
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Lin Ang | + 1337 word(s) | 1337 | 2021-05-18 09:48:56 | | | |
| 2 | Karina Chen | Meta information modification | 1337 | 2021-05-18 11:30:00 | | |
Video Upload Options
Osteoarthritis (OA) is a common joint disease, which is linked to joint degeneration, loss of cartilage, and alterations of the subchondral bone, and mainly affects the hands, knees, and hips. OA is a highly predominant health condition, which has affected over 260 million people worldwide, and it is becoming even more common due to the combined effects of aging and obesity. OA is even more problematic as it is associated with pain, disability, and personal and economic burden. This review aims to evaluate the effectiveness of acupressure as a treatment method for osteoarthritis.
1. Introduction
There are many treatment approaches for the management of osteoarthritis, and they are generally nonpharmacologic, pharmacologic, surgical, or complementary and alternative approaches [1]. In particular, clinical practice guidelines for hip and knee OA suggest interventions such as patient education, exercise, and weight management as first-line treatments, pharmacological therapies and other therapies as second-line treatment, and surgical interventions for replacement as third-line treatment [2]. The complementary and alternative approaches, including acupuncture, yoga, manual therapy, and electrotherapy, are recommended for the OA treatment by the National Clinical Guideline Centre in United Kingdom and the American Academy of Orthopedic Surgeons (AAOS) [3]. Among the complementary and alternative options for the treatment of OA, the clinical evidence of dry needling [4], moxibustion [5], and yoga [6] have been systematically evaluated, but the clinical evidence of acupressure for OA treatment has not been systematically examined yet.
Acupressure is a non-invasive and cost-efficient medical approach and involves applying pressure to the acupoints or meridian points as practiced in Chinese Medicine [7]. Acupressure has been used for various purposes. Previous systematic reviews have investigated the efficacy or the impact of acupressure as a sole intervention on pain [8], low back pain [7][9], labor or labor pain [10][11][12], neck pain syndrome [13], sleep quality, or sleep disorders [14][15][16], promoting the health of older adults [17], respiratory allergic diseases [18], postoperative gastrointestinal symptoms [19], chemotherapy-induced nausea and vomiting [20], primary dysmenorrhea [21][22][23], anxiety [24], neurological disorders [25], and symptom management [26][27][28]; and other reviews considered acupressure as a complementary intervention with acupuncture on cancer pain [29], cancer-related fatigue [30], weight reduction [31], uremic pruritus [32], premenstrual syndrome [33], and labor pain [34].
This review aims to add to the existing literature on acupressure as a treatment method for osteoarthritis by systematically reviewing clinical trials for its clinical efficacy. Fourteen electronic databases were searched from the date of inception until 16 March 2021, for eligible studies. Studies comparing acupressure with sham acupuncture, no intervention or conventional intervention were eligible for inclusion. The risk of bias of the included studies was assessed using the Cochrane Collaboration’s Risk of Bias Assessment tool Version 2.0. A total of eight trials were included in this review, focusing on the seven trials investigating knee osteoarthritis. The risk of bias is judged as low in only two trials and concerning in the remaining six trials.
2. Research findings
2.1. Primary Outcomes
Pain
Acupressure vs. sham acupressure
Three RCTs [35][36][37] compared acupressure with sham acupressure, where one trial [35] reported that acupressure has positive effect in reducing pain and two trials [36][37] reported otherwise. The meta-analysis showed that acupressure has equivalent effect on reducing pain (n = 174, MD −1.93, CI 95%: −4.38 to 0.51, p = 0.12, I2 = 87%, Figure 3A), as compared to sham acupressure.
