Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Elena Moretti and Version 3 by Rita Xu.
Spermatozoa are highly differentiated cells that produce reactive oxygen species (ROS) due to aerobic metabolism. Below a certain threshold, ROS are important in signal transduction pathways and cellular physiological processes, whereas ROS overproduction damages spermatozoa. Sperm manipulation and preparation protocols during assisted reproductive procedures—for example, cryopreservation—can result in excessive ROS production, exposing these cells to oxidative damage. Human spermatozoa represent an ideal cell model to test numerous compounds in vitro, including antioxidants that can be used as supplements to improve the outcome of these procedures.
- antioxidants
- human sperm in vitro
- oxidative stress
1. Introduction
Infertility is a global health issue. It is defined as the failure to achieve a pregnancy after 12 months or more of regular, unprotected sexual intercourse [1]. It is estimated that 8–12% of couples worldwide are infertile [2] and resort to fertility medical treatment. Both of the partners of a couple can be responsible for non-conception. In at least 50% of cases, a male infertility factor is involved, isolated or in combination with a female factor [3][4][3,4]. There are numerous causes and risk factors contributing to the increasing incidence of male infertility [2]. Many of them share oxidative stress (OS) as a common pathway, including varicocele [5], genitourinary infection and inflammation [6][7][6,7]. In this scenario, assisted fertilisation technologies (ART) represent the treatment of choice for many couples facing infertility problems. The use of these techniques implies gamete handling in the laboratory and the exposure of gametes to atmospheric oxygen. In addition, semen laboratory processing such as centrifugation; cryopreservation; exposure to visible light; and the variation in oxygen tension, pH and temperature [8][9][8,9] enhance the production of reactive oxygen species (ROS).
Spermatozoa are highly differentiated cells that produce ROS as consequence of aerobic metabolism. Below a certain threshold, ROS play a key role in signal transduction pathways and cellular physiological processes. In particular, ROS are necessary for sperm motility, capacitation, the acrosome reaction and oocyte interaction [10][11][10,11]. On the contrary, ROS overproduction and the consequent antioxidant imbalance can damage the cellular structure [12], including the membrane, particularly rich in polyunsaturated fatty acids (PUFA), and molecules such as DNA and proteins [13][14][15][16][13,14,15,16].
Assuming that external laboratory conditions are optimal, a strategy to minimise OS during sperm manipulation can include the treatment of the patients with antioxidants even though the real efficacy of in vivo supplementation is still debated [16][17][18][16,17,18]. Another very interesting strategy includes the supplementation of media with antioxidants. Many in vitro studies have investigated the scavenging ability of antioxidant compounds against OS induced in human sperm [9] and many other studies have successfully used antioxidants to supplement media applied in semen cryopreservation [19][20][19,20].
Human spermatozoa represent a model for an in vitro study because they are motile, and the motility is a parameter that is easy to evaluate; they are nearly transcriptionally and translationally silenced; they do not have DNA-repair activity; and they lack intracellular antioxidant protection. Thus, they depend on and are deeply influenced by the external environment.
2. Structure of Human Spermatozoa
Human spermatozoa are highly differentiated and polarised cells made up of a head and a flagellum joined by a connecting piece, all of which is enveloped by the plasma membrane (Figure 1).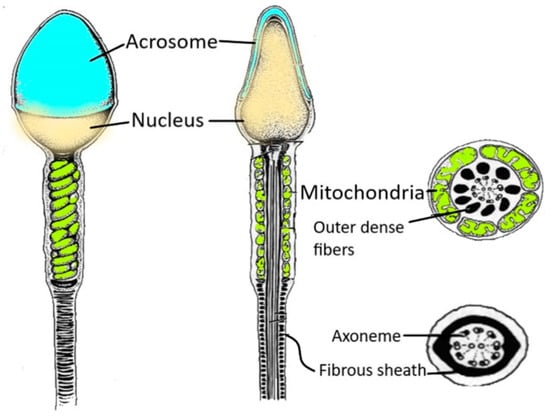
Figure 1. Spermatozoon structure. The figure shows the various regions of a human spermatozoon. Starting from the head region, it is possible to distinguish the acrosome and the nucleus. The sperm flagellum contains the axoneme and periaxonemal structures such as outer dense fibres and a fibrous sheath.
