
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Claire Monge | + 1095 word(s) | 1095 | 2021-05-19 12:01:44 | | | |
| 2 | Claire Monge | + 1095 word(s) | 1095 | 2021-05-19 14:46:58 | | | | |
| 3 | Nora Tang | + 1095 word(s) | 1095 | 2021-05-20 02:51:25 | | |
Video Upload Options
Respiratory viral infections have been a leading cause of morbidity and mortality worldwide. Despite massive advancements in the virology field, no specific treatment exists for most respiratory viral infections. Approved therapies against respiratory viruses rely almost exclusively on synthetic drugs that have potential side effects, restricting their use.
1. Introduction
The respiratory tract is one of the main portals of entry for human viruses. Respiratory tract infections lead to enormous health and economic burdens and cause severe outcomes, including hospitalization and death, especially in developing countries [1][2][3][4]. In 2013, the WHO’s Battle against Respiratory Viruses initiative (BRaVe) recognized acute respiratory infection as a major global public health issue [5]. Unfortunately, nearly ten years later, respiratory infections are still a global health security threat, exemplified by the recent coronavirus outbreak in 2020 [3].
Viral respiratory tract infections (vRTIs) can be due to several families of viruses, such as picornaviruses (human rhinoviruses (HRV)), coronaviruses (CoV), ortho- and paramyxoviruses (influenza virus, parainfluenza virus (PIV or HPIV for human), human metapneumovirus (HMPV) and respiratory syncytial virus (RSV)), adenoviruses and herpes viruses [1][6]. Since the beginning of the 21st century, the world has faced several episodes of epidemic or pandemic respiratory illnesses due to the emergence of new respiratory viruses, including severe acute respiratory syndrome coronavirus (SARS-CoV) in 2003, H1N1 influenza in 2009, avian influenza A viruses, such as H5N1 and H7N9, middle east respiratory syndrome coronavirus (MERS-CoV) in 2012, and the recent SARS-CoV-2 in 2019. These reemerging and highly pathogenic pandemic viruses have been one of the leading causes of morbidity and mortality worldwide and are known to cause acute respiratory infections in all age groups globally and all year round [7][8][9][10]. In 2017, it was estimated that more than 54 million lower respiratory tract infection (LRI) episodes were due to influenza worldwide, leading to more than 9 million hospitalizations and 145,000 deaths among all ages [11]. Even though all age groups are susceptible to influenza, children up to 5 years, pregnant women, the elderly and individuals with specific chronic medical conditions are considered at-risk populations. Alike influenza-virus-associated infections, RSV caused around 1.5 million episodes of acute LRIs in 2015 in the elderly, specifically those aged 50–64 years [12]. Although other respiratory viruses, such as adenovirus and rhinovirus, cause lower mortality, they are associated with significant morbidity, which causes a huge economic burden. Increased respiratory viral infections worldwide necessitate searching for safe and effective antiviral drugs to counteract these massive healthcare problems.
2. Symptoms of Respiratory Viral Infections and Approved Therapies
The transmission of viral pathogens occurs mainly by the respiratory route, characterized by aerosol emission or droplets primarily during a cough or sneezing episode [6][13]. In most cases, these vRTIs are limited to the upper respiratory tract but can lead to acute lower respiratory tract infections as well, particularly in the case of RSV, influenza virus, PIV and SARS-CoV2 [14][15][16]. The symptoms of viral respiratory infections can include congestion of either the nasal sinuses or lungs, runny nose, cough, sore throat, body aches, fatigue (Figure 1).
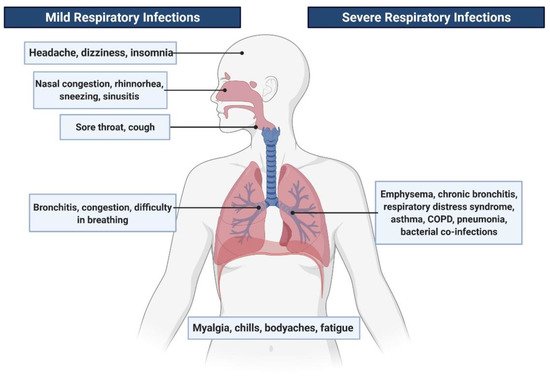
Figure 1. Symptoms related to viral respiratory tract infections.