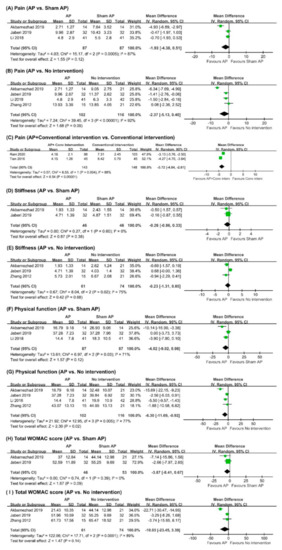
Figure 3. Forest plot of (A) pain (acupressure vs. sham acupressure); (B) pain (acupressure vs. no intervention); (C) pain (acupressure plus conventional intervention vs. conventional intervention) (D) stiffness (acupressure vs. sham acupressure) (E) stiffness (acupressure vs. no intervention); (F) physical function (acupressure vs. sham acupressure); (G) physical function (acupressure vs. no intervention); (H) total WOMAC score (acupressure vs. sham acupressure); (I) total WOMAC score (acupressure vs. no intervention). AP: acupressure; CI: conventional intervention.
Acupressure vs. no intervention
Of the four RCTs [35][36][37][38] comparing acupressure with no intervention, three trials [35][36][37] reported that acupressure has positive effect in reducing pain and one trial [38] reported otherwise. The meta-analysis showed that acupressure has equivalent effect on reducing pain (n = 218, MD −2.37, CI 95%: −5.13 to 0.40, p = 0.09, I2 = 92%, Figure 3B), as compared to no intervention.
Acupressure plus conventional intervention vs. conventional intervention
Two RCTs [39][40], comparing acupressure complementing conventional intervention with conventional intervention, reported that acupressure has superior effect in reducing pain. The pooled results also showed similar results (n = 291, MD −3.72, 95% CI: −4.84 to −2.61, p < 0.00001, I2 = 88%, Figure 3C), where acupressure as complementary intervention has superior effect in reducing pain compared to conventional intervention alone.
Acupressure only vs. conventional intervention
One RCT [40] evaluated the effectiveness of acupressure alone in comparison with conventional intervention and showed superior effect in reducing pain (n = 90, MD 5.44, 95% CI: 5.06 to 5.82, p < 0.00001).
Acupressure only vs. health education
One RCT [41] evaluated the effectiveness of acupressure alone in comparison with health education and showed favorable effect in reducing pain (n = 35, MD 0.54, 95% CI: 0.07 to 1.01, p = 0.03).
Stiffness
Acupressure vs. sham acupressure
Two RCTs [35][36] compared acupressure with sham acupressure and reported equivalent effect in relieving stiffness for both groups. The meta-analysis showed that acupressure has failed to show superior effects in relieving stiffness (n = 92, MD −0.26, CI 95%: −0.86 to 0.33, p = 0.38, I2 = 0%, Figure 3D), as compared to sham acupressure.
Acupressure vs. no intervention
Three RCTs [35][36][37][38], comparing acupressure with no intervention, also reported equivalent effect in relieving stiffness for both groups. The meta-analysis presented similar result where acupressure failed to show superior effects in relieving stiffness (n = 135, MD −0.23, CI 95%: −1.31 to 0.85, p = 0.68, I2 = 75%, Figure 3E), as compared to no intervention.
Acupressure only vs. health education
Physical Function
Acupressure vs. sham acupressure
Three RCTs [35][36][37] compared acupressure with sham acupressure, where one trial [35] reported that acupressure has positive effect in improving physical function and two trials [36][37] reported otherwise. The meta-analysis showed that acupressure has equivalent effects on improving physical function (n = 174, MD −4.02, CI 95%: −9.02 to 0.98, p = 0.12, I2 = 71%, Figure 3F), as compared to sham acupressure.
Acupressure vs. no intervention
Of the four RCTs [35][36][37][38] comparing acupressure with no intervention, two trials [35][37] reported that acupressure has positive effect in improving physical function and two trials [36][38] reported otherwise. The meta-analysis showed that acupressure has superior effects (n = 218, MD −6.30, CI 95%: −11.69 to −0.92, p = 0.02, I2 = 77%, Figure 3G), as compared to no intervention.
Acupressure vs. health education
The only RCT [41] comparing acupressure with health education did not show beneficial effects of acupressure in improving physical function (n = 35, MD: −0.85, 95% CI: −2.60 to 0.90, p = 0.34).
