “a selectively fermented ingredient that results in specific changes in the composition and/or activity of the gastrointestinal microbiota, thus conferring benefit(s) upon host health” [171][94]. Prebiotics use could increase the amount of Bifidobacterium and promotes a higher body weight loss, which decreased systolic and diastolic blood pressure [172][95].References
- Groenewegen, A.; Rutten, F.H.; Mosterd, A.; Hoes, A.W. Epidemiology of heart failure. Eur. J. Heart Fail. 2020, 22, 1342–1356.
- Tang, W.H.W.; Li, D.Y.; Hazen, S.L. Dietary metabolism, the gut microbiome, and heart failure. Nat. Rev. Cardiol. 2019, 16, 137–154.
- Shirazi, L.F.; Bissett, J.; Romeo, F.; Mehta, J.L. Role of Inflammation in Heart Failure. Curr. Atheroscler. Rep. 2017, 19, 27.
- Nemet, I.; Saha, P.P.; Gupta, N.; Zhu, W.; Romano, K.A.; Skye, S.M.; Cajka, T.; Mohan, M.L.; Li, L.; Wu, Y.; et al. A Cardiovascular Disease-Linked Gut Microbial Metabolite Acts via Adrenergic Receptors. Cell 2020, 180, 862–877.e22.
- Kummen, M.; Mayerhofer, C.C.K.; Vestad, B.; Broch, K.; Awoyemi, A.; Storm-Larsen, C.; Ueland, T.; Yndestad, A.; Hov, J.R.; Trøseid, M. Gut Microbiota Signature in Heart Failure Defined From Profiling of 2 Independent Cohorts. J. Am. Coll. Cardiol. 2018, 71, 1184–1186.
- Hietbrink, F.; Besselink, M.G.; Renooij, W.; de Smet, M.B.; Draisma, A.; van der Hoeven, H.; Pickkers, P. Systemic inflammation increases intestinal permeability during experimental human endotoxemia. Shock 2009, 32, 374–378.
- Bozomitu, L.; Miron, I.; Adam Raileanu, A.; Lupu, A.; Paduraru, G.; Marcu, F.M.; Buga, A.M.L.; Rusu, D.C.; Dragan, F.; Lupu, V.V. The Gut Microbiome and Its Implication in the Mucosal Digestive Disorders. Biomedicines 2022, 10, 3117.
- Di Tommaso, N.; Gasbarrini, A.; Ponziani, F.R. Intestinal Barrier in Human Health and Disease. Int. J. Environ. Res. Public Health 2021, 18, 12836.
- Dekaboruah, E.; Suryavanshi, M.V.; Chettri, D.; Verma, A.K. Human microbiome: An academic update on human body site specific surveillance and its possible role. Arch. Microbiol. 2020, 202, 2147–2167.
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010, 464, 59–65.
- Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; Batto, J.M.; et al. Enterotypes of the human gut microbiome. Nature 2011, 473, 174–180, Erratum in Nature 2011, 474, 666; Erratum in Nature 2014, 506, 516.
- Sharon, I.; Quijada, N.M.; Pasolli, E.; Fabbrini, M.; Vitali, F.; Agamennone, V.; Dötsch, A.; Selberherr, E.; Grau, J.H.; Meixner, M.; et al. The Core Human Microbiome: Does It Exist and How Can We Find It? A Critical Review of the Concept. Nutrients 2022, 14, 2872.
- Sandek, A.; Bjarnason, I.; Volk, H.D.; Crane, R.; Meddings, J.B.; Niebauer, J.; Kalra, P.R.; Buhner, S.; Herrmann, R.; Springer, J.; et al. Studies on bacterial endotoxin and intestinal absorption function in patients with chronic heart failure. Int. J. Cardiol. 2012, 157, 80–85.
- Piggott, D.A.; Tuddenham, S. The gut microbiome and frailty. Transl. Res. 2020, 221, 23–43.
- Stinson, L.F.; Boyce, M.C.; Payne, M.S.; Keelan, J.A. The Not-so-Sterile Womb: Evidence That the Human Fetus Is Exposed to Bacteria Prior to Birth. Front. Microbiol. 2019, 10, 1124.
- Li, S.; Kararigas, G. Role of Biological Sex in the Cardiovascular-Gut Microbiome Axis. Front. Cardiovasc. Med. 2022, 8, 759735.
- Mills, S.; Stanton, C.; Lane, J.A.; Smith, G.J.; Ross, R.P. Precision Nutrition and the Microbiome, Part I: Current State of the Science. Nutrients 2019, 11, 923.