3. Sperm and ROS: An Ambivalent Relationship
Spermatozoa represent a perfect example of the oxygen paradox [36][37][48,49]. Indeed, oxygen homeostasis and the maintenance of a redox steady state are critical for spermatozoa. Spermatozoa generate ROS because they need them for several physiological processes (Figure 2). On the other hand, when ROS production overcomes the antioxidant defences, there are detrimental effects to the sperm membrane, proteins and DNA (Figure 2), which have a negative impact on male fertility [38][50].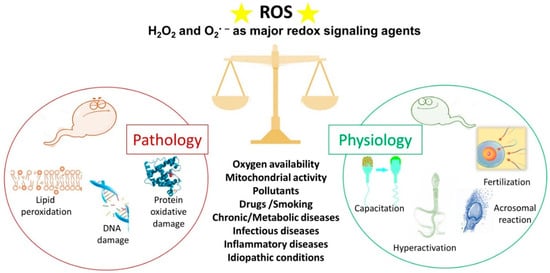
Figure 2. The double face of reactive oxygen species (ROS). Under physiological conditions, ROS regulate the sperm mechanisms involved in capacitation, hyperactivation, the acrosome reaction and fertilisation. On the contrary, some pathophysiological conditions can increase ROS levels over the physiological threshold, generating a condition of oxidative stress that leads to lipid peroxidation, DNA damage and protein oxidative damage. The stars represent ROS.
3.1. ROS and Sperm Physiology
ROS play an important role in sperm physiology because they regulate several intracellular pathways, thus modulating the activation of different transcription factors [38][39][40][50,51,52]. First, ROS are responsible for the stability and compaction of sperm chromatin during epididymal transit and storage. They act as oxidising agents and allow for the formation of disulphide bonds between cysteine residues of protamines, arginine-rich proteins that replace histones during spermiogenesis. Chromatin folding is a crucial event in protecting the paternal genome as the spermatozoa travel through the female reproductive tract [27]. One of the most important roles of ROS in sperm physiology (Figure 2) concerns the process of capacitation by which spermatozoa undergo dramatic changes in the membrane composition and acquire hyperactivated motility, leading to the acrosome reaction and fertilisation [41][42][53,54]. The molecular processes behind capacitation include an increase in pH, Ca2+ and HCO3− influx, efflux of cholesterol from the plasma membrane, an increase in cyclic adenosine monophosphate (cAMP) concentration; and protein hyper-phosphorylation [43][44][55,56]. During capacitation, the concentration of O2•−, H2O2, nitric oxide and peroxynitrite increase progressively. These ROS stimulate the activation of adenylate cyclase that drives the increase in cAMP. This second messenger activates protein kinase A (PKA) that triggers a massive tyrosine phosphorylation cascade, inhibiting tyrosine phosphatase [45][46][57,58]. Redox signalling occurs alongside modification of thiol groups of proteins of the plasma membrane and the inner sperm compartments [41][53]. As a part of the capacitation process, the hyperactivated motility triggered by calcium signalling [47][59] is characterised by a high amplitude and extremely asymmetrical beating pattern of sperm flagellum, as well as lateral head displacement. These motility modifications are dependent on ROS-mediated tyrosine phosphorylation of flagellar protein and are needed to make spermatozoa that can penetrate the cumulus oophorous and zona pellucida and fertilise the oocyte [48][49][60,61]. In addition, the acrosome reaction, the universal requisite for sperm–egg fusion, is influenced by ROS [50][62] that increase membrane fluidity. In fact, spermatozoa exposed to H2O2 show an enhanced acrosome reaction and an increased ability to fuse with oocyte [51][63]. Finally, the involvement of ROS in sperm function and physiology is supported by the observations that antioxidants can alter sperm maturation and, in particular, catalase or superoxide dismutase can inhibit sperm capacitation and the acrosome reaction [52][64].3.2. ROS and Sperm Pathology
In recent decades, OS has emerged as a one of the main causes of altered sperm function [53][65]. Spermatozoa represent an easy target for free radical attack due to the high content of unsaturated fatty acids in their membranes, the limited ability to repair DNA damage and the virtual lack of cytoplasm. Moreover, spermatozoa are poor in antioxidant enzymes such as superoxide dismutase, catalase and glutathione peroxidase, as well as peroxiredoxins [54][66] that protect most cells from oxidative damage. To compensate the scarce presence of cellular antioxidants, the seminal plasma is rich in antioxidant enzymes and radical scavengers, among them glutathione peroxidase, glutathione-S-transferase, catalase and superoxide dismutase [55][67]. In addition, other hydrophilic compounds as uric acid, hypotaurine, tyrosine, polyphenols, vitamin C, ergothioneine and glutathione, and hydrophobic scavengers as trans-retinoic acids, trans-retinols, α-tocopherol, carotenoids and coenzyme Q10 are present [56][68]. The antioxidant properties of seminal plasma are important to balance the presence of ROS that are not just from the physiological production by spermatozoa. Human semen contain various amounts of immature