WOMAC Total Score
Acupressure vs. sham acupressure
Two RCTs [35][36] compared acupressure with sham acupressure for KOA, where one trial [35] reported that acupressure has positive effect in improving WOMAC total score and the other trial [36] reported otherwise. The meta-analysis showed that acupressure has equivalent effects on improving WOMAC total score (n = 135, MD −3.87, CI 95%: −8.41 to 0.67, p= 0.09, I2 = 0%, Figure 3H), as compared to sham acupressure.
Acupressure vs. no intervention
Of the three RCTs [35][36][38] comparing acupressure with no intervention for KOA, one trial [35] reported that acupressure has positive effect in improving WOMAC total score and two trials [36][38] reported otherwise. The meta-analysis showed that acupressure has no superior effects (n = 218, MD −10.03, CI 95%: −23.45 to 3.39, p = 0.14, I2 = 89%, Figure 3I), as compared to no intervention.
2.2. Secondary Outcomes
QoL
One RCT [38], comparing acupressure with no intervention, investigated the QoL in OA patients using SF-36 and showed equivalent results between both groups. In contrast, another RCT [41] that compared acupressure with health education assessed QoL in OA patients using SF-6d, which is derived from SF-36, and showed that acupressure has a superior effect on increasing the quality of life in OA patients (n = 35, MD: −0.07, 95% CI: −0.09 to −0.05, p < 0.00001).
Adverse Events (AEs)
Four RCTs [37][38][41][40] assessed adverse events in their trials. In terms of the acupressure group, one trial [37] reported broken skin and soreness at simulation site, one trial [41] reported pain and bruising at simulation sites, worsening of knee pain, and pricking pain sensation on the legs, one trial [40] reported itchiness at simulation site, and one RCT [38] reported that no adverse events were found. For the comparator group, no adverse events were found. The remaining 4 RCTs [35][36][39][42] did not report on adverse events.
3. Conclusions
This systematic review indicates that acupressure as a sole or complementary intervention is lacking apparent advantages in the management of OA. More trials of rigorous designs are needed to further validate and overcome the limitation of current evidence.
References
- Taruc-Uy, R.L.; Lynch, S.A. Diagnosis and treatment of osteoarthritis. Prim. Care 2013, 40, 821–836.
- Wallis, J.A.; Barton, C.J.; Brusco, N.K.; Kemp, J.L.; Sherwood, J.; Young, K.; Jennings, S.; Trivett, A.; Ackerman, I.N. Exploring views of orthopaedic surgeons, rheumatologists and general practitioners about osteoarthritis management. Musculoskelet. Care 2021.
- Ng, J.Y.; Azizudin, A.M. Rheumatoid arthritis and osteoarthritis clinical practice guidelines provide few complementary and alternative medicine therapy recommendations: A systematic review. Clin. Rheumatol. 2020, 39, 2861–2873.
- Ughreja, R.A.; Prem, V. Effectiveness of Dry Needling Techniques in Patients with Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J. Bodyw. Mov. Ther. 2021.
- Choi, T.-Y.; Lee, M.S.; Kim, J.I.; Zaslawski, C. Moxibustion for the treatment of osteoarthritis: An updated systematic review and meta-analysis. Maturitas 2017, 100, 33–48.
- Lauche, R.; Hunter, D.J.; Adams, J.; Cramer, H. Yoga for osteoarthritis: A systematic review and meta-analysis. Curr. Rheumatol. Rep. 2019, 21, 47.
- Godley, E.; Smith, M.A. Efficacy of acupressure for chronic low back pain: A systematic review. Complement. Ther. Clin. Pract. 2020, 39, 101146.
- Chen, Y.W.; Wang, H.H. The effectiveness of acupressure on relieving pain: A systematic review. Pain Manag. Nurs. 2014, 15, 539–550.
- Li, T.; Li, X.; Huang, F.; Tian, Q.; Fan, Z.Y.; Wu, S. Clinical efficacy and safety of acupressure on low back pain: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2021, 2021, 8862399.
- Chen, Y.; Xiang, X.Y.; Chin, K.H.R.; Gao, J.; Wu, J.; Lao, L.; Chen, H. Acupressure for labor pain management: A systematic review and meta-analysis of randomized controlled trials. Acupunct. Med. 2020, 964528420946044.