- Wang, W.; Zhu, L.J.; Leng, Y.Q.; Wang, Y.W.; Shi, T.; Wang, W.Z.; Sun, J.C. Inflammatory Response: A Crucial Way for Gut Microbes to Regulate Cardiovascular Diseases. Nutrients 2023, 15, 607.
- Steimle, A.; Frick, J.S. Molecular Mechanisms of Induction of Tolerant and Tolerogenic Intestinal Dendritic Cells in Mice. J. Immunol. Res. 2016, 2016, 1958650.
- Ilyas, A.; Wijayasinghe, Y.S.; Khan, I. Implications of trimethylamine N-oxide (TMAO) and Betaine in Human Health: Beyond Being Osmoprotective Compounds. Front. Mol. Biosci. 2022, 9, 964624.
- Su, X.; Gao, Y.; Yang, R. Gut Microbiota-Derived Tryptophan Metabolites Maintain Gut and Systemic Homeostasis. Cells 2022, 11, 2296.
- Nagatomo, Y.; Tang, W.H.W. Intersections between microbiome and heart failure: Revisiting the gut hypothesis. J. Card Fail. 2015, 21, 973–980.
- Mu, F.; Tang, M.; Guan, Y.; Lin, R.; Zhao, M.; Zhao, J.; Huang, S.; Zhang, H.; Wang, J.; Tang, H. Knowledge Mapping of the Links Between the Gut Microbiota and Heart Failure: A Scientometric Investigation (2006–2021). Front. Cardiovasc. Med. 2022, 9, 882660.
- Kamo, T.; Akazawa, H.; Suda, W.; Saga-Kamo, A.; Shimizu, Y.; Yagi, H.; Liu, Q.; Nomura, S.; Naito, A.T.; Takeda, N.; et al. Dysbiosis and compositional alterations with aging in the gut microbiota of patients with heart failure. PLoS ONE 2017, 12, e0174099.
- Gallo, A.; Macerola, N.; Favuzzi, A.M.; Nicolazzi, M.A.; Gasbarrini, A.; Montalto, M. The Gut in Heart Failure: Current Knowledge and Novel Frontiers. Med. Princ. Pract. 2022, 31, 203–214.
- Sandek, A.; Swidsinski, A.; Schroedl, W.; Watson, A.; Valentova, M.; Herrmann, R.; Scherbakov, N.; Cramer, L.; Rauchhaus, M.; Grosse-Herrenthey, A.; et al. Intestinal blood flow in patients with chronic heart failure: A link with bacterial growth, gastrointestinal symptoms, and cachexia. J. Am. Coll. Cardiol. 2014, 64, 1092–1110.
- Sandek, A.; Bauditz, J.; Swidsinski, A.; Buhner, S.; Weber-Eibel, J.; von Haehling, S.; Schroedl, W.; Karhausen, T.; Doehner, W.; Rauchhaus, M.; et al. Altered intestinal function in patients with chronic heart failure. J. Am. Coll. Cardiol. 2007, 50, 1561–1569.
- Anker, S.D.; Egerer, K.R.; Volk, H.D.; Kox, W.J.; Poole-Wilson, P.A.; Coats, A.J. Elevated soluble CD14 receptors and altered cytokines in chronic heart failure. Am. J. Cardiol. 1997, 79, 1426–1430.
- Lu, Y.C.; Yeh, W.C.; Ohashi, P.S. LPS/TLR4 signal transduction pathway. Cytokine 2008, 42, 145–151.
- Peschel, T.; Schonauer, M.; Thiele, H.; Anker, S.D.; Schuler, G.; Niebauer, J. Invasive assessment of bacterial endotoxin and inflammatory cytokines in patients with acute heart failure. Eur. J. Heart Fail 2003, 5, 609–614.
- Thierer, J.; Acosta, A.; Vainstein, N.; Sultan, M.; Francesia, A.; Marino, J.; Prado, A.H.; Guglielmone, R.; Trivi, M.; Boero, L.; et al. Relation of left ventricular ejection fraction and functional capacity with metabolism and inflammation in chronic heart failure with reduced ejection fraction (from the MIMICA Study). Am. J. Cardiol. 2010, 105, 977–983.
- Deswal, A.; Petersen, N.J.; Feldman, A.M.; Young, J.B.; White, B.G.; Mann, D.L. Cytokines and cytokine receptors in advanced heart failure: An analysis of the cytokine database from the Vesnarinone trial (VEST). Circulation 2001, 103, 2055–2059.