In the most severe cases, symptoms can be chills, difficulty in breathing, dizziness, bronchiolitis, asthma exacerbations, pneumonia, respiratory distress syndromes and chronic obstructive pulmonary disease (COPD) [5][17]. The propagation of several respiratory viruses has also been reported from the respiratory tract to the central nervous system (CNS) [18].
Although some viruses may be associated with defined clinical signs and symptoms, there is also some intersection in the correspondence of pathology and the responsible pathogen. It is thus difficult to define viral respiratory diseases because the symptoms related to vRTI commonly overlap [6]. For example, the common cold may originate from different etiologic agents, such as rhinoviruses or coronaviruses. Similarly, influenza may be caused by the influenza virus, but also by RSV, Haemophilus influenzae type b, or Streptococcus pneumoniae [11].
Symptomatic therapies or antiviral medications are still the major tools to treat vRTIs [19] as vaccines are currently not yet available for most of the respiratory viruses [20] except against influenza, adenovirus and more recently, against SARS-CoV-2. However, it is also important to notice that such vaccines will face several specific hurdles: (i) they could be restricted to some countries and dedicated personnel, as evidenced by the adenovirus vaccine available only to military personnel in the US; (ii) their mild efficacy (from 30% to 60% for the influenza vaccine) and need for annual revaccination due to emerging new variants [6] and (iii) high-cost and need for specific cold chain suppliers as observed with recent mRNA vaccines against SARS-CoV-2. Although developing vaccine strategies against the respiratory diseases still remain an outstanding priority, it questions the availability of these vaccines in developing countries in a timely manner, where cost-effective antiviral therapies could be preferred.
2.1. Symptomatic Treatment
For most respiratory viruses, the guidelines for their treatment and management can differ widely according to the patient status or the country [21]. Most vRTIs medications are not antiviral agents but rather target the short-term relief of symptoms, such as nasal decongestants, antipyretics/analgesics, antitussives or expectorants. However, though rare, adverse effects could occur, especially in young children [6][22]. Therefore, using targeted therapeutic options against these respiratory viruses is highly required.
2.2. Antiviral Medication
In general practice, the treatment is done with nonspecific antiviral agents, e.g., cidofovir against adenovirus infections, ribavirin against influenza, and palivizumab for protection against RSV (Table 1). The use of adamantane drugs and neuraminidase inhibitors (oseltamivir, laninamivir, peramivir and zanamivir) has been also reported in the literature against influenza [6][23].
Table 1. Some approved synthetic antiviral agents and natural seaweed polysaccharides against respiratory viruses.
| * FDA/EMA Approved Antivirals | ||||
|---|---|---|---|---|
| Respiratory Virus | Synthetic Antivirals | Natural Seaweed Polysaccharides | Vaccine | Reference |
| Human rhinovirus | No | Iota-carrageenan | No | |
| Adenovirus | Cidofovir, ganciclovir, ribavirin | No | Yes (not accessible to all) |
[24] |
| Human metapneumovirus | No | No | No | |
| Parainfluenza virus | No | No | No | |
| Influenza virus | Ribavirin, amantadine | No | Yes | [23] |
| Rimantadine, zanamivir | ||||
| Oseltamivir, peramivir | ||||
| Laninamivir | ||||
| Respiratory syncytial virus | Ribavarin, palivizumab | No | No | [25][26] |
| SARS CoV-2 | Remdesivir | No | Yes | [27] |
| HCoV-OC43 | No | No | No | |
* FDA: US Food and Drug Administration, EMA: European Medicines Agency.
Although active research is ongoing to develop safe and efficient antiviral agents against respiratory viruses [28], their clinical effectiveness is still under investigation, and their use is limited to high-risk populations, such as immunocompromised patients [29]. These antiviral agents lack targeted therapeutic activity towards respiratory viruses. Their cost, as well as associated side effects, restrict their use. Moreover, the emergence of viral resistance remained a major limiting factor for the general population and emerged as a major public health problem [30][31]. Furthermore, using antibiotics is still widely practiced in certain parts of the world, which leads to their misuse [32]. Due to the lack of optimal medication and effective vaccines, the search for alternative natural therapies, such as sulfated marine polysaccharides, is indispensable.
