
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Koichiro Yano | + 2233 word(s) | 2233 | 2021-04-21 09:29:43 | | | |
| 2 | Dean Liu | -10 word(s) | 2223 | 2021-04-23 03:00:21 | | | | |
| 3 | Dean Liu | -10 word(s) | 2223 | 2021-04-23 03:00:58 | | |
Video Upload Options
The concept of “joint-preservation” was introduced by Hanyu et al. in 1997. They started joint-preserving surgery to preserve the function of the MTP joints as they recognized its function as important for gait even in patients with RA.
1. Introduction
The concept of “joint-preservation” was introduced by Hanyu et al. in 1997. They started joint-preserving surgery to preserve the function of the MTP joints as they recognized its function as important for gait even in patients with RA [1]. Thus, joint-preserving surgery is defined as forefoot surgery that preserves the MTP joints. It consists of a combination of metatarsal osteotomy and soft tissue reconstruction. Bhavikatti et al. suggested that the purpose of joint-preserving surgery was not to create a normal foot, but to correct deformity, alleviate pain, and improve function [2].
2. Indications
Joint-preserving surgery is performed in patients with RA who suffer from pain and deformity of the forefoot or plantar callosities despite conservative treatment.
The indication criteria for destruction of the MTP joints vary according to previous reports and are as follow: Larsen grades 2 [3][4], 3 [5][6][1], and 4 [7][8]. The Larsen scoring system is a radiological method for grading the severity of joint destruction in patients with RA [9]. On the other hand, Hirao et al. performed joint-preserving surgery for any joint destruction, except for pencil deformities of the metatarsal head [10][11].
As for radiographic assessment, a hallux valgus angle (HVA) > 15° and intermetatarsal angle between the first and second metatarsals (IMA) > 15° [12], as well as HVA > 25° [10] and IMA > 10° [7][8] were indicated as inclusion criteria for joint-preserving surgery.
2.1. First Ray
2.1.1. Modified Scarf Osteotomy
Scarf osteotomy is a z-shaped osteotomy of the first metatarsal (Figure 1) [13]. Scarf is a carpentry term that describes the beveling of the ends of two pieces of wood such that securely fastening them creates overlap, leading to one continuous piece [14].
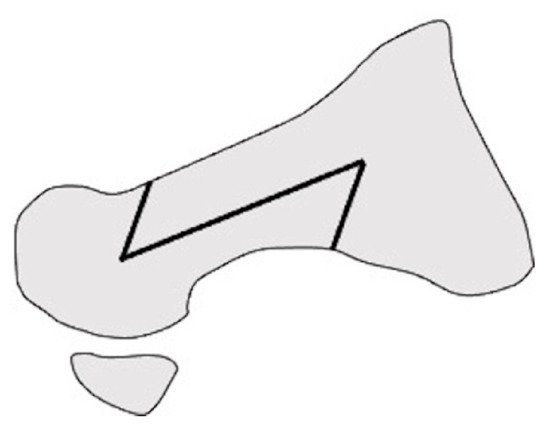
Figure 1. Scarf osteotomy in lateral view.
Barouk et al. performed the modified scarf osteotomy suggested by Maestro in which a notch was created via medial extension of the cephalic part of the osteotomy, the plantar fragment was displaced laterally, and the distal end of the proximal fragment was then fitted into the notch [15]. They reported outcomes in 55 cases of joint-preserving surgery using this modified scarf osteotomy and the Weil osteotomy for the lateral metatarsals [16]. Over an average of 6 years of follow-up, maintenance of satisfactory correction was found in 95% of the cases. There was only one case of failure which required revision surgery for arthrodesis of the first metatarsal. They emphasized that the most important component of correction was the shortening of the first metatarsal. In addition, they warned that excessive lateral translation of the distal bone fragment led to overcorrection, especially in cases with a narrow IMA [16].
Bhavikatti et al. reviewed 66 feet that underwent scarf osteotomy of the first metatarsal with a Weil osteotomy of the lesser metatarsal. Over 87% of patients subjectively reported their outcome as excellent or good, and the mean American Orthopedic Foot and Ankle Society Score (AOFAS) score increased from 39.8 to 88.7 after surgery [2].