- Rauchhaus, M.; Doehner, W.; Francis, D.P.; Davos, C.; Kemp, M.; Liebenthal, C.; Niebauer, J.; Hooper, J.; Volk, H.D.; Coats, A.J.; et al. Plasma cytokine parameters and mortality in patients with chronic heart failure. Circulation 2000, 102, 3060–3067.
- Kitai, T.; Kirsop, J.; Tang, W.H. Exploring the Microbiome in Heart Failure. Curr. Heart Fail Rep. 2016, 13, 103–109.
- Pasini, E.; Aquilani, R.; Testa, C.; Baiardi, P.; Angioletti, S.; Boschi, F.; Verri, M.; Dioguardi, F. Pathogenic Gut Flora in Patients With Chronic Heart Failure. JACC Heart Fail. 2016, 4, 220–227.
- Hayashi, T.; Yamashita, T.; Watanabe, H.; Kami, K.; Yoshida, N.; Tabata, T.; Emoto, T.; Sasaki, N.; Mizoguchi, T.; Irino, Y.; et al. Gut Microbiome and Plasma Microbiome-Related Metabolites in Patients With Decompensated and Compensated Heart Failure. Circ. J. 2018, 83, 182–192.
- Sun, W.; Du, D.; Fu, T.; Han, Y.; Li, P.; Ju, H. Alterations of the Gut Microbiota in Patients With Severe Chronic Heart Failure. Front. Microbiol. 2022, 12, 813289.
- Duncan, S.H.; Holtrop, G.; Lobley, G.E.; Calder, A.G.; Stewart, C.S.; Flint, H.J. Contribution of acetate to butyrate formation by human faecal bacteria. Br. J. Nutr. 2004, 91, 915–923.
- Cui, X.; Ye, L.; Li, J.; Wang, W.; Li, S.; Bao, M.; Wu, S.; Li, L.; Geng, B.; Zhou, X.; et al. Metagenomic and metabolomic analyses unveil dysbiosis of gut microbiota in chronic heart failure patients. Sci. Rep. 2018, 8, 635.
- Sokol, H.; Pigneur, B.; Watterlot, L.; Lakhdari, O.; Bermudez-Humaran, L.G.; Gratadoux, J.J.; Blugeon, S.; Bridonneau, C.; Furet, J.P.; Corthier, G.; et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. USA 2008, 105, 16731–16736.
- Martin, R.; Miquel, S.; Chain, F.; Natividad, J.M.; Jury, J.; Lu, J.; Sokol, H.; Theodorou, V.; Bercik, P.; Verdu, E.F.; et al. Faecalibacterium prausnitzii prevents physiological damages in a chronic low-grade inflammation murine model. BMC Microbiol. 2015, 15, 67.
- Leonel, A.J.; Alvarez-Leite, J.I. Butyrate: Implications for intestinal function. Curr. Opin. Clin. Nutr. Metab. Care 2012, 15, 474–479.
- Furusawa, Y.; Obata, Y.; Fukuda, S.; Endo, T.A.; Nakato, G.; Takahashi, D.; Nakanishi, Y.; Uetake, C.; Kato, K.; Kato, T.; et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 2013, 504, 446–450.
- Li, L.; Zhong, S.J.; Hu, S.Y.; Cheng, B.; Qiu, H.; Hu, Z.X. Changes of gut microbiome composition and metabolites associated with hypertensive heart failure rats. BMC Microbiol. 2021, 21, 141.
- Yu, W.; Jiang, Y.; Xu, H.; Zhou, Y. The Interaction of Gut Microbiota and Heart Failure with Preserved Ejection Fraction: From Mechanism to Potential Therapies. Biomedicines 2023, 11, 442.
- Hairrman, R.S.; Gouveia, C.G.; Sichinel, Â.H.; Silva, L.S.A.; Oliveira, T.S.S.; Farias, M.N. Tmao and the relationship with cardiovascular disease: The elderly and their physiological aspects. Braz. J. Dev. 2021, 7, 6971–6982.
- Trøseid, M.; Andersen, G.Ø.; Broch, K.; Hov, J.R. The gut microbiome in coronary artery disease and heart failure: Current knowledge and future directions. EBioMedicine 2020, 52, 102649.