References
- Tang, J.W.; Lam, T.T.; Zaraket, H.; Lipkin, W.I.; Drews, S.J.; Hatchette, T.F.; Heraud, J.M.; Koopmans, M.P.; Abraham, A.M.; Baraket, A.; et al. Global Epidemiology of Non-Influenza RNA Respiratory Viruses: Data Gaps and a Growing Need for Surveillance. Lancet Infect. Dis. 2017, 17, e320–e326.
- Watkins, K. Emerging Infectious Diseases: A Review. Curr. Emerg. Hosp. Med. Rep. 2018, 6, 86–93.
- Patchett, D.; Yang, J.; Northern, J.; Salinas, M.; Bauer, B.A. Viral Respiratory Infections: An Ounce of Prevention Is Worth a Pound of Cure. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 480–485.
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review. Int. J. Surg. 2020, 78, 185–193.
- World Health Organization. Research Needs for the Battle against Respiratory Viruses (BRaVe). Future Virol. 2013, 1–42.
- Van Doorn, H.R.; Yu, H. Viral Respiratory Infections, 2020, 10th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2020.
- Al-Tawfik, J.A.; Memish, Z.A. Emerging Respiratory Viral Infections: MERS-CoV and Influenza. Lancet Respir. Med. 2014, 2, 23–25.
- Zhang, N.; Wang, L.; Deng, X.; Liang, R.; Su, M.; He, C.; Hu, L.; Su, Y.; Ren, J.; Yu, F.; et al. Recent Advances in the Detection of Respiratory Virus Infection in Humans. J. Med. Virol. 2020, 92, 408–417.
- Islam, M.T.; Sarkar, C.; El-Kersh, D.M.; Jamaddar, S.; Uddin, S.J.; Shilpi, J.A.; Mubarak, M.S. Natural Products and Their Derivatives against Coronavirus: A Review of the Non-Clinical and Pre-Clinical Data. Phyther. Res. 2020, 34, 2471–2492.
- Moriyama, M.; Hugentobler, W.J.; Iwasaki, A. Seasonality of Respiratory Viral Infections. Annu. Rev. Virol. 2020, 7, 83–101.
- Troeger, C.E.; Blacker, B.F.; Khalil, I.A.; Zimsen, S.R.M.; Albertson, S.B.; Abate, D.; Abdela, J.; Adhikari, T.B.; Aghayan, S.A.; Agrawal, S.; et al. Mortality, Morbidity, and Hospitalisations Due to Influenza Lower Respiratory Tract Infections, 2017: An Analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2019, 7, 69–89.
- Shi, T.; Denouel, A.; Tietjen, A.K.; Campbell, I.; Moran, E.; Li, X.; Campbell, H.; Demont, C.; Nyawanda, B.O.; Chu, H.Y.; et al. Global Disease Burden Estimates of Respiratory Syncytial Virus-Associated Acute Respiratory Infection in Older Adults in 2015: A Systematic Review and Meta-Analysis. J. Infect. Dis. 2020, 222, S577–S583.
- Herfst, S.; Böhringer, M.; Karo, B.; Lawrence, P.; Lewis, N.S.; Mina, M.J.; Russell, C.J.; Steel, J.; de Swart, R.L.; Menge, C. Drivers of Airborne Human-to-Human Pathogen Transmission. Curr. Opin. Virol. 2017, 22, 22–29.
- Shi, T.; McLean, K.; Campbell, H.; Nair, H. Aetiological Role of Common Respiratory Viruses in Acute Lower Respiratory Infections in Children under Five Years: A Systematic Review and Meta–Analysis. J. Glob. Health 2015, 5, 1–10.
- Buetti, N.; Wicky, P.H.; Le Hingrat, Q.; Ruckly, S.; Mazzuchelli, T.; Loiodice, A.; Trimboli, P.; Forni Ogna, V.; de Montmollin, E.; Bernasconi, E.; et al. SARS-CoV-2 Detection in the Lower Respiratory Tract of Invasively Ventilated ARDS Patients. Crit. Care 2020, 24, 4–9.
- Murphy, K. SARS CoV-2 Detection from Upper and Lower Respiratory Tract Specimens: Diagnostic and Infection Control Implications. Chest 2020, 158, 1804–1805.