spermatozoa, germinal cells, leucocytes, macrophages and epithelial cells. Among them, the main contributors to OS are leucocytes and immature spermatozoa with large cytoplasmic residues, but in physiological conditions, the redox balance is maintained by antioxidants contained in seminal plasma [57][69]. However, leucocytospermia occurs when the peroxidase-positive leucocyte concentration exceeds 1 × 106/mL [1]. In this pathology, leucocytes produce a hundred times as much ROS as what they would in physiological conditions and the antioxidant power of the seminal plasma is not sufficient to counteract free radicals, leading to OS [58][70]. Immature spermatozoa fail to extrude the cytoplasm during maturation and the residual cytoplasm allows for the production of NADPH from glucose-6-phosphate (G6PDH) via the hexose monophosphate shunt [59][60][71,72]. NADPH generates ROS by using two different pathways: via NADPH oxidase, a membrane bound enzyme that produces the O2•− by oxygen, and via NADPH dehydrogenase, which is responsible for redox reactions in the mitochondria. The enhanced ROS production triggered by immature spermatozoa is responsible for OS propagation to maturing normal spermatozoa during epididymal transit [61][73]. During recent decades, a growing body of evidence has revealed the role of altered redox balance in seminal plasma, sperm alterations and male infertility [12][60][62][12,72,74]. OS is enhanced in situations when non-physiological ROS levels overwhelm the natural scavenger systems. These situations can be represented by primary pathologies affecting the male reproductive system, including varicocele [63][75], bacterial and viral infections, inflammation and leucocytospermia; chronic pathologies such as diabetes and cancer [60][64][72,76]; and environmental and lifestyle factors such as use of drugs, smoking, pollution and radiation (Figure 2). In these conditions, the unconjugated double bonds of PUFA in the sperm membrane are attacked by ROS, producing lipid hydroperoxides and its secondary decomposition product, aldehydes [59][71]. These highly reactive by-products produced by lipid peroxidation react with proteins and DNA and alter the proteins of the electron transport chain to induce mitochondrial dysfunction, enhancing the production of mitochondrial ROS in a self-perpetrating mechanism [9][59][65][9,71,77]. The most evident effect of OS and lipid peroxidation on spermatozoa is the loss of motility by inhibiting energy generation and the decrease in vitality as observed when sperm are frozen and thawed, two processes that boost ROS production [59][71]. The relevance of lipid oxidative damage to sperm conditions has been highlighted by the detection, quantification or immunolocalization of the specific end products of lipid peroxidation (aldehydes and oxygenated metabolites of PUFA) [66][67][78,79]. OS is a major cause of DNA damage in mammalian spermatozoa. Aitken and De Iuliis [68][80] proposed a two-step mechanism for the origin of oxidative DNA damage in spermatozoa. The first phase occurs during spermiogenesis and leads to defective protamination and compaction of sperm chromatin, making DNA more vulnerable to ROS attack. In normal conditions, chromatin compaction is mandatory to protect paternal DNA—this stabilisation makes the spermatozoa resistant to oxidative damage. The second phase is referred to a direct oxidative insult on the DNA due to increased ROS generation by sperm and a loss of extracellular antioxidant protection. The evident ROS effects on sperm nuclear DNA include DNA fragmentation, chromatin cross-linking, base-pair modifications and chromosomal microdeletions [11]. In addition, paternal aging plays a negative effect on sperm parameters and induces a ROS-related DNA fragmentation. These alterations negatively influence the reproductive outcome and offspring health documented for cancer, genetic and congenital diseases, chromosomal alterations and others [69][81].4. Human Spermatozoa as a Model for In Vitro Studies
There are many reasons why human spermatozoa represent a model for in vitro studies (Figure 3). First, the easy collection of spermatozoa from fertile men can guarantee abundant cellular material. Spermatozoa are differentiated cells with features and specific functions that enable them to reach the oocyte and to fertilise it. The first peculiar characteristic of spermatozoa is their motility, which enables them to reach and fertilise the oocyte. This motility is guaranteed by the ability to obtain energy by both mitochondrial oxidative phosphorylation and glycolysis, the enzymes for which are located along the FS [33].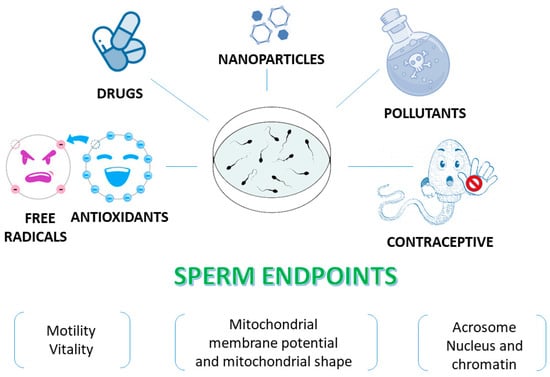
Figure 3. Human sperm as an in vitro model to test various compounds. Sperm endpoints such as motility, vitality, mitochondrial membrane potential, the acrosome status and DNA integrity can be evaluated when human spermatozoa are used as an in vitro model to test effects of toxic compounds, natural extracts and molecules.