- Tang, W.H.; Wang, Z.; Fan, Y.; Levison, B.; Hazen, J.E.; Donahue, L.M.; Wu, Y.; Hazen, S.L. Prognostic value of elevated levels of intestinal microbe-generated metabolite trimethylamine-N-oxide in patients with heart failure: Refining the gut hypothesis. J. Am. Coll. Cardiol. 2014, 64, 1908–1914.
- Savji, N.; Meijers, W.C.; Bartz, T.M.; Bhambhani, V.; Cushman, M.; Nayor, M.; Kizer, J.R.; Sarma, A.; Blaha, M.J.; Gansevoort, R.T.; et al. The Association of Obesity and Cardiometabolic Traits With Incident HFpEF and HFrEF. JACC Heart Fail. 2018, 6, 701–709.
- Paulus, W.J.; Tschöpe, C. A novel paradigm for heart failure with preserved ejection fraction: Comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 2013, 62, 263–271.
- Wang, Y.C.; Liang, C.S.; Gopal, D.M.; Ayalon, N.; Donohue, C.; Santhanakrishnan, R.; Sandhu, H.; Perez, A.J.; Downing, J.; Gokce, N.; et al. Preclinical Systolic and Diastolic Dysfunctions in Metabolically Healthy and Unhealthy Obese Individuals. Circ. Heart Fail. 2015, 8, 897–904.
- Gurung, M.; Li, Z.; You, H.; Rodrigues, R.; Jump, D.B.; Morgun, A.; Shulzhenko, N. Role of gut microbiota in type 2 diabetes pathophysiology. EBioMedicine 2020, 51, 102590.
- Okamura, M.; Ueno, T.; Tanaka, S.; Murata, Y.; Kobayashi, H.; Miyamoto, A.; Abe, M.; Fukuda, N. Increased expression of acyl-CoA oxidase 2 in the kidney with plasma phytanic acid and altered gut microbiota in spontaneously hypertensive rats. Hypertens Res. 2021, 44, 651–661.
- Yang, T.; Santisteban, M.M.; Rodriguez, V.; Li, E.; Ahmari, N.; Carvajal, J.M.; Zadeh, M.; Gong, M.; Qi, Y.; Zubcevic, J.; et al. Gut dysbiosis is linked to hypertension. Hypertension 2015, 65, 1331–1340.
- Adnan, S.; Nelson, J.W.; Ajami, N.J.; Venna, V.R.; Petrosino, J.F.; Bryan, R.M., Jr.; Durgan, D.J. Alterations in the gut microbiota can elicit hypertension in rats. Physiol. Genom. 2017, 49, 96–104.
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726, Erratum in Eur. Heart J. 2021, 42, 3599–3726.
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e895–e1032, Erratum in Circulation 2022, 145, e1033; Erratum in Circulation 2022, 146, e185.
- Verhaar, B.J.H.; Prodan, A.; Nieuwdorp, M.; Muller, M. Gut Microbiota in Hypertension and Atherosclerosis: A Review. Nutrients 2020, 12, 2982.
- Liu, B.N.; Liu, X.T.; Liang, Z.H.; Wang, J.H. Gut microbiota in obesity. World J. Gastroenterol. 2021, 27, 3837–3850.
- Hobby, G.P.; Karaduta, O.; Dusio, G.F.; Singh, M.; Zybailov, B.L.; Arthur, J.M. Chronic kidney disease and the gut microbiome. Am. J. Physiol. Renal. Physiol. 2019, 316, F1211–F1217.
- Francisqueti-Ferron, F.V.; Nakandakare-Maia, E.T.; Siqueira, J.S.; Ferron, A.J.T.; Vieira, T.A.; Bazan, S.G.Z.; Corrêa, C.R. The role of gut dysbiosis-associated inflammation in heart failure. Rev. Assoc. Med. Bras 2022, 68, 1120–1124.
- Tuerhongjiang, G.; Guo, M.; Qiao, X.; Lou, B.; Wang, C.; Wu, H.; Wu, Y.; Yuan, Z.; She, J. Interplay Between Gut Microbiota and Amino Acid Metabolism in Heart Failure. Front. Cardiovasc. Med. 2021, 8, 752241.
- Chen, W.S.; Wang, C.H.; Cheng, C.W.; Liu, M.H.; Chu, C.M.; Wu, H.P.; Huang, P.C.; Lin, Y.T.; Ko, T.; Chen, W.H.; et al. Elevated plasma phenylalanine predicts mortality in critical patients with heart failure. ESC Heart Fail. 2020, 7, 2884–2893.