- Najafi, F.; Jaafarpour, M.; Sayehmiri, K.; Khajavikhan, J. An Evaluation of Acupressure on the Sanyinjiao (SP6) and Hugo (LI4) Points on the Pain Severity and Length of Labor: A Systematic Review and Meta-analysis Study. Iran. J. Nurs. Midwifery Res. 2018, 23, 1–7.
- Mollart, L.J.; Adam, J.; Foureur, M. Impact of acupressure on onset of labour and labour duration: A systematic review. Women Birth 2015, 28, 199–206.
- Kwon, C.Y.; Lee, B. Clinical effects of acupressure on neck pain syndrome (nakchim): A systematic review. Integr. Med. Res. 2018, 7, 219–230.
- Hmwe, N.T.; Subramaniam, P.; Tan, L.P. Effectiveness of acupressure in promoting sleep quality: A systematic review of randomized controlled trials. Holist. Nurs. Pract. 2016, 30, 283–293.
- Waits, A.; Tang, Y.R.; Cheng, H.M.; Tai, C.J.; Chien, L.Y. Acupressure effect on sleep quality: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 37, 24–34.
- Wang, X.; Gu, J.; Liu, J.; Hong, H. Clinical evidence for acupressure with the improvement of sleep disorders in hemodialysis patients: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2020, 39, 101151.
- Chen, M.C.; Yang, L.Y.; Chen, K.M.; Hsu, H.F. Systematic review and meta-analysis on using acupressure to promote the health of older adults. J. Appl. Gerontol. 2020, 39, 1144–1152.
- Liang, Y.; Lenon, G.B.; Yang, A.W.H. Acupressure for respiratory allergic diseases: A systematic review of randomised controlled trials. Acupunct. Med. 2017, 35, 413–420.
- Liu, Y.; Tang, W.P.Y.; Gong, S.; Chan, C.W.H. A systematic review and meta-analysis of acupressure for postoperative gastrointestinal symptoms among abdominal surgery patients. Am. J. Chin. Med. 2017, 45, 1127–1145.
- Miao, J.; Liu, X.; Wu, C.; Kong, H.; Xie, W.; Liu, K. Effects of acupressure on chemotherapy-induced nausea and vomiting-a systematic review with meta-analyses and trial sequential analysis of randomized controlled trials. Int. J. Nurs. Stud. 2017, 70, 27–37.
- Abaraogu, U.O.; Igwe, S.E.; Tabansi-Ochiogu, C.S. Effectiveness of SP6 (Sanyinjiao) acupressure for relief of primary dysmenorrhea symptoms: A systematic review with meta- and sensitivity analyses. Complement. Ther. Clin. Pract. 2016, 25, 92–105.
- Jiang, H.R.; Ni, S.; Li, J.L.; Liu, M.M.; Li, J.; Cui, X.J.; Zhang, B.M. Systematic review of randomized clinical trials of acupressure therapy for primary dysmenorrhea. Evid. Based Complement. Alternative Med. 2013, 2013, 169692.
- Cho, S.H.; Hwang, E.W. Acupressure for primary dysmenorrhoea: A systematic review. Complement. Ther. Med. 2010, 18, 49–56.
- Au, D.W.; Tsang, H.W.; Ling, P.P.; Leung, C.H.; Ip, P.K.; Cheung, W.M. Effects of acupressure on anxiety: A systematic review and meta-analysis. Acupunct. Med. 2015, 33, 353–359.
- Lee, J.S.; Lee, M.S.; Min, K.; Lew, J.H.; Lee, B.J. Acupressure for treating neurological disorders: A systematic review. Int. J. Neurosci. 2011, 121, 409–414.
- Song, H.J.; Seo, H.J.; Lee, H.; Son, H.; Choi, S.M.; Lee, S. Effect of self-acupressure for symptom management: A systematic review. Complement. Ther. Med. 2015, 23, 68–78.