Hirao et al. performed another modified scarf osteotomy in which the osteotomy was done parallel to the plantar aspect, and both ends of the bone fragments were partially resected (Figure 2). Moreover, an interposition technique for the medial capsule of the first MTP joint was added [10][11][17]. The medium-term outcomes in 108 cases of osteotomy indicated significant improvements on both the Japanese Society for Surgery of Foot (JSSF) scales and radiographic assessments at the last follow-up. Hallux valgus (HV) recurrence occurred in 16% of patients with relatively high preoperative IMA (average, 17.7°). The study also found that the preoperative disease activity score of RA significantly correlated with the JSSF scale and HVA at the final follow-up. This suggests that higher disease activity is associated with both clinical and radiographic outcomes [10].
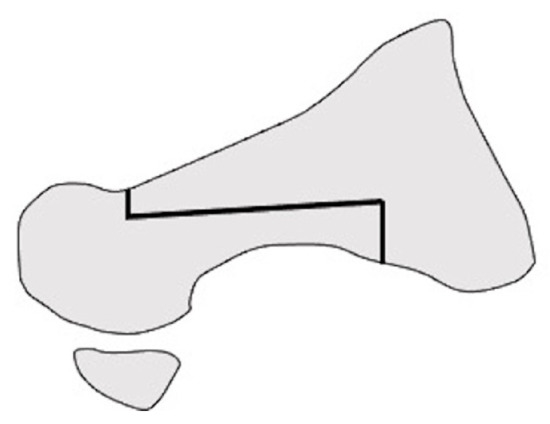
Figure 2. Modified scarf osteotomy in lateral view.
2.1.2. Lapidus Arthrodesis
Lapidus arthrodesis is the first tarsometatarsal (TMT) joint fusion procedure, introduced as a surgery for idiopathic HV in 1934 [18]. In this procedure, after osteotomy of the TMT joint, the first metatarsal is abducted to correct the HV while preserving the first MTP joint.
Shi et al. evaluated a modified Lapidus technique in 21 rheumatoid HV deformities. They described satisfactory pain relief, footwear comfort, satisfaction with the outcome of the surgery, and radiographic improvement after surgery. In addition, there was a strong correlation between splay deformity and the recurrence of HV [19].
Popelka et al. performed Lapidus arthrodesis in 143 patients with RA to treat hypermobility of the TMT joint leading to the development of HV. To assess hypermobility, they examined the preoperative anteroposterior radiographs of the weight-bearing and non-weight-bearing feet with measurement of the IMA. Moreover, weight-bearing lateral X-rays were focused on the asymmetry of the TMT joint gap [20]. Hypermobility of the TMT joint was found in 64.3% of cases. In 10 cases, after surgery, the IMA did not reduce to normal levels due to insufficient resection of the TMT joint; therefore, they suggested that appropriate bone resection is essential for positive postoperative outcomes with Lapidus arthrodesis [12].
Long-term outcomes of the modified Lapidus arthrodesis, in which the first metatarsal was abducted, shortened, and supinated after osteotomy (Figure 3), combined with proximal shortening osteotomy of the lesser metatarsals, were reported by Niki et al. [5]. The surgery was performed on 57 RA patients in clinical remission, with an average of 76.6 months of follow-up. The JSSF score and radiographic assessments significantly improved at the last follow-up. No patient experienced obvious recurrence of the deformity or symptomatic callus formation. They suggested that one of the advantages of Lapidus arthrodesis is that correction loss due to postoperative changes in TMT joint alignment can be avoided [5][6].
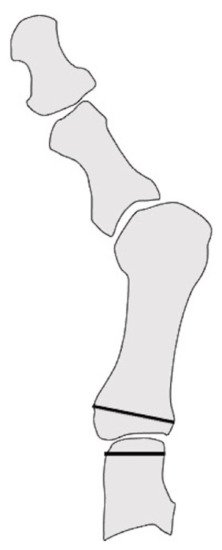
Figure 3. Modified Lapidus arthrodesis in anteroposterial view.
2.1.3. Proximal Rotational Closing-Wedge Osteotomy
Authors in this article developed proximal rotational closing-wedge osteotomy of the first metatarsal, in which the distal aspect of the wedge was vertical to the axis of the first metatarsal (Figure 4). The benefits of the osteotomy are as follows: (1) large correction due to proximal osteotomy; (2) correction of the pronation deformity of the first metatarsal by supinating the distal fragment of the first metatarsal; (3) easy shortening of the first metatarsal according to the amount of shortening of the lesser metatarsals; and (4) easy correction as planned preoperatively by placing osteotomy surfaces in contact without fluoroscopy [7][8].