- Chen, X.; Li, H.Y.; Hu, X.M.; Zhang, Y.; Zhang, S.Y. Current understanding of gut microbiota alterations and related therapeutic intervention strategies in heart failure. Chin. Med. J. 2019, 132, 1843–1855.
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.; Org, E.; Sheehy, B.; Britt, E.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585.
- Wang, Z.; Roberts, A.B.; Buffa, J.A.; Levison, B.S.; Zhu, W.; Org, E.; Gu, X.; Huang, Y.; Zamanian-Daryoush, M.; Culley, M.K.; et al. Non-lethal Inhibition of Gut Microbial Trimethylamine Production for the Treatment of Atherosclerosis. Cell 2015, 163, 1585–1595.
- Yang, W.; Zhang, S.; Zhu, J.; Jiang, H.; Jia, D.; Ou, T.; Qi, Z.; Zou, Y.; Qian, J.; Sun, A.; et al. Gut microbe-derived metabolite trimethylamine N-oxide accelerates fibroblast-myofibroblast differentiation and induces cardiac fibrosis. J. Mol. Cell. Cardiol. 2019, 134, 119–130.
- Hinderer, S.; Schenke-Layland, K. Cardiac fibrosis—A short review of causes and therapeutic strategies. Adv. Drug Deliv. Rev. 2019, 146, 77–82.
- Salzano, A.; Cassambai, S.; Yazaki, Y.; Israr, M.Z.; Bernieh, D.; Wong, M.; Suzuki, T. The Gut Axis Involvement in Heart Failure: Focus on Trimethylamine N-oxide. Cardiol. Clin. 2022, 40, 161–169.
- Xu, J.; Yang, Y. Gut microbiome and its meta-omics perspectives: Profound implications for cardiovascular diseases. Gut Microbes. 2021, 13, 1936379.
- Guan, X.; Sun, Z. The Role of Intestinal Flora and Its Metabolites in Heart Failure. Infect. Drug Resist. 2023, 16, 51–64.
- Mayerhofer, C.C.K.; Kummen, M.; Holm, K.; Broch, K.; Awoyemi, A.; Vestad, B.; Storm-Larsen, C.; Seljeflot, I.; Ueland, T.; Bohov, P.; et al. Low fibre intake is associated with gut microbiota alterations in chronic heart failure. ESC Heart Fail. 2020, 7, 456–466.
- Tuteja, S.; Ferguson, J.F. Gut Microbiome and Response to Cardiovascular Drugs. Circ. Genom. Precis Med. 2019, 12, 421–429.
- Kim, D.-H. Gut microbiota-mediated drug-antibiotic interactions. Drug Metab. Dispos. 2015, 43, 1581–1589.
- Sousa, T.; Paterson, R.; Moore, V.; Carlsson, A.; Abrahamsson, B.; Basit, A.W. The gastrointestinal microbiota as a site for the biotransformation of drugs. Int. J. Pharm. 2008, 363, 1–25.
- Zhernakova, A.; Kurilshikov, A.; Bonder, M.J.; Tigchelaar, E.F.; Schirmer, M.; Vatanen, T.; Mujagic, Z.; Vila, A.V.; Falony, G.; Vieira-Silva, S.; et al. Population-based metagenomics analysis reveals markers for gut microbiome composition and diversity. Science 2016, 352, 565–569.
- Jackson, M.A.; Verdi, S.; Maxan, M.E.; Shin, C.M.; Zierer, J.; Bowyer, R.C.E.; Martin, T.; Williams, F.M.K.; Menni, C.; Bell, J.T.; et al. Gut microbiota associations with common diseases and prescription medications in a population-based cohort. Nat. Commun. 2018, 9, 2655.
- Haiser, H.J.; Gootenberg, D.B.; Chatman, K.; Sirasani, G.; Balskus, E.P.; Turnbaugh, P.J. Predicting and manipulating cardiac drug inactivation by the human gut bacterium eggerthella lenta. Science 2013, 341, 295–298.
- Saha, J.R.; Butler, V.P., Jr.; Neu, H.C.; Lindenbaum, J. Digoxin-inactivating bacteria: Identification in human gut flora. Science 1983, 220, 325–327.
- Kim, I.S.; Yoo, D.H.; Jung, I.H.; Lim, S.; Jeong, J.J.; Kim, K.A.; Bae, O.N.; Yoo, H.H.; Kim, D.H. Reduced metabolic activity of gut microbiota by antibiotics can potentiate the antithrombotic effect of aspirin. Biochem. Pharmacol. 2016, 122, 72–79.