- Lee, E.J.; Frazier, S.K. The efficacy of acupressure for symptom management: A systematic review. J. Pain Symptom Manag. 2011, 42, 589–603.
- Kim, K.H.; Lee, M.S.; Kang, K.W.; Choi, S.M. Role of acupressure in symptom management in patients with end-stage renal disease: A systematic review. J. Palliat. Med. 2010, 13, 885–892.
- He, Y.; Guo, X.; May, B.H.; Zhang, A.L.; Liu, Y.; Lu, C.; Mao, J.J.; Xue, C.C.; Zhang, H. Clinical evidence for association of acupuncture and acupressure with improved cancer pain: A systematic review and meta-analysis. JAMA Oncol. 2020, 6, 271–278.
- Ling, W.M.; Lui, L.Y.; So, W.K.; Chan, K. Effects of acupuncture and acupressure on cancer-related fatigue: A systematic review. Oncol. Nurs. Forum 2014, 41, 581–592.
- Ernst, E. Acupuncture/acupressure for weight reduction? A systematic review. Wien. Klin. Wochenschr. 1997, 109, 60–62.
- Badiee Aval, S.; Ravanshad, Y.; Azarfar, A.; Mehrad-Majd, H.; Torabi, S.; Ravanshad, S. A systematic review and meta-analysis of using acupuncture and acupressure for uremic pruritus. Iran. J. Kidney Dis. 2018, 12, 78–83.
- Armour, M.; Ee, C.C.; Hao, J.; Wilson, T.M.; Yao, S.S.; Smith, C.A. Acupuncture and acupressure for premenstrual syndrome. Cochrane Database Syst. Rev. 2018, CD005290.
- Smith, C.A.; Collins, C.T.; Levett, K.M.; Armour, M.; Dahlen, H.G.; Tan, A.L.; Mesgarpour, B. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst. Rev. 2020, CD009232.
- Akbarnezhad, N.; Shahboulaghi, F.M.; Khankeh, H.; Sokhangouie, Y.; Biglarian, A.; Modanloo, S. The effect of acupressure therapy on pain, stiffness and physical functioning of knees among older adults diagnosed with osteoarthritis: A pilot randomized control trial. Eur. J. Integr. Med. 2019, 28, 68–75.
- Jaberi, A.A.; Norouzi, T.; Haydari, S.; Bonabi, T.N. Effect of acupressure on knee osteoarthritis symptoms in the elderly: A double-blind randomized clinical trial. Electron. Physician 2019, 11, 7489–7498.
- Li, L.W.; Harris, R.E.; Tsodikov, A.; Struble, L.; Murphy, S.L. Self-acupressure for older adults with symptomatic knee osteoarthritis: A randomized controlled trial. Arthritis Care Res. 2018, 70, 221–229.
- Zhang, Y.; Shen, C.-L.; Peck, K.; Brismée, J.-M.; Doctolero, S.; Lo, D.-F.; Lim, Y.; Lao, L. Training self-administered acupressure exercise among postmenopausal women with osteoarthritic knee pain: A feasibility study and lessons learned. Evid. Based Complement. Altern. Med. 2012, 2012.
- Rani, M.; Sharma, L.; Advani, U.; Kumar, S. Acupressure as an Adjunct to Pharmacological Treatment for Depression, Anxiety, and Stress in Patients with Knee Osteoarthritis. J. Acupunct. Meridian Stud. 2020, 13, 129–135.
- Tian, X.; Zhao, Z.; Hou, L. Clinical observation on acupoint massage combined with sodium hyaluronate in the treatment of knee osteoarthritis. Mod. J. Integrat. Trad. Chin. West. Med. 2016, 25, 2481–2483.
- Cheung, D.S.T.; Yeung, W.-F.; Lao, L. Self-administered acupressure for knee osteoarthritis in middle-aged and older adults: A pilot randomized controlled trial. J. Altern. Complement. Med. 2019, 25, A32.
- Ma, X. The research on nursing effect of TCM fumigation and acupoint massage on cervical spondylosis. Master’s Thesis, Hubei University of Chinese Medicine, Wuhan, China, 2016.