- Linden, D.; Guo-Parke, H.; Coyle, P.V.; Fairley, D.; McAuley, D.F.; Taggart, C.C.; Kidney, J. Respiratory Viral Infection: A Potential “Missing Link” in the Pathogenesis of COPD. Eur. Respir. Rev. 2019, 28, 1–14.
- Desforges, M.; Le Coupanec, A.; Dubeau, P.; Bourgouin, A.; Lajoie, L.; Dubé, M.; Talbot, P.J. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses 2019, 12, 14.
- Brendish, N.J.; Clark, T.W. Antiviral Treatment of Severe Non-Influenza Respiratory Virus Infection. Curr. Opin. Infect. Dis. 2017, 30, 573–578.
- Pagarete, A.; Ramos, A.S.; Puntervoll, P.; Allen, M.J.; Verdelho, V. Antiviral Potential of Algal Metabolites—A Comprehensive Review. Mar. Drugs 2021, 19, 94.
- Peghin, M.; Danziger-Isakov, L. Prevention and Treatment of Respiratory Virus Infection. In Infectious Diseases in Solid-Organ Transplant Recipients; Manuel, O., Ison, M., Eds.; Springer: Cham, Switzerland, 2019.
- Papadopoulos, N.G.; Megremis, S.; Kitsioulis, N.A.; Vangelatou, O.; West, P.; Xepapadaki, P. Promising Approaches for the Treatment and Prevention of Viral Respiratory Illnesses. J. Allergy Clin. Immunol. 2017, 140, 921–932.
- Shie, J.J.; Fang, J.M. Development of Effective Anti-Influenza Drugs: Congeners and Conjugates—A Review. J. Biomed. Sci. 2019, 26, 1–20.
- Dodge, M.J.; MacNeil, K.M.; Tessier, T.M.; Weinberg, J.B.; Mymryk, J.S. Emerging Antiviral Therapeutics for Human Adenovirus Infection: Recent Developments and Novel Strategies. Antiviral Res. 2021, 188, 105034.
- Boyoglu-Barnum, S.; Tripp, R.A. Up-to-Date Role of Biologics in the Management of Respiratory Syncytial Virus. Expert Opin. Biol. Ther. 2020, 20, 1073–1082.
- Kalergis, A.M.; Soto, J.A.; Gálvez, N.M.S.; Andrade, C.A.; Fernandez, A.; Bohmwald, K.; Bueno, S. Pharmacological Management of Human Respiratory Syncytial Virus Infection. Expert Opin. Pharmacother. 2020, 21, 2293–2303.
- Vivekanandhan, K.; Shanmugam, P.; Barabadi, H.; Arumugam, V.; Daniel Raj Daniel Paul Raj, D.; Sivasubramanian, M.; Ramasamy, S.; Anand, K.; Boomi, P.; Chandrasekaran, B.; et al. Emerging Therapeutic Approaches to Combat COVID-19: Present Status and Future Perspectives. Front. Mol. Biosci. 2021, 8, 1–10.
- Beigel, J.H.; Nam, H.H.; Adams, P.L.; Krafft, A.; Ince, W.L.; El-Kamary, S.S.; Sims, A.C. Advances in Respiratory Virus Therapeutics—A Meeting Report from the 6th Isirv Antiviral Group Conference. Antiviral Res. 2019, 167, 45–67.
- Shahani, L.; Ariza-Heredia, E.J.; Chemaly, R.F. Antiviral Therapy for Respiratory Viral Infections in Immunocompromised Patients. Expert Rev. Anti. Infect. Ther. 2017, 15, 401–415.
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Prim. 2018, 4, 1–21.
- Krylova, N.V.; Ermakova, S.P.; Lavrov, V.F.; Leneva, I.A.; Kompanets, G.G.; Iunikhina, O.V.; Nosik, M.N.; Ebralidze, L.K.; Falynskova, I.N.; Silchenko, A.S.; et al. The Comparative Analysis of Antiviral Activity of Native and Modified Fucoidans from Brown Algae Fucus Evanescens in Vitro and in Vivo. Mar. Drugs 2020, 18, 224.
- Alfayate Miguélez, S.; Garcia-Marcos, L. Rational Use of Antimicrobials in the Treatment of Upper Airway Infections. J. Pediatr. 2020, 96, 111–119.