- Mortensen, B.; Murphy, C.; O’Grady, J.; Lucey, M.; Elsafi, G.; Barry, L.; Westphal, V.; Wellejus, A.; Lukjancenko, O.; Eklund, A.; et al. Bifidobacteriumbreve Bif195 Protects Against Small-Intestinal Damage Caused by Acetylsalicylic Acid in Healthy Volunteers. Gastroenterology 2019, 157, 637–646.e4.
- Liu, Y.; Song, X.; Zhou, H.; Zhou, X.; Xia, Y.; Dong, X.; Zhong, W.; Tang, S.; Wang, L.; Wen, S.; et al. Gut microbiome associates with lipid-lowering effect of rosuvastatin in vivo. Front. Microbiol. 2018, 9, 530.
- Khan, T.J.; Ahmed, Y.M.; Zamzami, M.A.; Siddiqui, A.M.; Khan, I.; Baothman, O.A.S.; Mehanna, M.G.; Kuerban, A.; Kaleemuddin, M.; Yasir, M. Atorvastatin treatment modulates the gut microbiota of the hypercholesterolemic patients. Omics J. Integr. Biol. 2018, 22, 154–163.
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563.
- Merra, G.; Noce, A.; Marrone, G.; Cintoni, M.; Tarsitano, M.G.; Capacci, A.; De Lorenzo, A. Influence of Mediterranean Diet on Human Gut Microbiota. Nutrients 2020, 13, 7.
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016, 65, 1812–1821.
- Lopez-Garcia, E.; Rodriguez-Artalejo, F.; Li, T.Y.; Fung, T.T.; Li, S.; Willett, W.C.; Rimm, E.B.; Hu, F.B. The Mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. Am. J. Clin. Nutr. 2014, 99, 172–180.
- Marques, F.Z.; Nelson, E.; Chu, P.Y.; Horlock, D.; Fiedler, A.; Ziemann, M.; Tan, J.K.; Kuruppu, S.; Rajapakse, N.W.; El-Osta, A.; et al. High-Fiber diet and acetate supplementation change the gut microbiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation 2017, 135, 964–977.
- Mamic, P.; Chaikijurajai, T.; Tang, W.H.W. Gut microbiome—A potential mediator of pathogenesis in heart failure and its comorbidities: State-of-the-art review. J. Mol. Cell Cardiol. 2021, 152, 105–117.
- Lam, V.; Su, J.; Koprowski, S.; Hsu, A.; Tweddell, J.S.; Rafiee, P.; Gross, G.J.; Salzman, N.H.; Baker, J.E. Intestinal microbiota determine severity of myocardial infarction in rats. FASEB J. 2012, 26, 1727–1735.
- Ponziani, F.R.; Zocco, M.A.; D’Aversa, F.; Pompili, M.; Gasbarrini, A. Eubiotic properties of rifaximin: Disruption of the traditional concepts in gut microbiota modulation. World J. Gastroenterol. 2017, 23, 4491–4499.
- Chen, M.L.; Yi, L.; Zhang, Y.; Zhou, X.; Ran, L.; Yang, J.; Zhu, J.D.; Zhang, Q.Y.; Mi, M.T. Resveratrol Attenuates Trimethylamine-N-Oxide (TMAO)-Induced Atherosclerosis by Regulating TMAO Synthesis and Bile Acid Metabolism via Remodeling of the Gut Microbiota. mBio 2016, 7, e02210–e02215.
- Conraads, V.M.; Jorens, P.G.; De Clerck, L.S.; Van Saene, H.K.; Ieven, M.M.; Bosmans, J.M.; Schuerwegh, A.; Bridts, C.H.; Wuyts, F.; Stevens, W.J.; et al. Selective intestinal decontamination in advanced chronic heart failure: A pilot trial. Eur. J. Heart Fail. 2004, 6, 483–491.
- Davani-Davari, D.; Negahdaripour, M.; Karimzadeh, I.; Seifan, M.; Mohkam, M.; Masoumi, S.J.; Berenjian, A.; Ghasemi, Y. Prebiotics: Definition, Types, Sources, Mechanisms, and Clinical Applications. Foods 2019, 8, 92.
- Miao, T.; Yu, Y.; Sun, J.; Ma, A.; Yu, J.; Cui, M.; Yang, L.; Wang, H. Decrease in abundance of bacteria of the genus Bifidobacterium in gut microbiota may be related to pre-eclampsia progression in women from East China. Food Nutr. Res. 2021, 65.