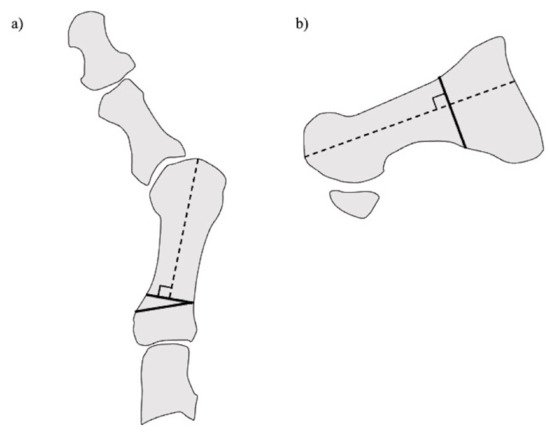
Figure 4. Proximal rotational closing-wedge osteotomy. (a) Anteroposterial view. (b) Lateral view.
We assessed the long-term outcomes, including patient-reported outcome measures and radiographic evaluations, of proximal rotational closing-wedge osteotomy in 105 rheumatoid feet with a minimum follow-up of 5 years. Patient-reported outcome measures were evaluated using the self-administered foot evaluation questionnaire (SAFE-Q). All SAFE-Q subscales and radiographic values improved significantly over an average follow-up of 6 years. Recurrence of HV occurred in 10.5% of cases. The estimated survivorship of joint-preserving surgery with proximal rotational closing-wedge osteotomy of the first metatarsal and shortening oblique osteotomies of the lesser toes, at 7 years, with reoperation as the endpoint, was 89.5% (Figure 5) [8].
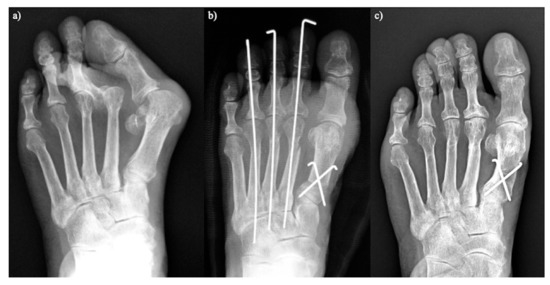
Figure 5. Proximal rotational closing-wedge osteotomy. (a) Preoperative. (b) Two weeks after surgery. (c) Five years after surgery.
2.1.4. Other Osteotomies
Thordarson et al. performed chevron osteotomy in 13 cases with well-preserved joint space and no active preoperative signs of inflammation, but approximately 85% of cases developed a HV deformity again or inflammatory erosions, with an average time to failure of 2 years [21].
Nagashima et al. reported the outcomes of a modified Hohmann osteotomy [22] combined with a Helal osteotomy [23] in the lesser toes of 47 rheumatoid feet. They reported that HVA and IMA improved significantly at final follow-up, and all patients were satisfied with the modified Hohmann procedure [3].
Takakubo et al. used a modified Mann method in 11 cases that combined proximal osteotomy of the first metatarsal and soft tissue reconstruction. The procedure showed satisfactory clinical and radiographic outcomes. Joint degeneration scores of the first MTP joint as per the modified Sharp methods [24] and Larsen grades [9] were also examined. Only the postoperative joint space narrowing score showed a slight decline. Although the recurrence of HV involving a HVA of more than 25° was relatively high (27%), this may be due to the small number of cases [25].
Chao et al. performed several osteotomies (Ludloff, scarf, and chevron) to preserve the first MTP joint in 37 rheumatoid feet. The AOFAS and visual analogue scale (VAS) pain scores improved significantly in this series. In contrast to Takakubo et al. [25], the joint degeneration scores of the first MTP increased postoperatively.
Jo et al. compared a fixation technique involving the modified Ludloff osteotomy using two screws with a plate augmentation along with two screws in 31 rheumatoid feet. Correction loss at the osteotomy site occurred only in patients who underwent fixation with two screws, without the plate [4].
2.2. Lateral Rays
Most osteotomies of the lesser metatarsals aim to shorten the metatarsal and elevate the metatarsal head dorsally. This shortening enables correction of the dorsally dislocated lesser toes, and elevation reduces the risk of callosity recurrence.
2.2.1. Shortening Oblique Osteotomy of the Metatarsal Neck
Shortening oblique osteotomy (SOO) of the metatarsal neck was first performed by Hanyu et al. in 1997 (Figure 6). Although a simple oblique osteotomy of the metatarsal neck had been developed by Helal et al. [23], Hanyu et al. modified it by cutting the metatarsal neck twice in a parallel manner to shorten metatarsal length and to elevate the metatarsal head. After correcting the dislocation of the MTP joints of the lesser toes, the joints and osteotomy sites were temporarily fixed using a single Kirschner wire (K-wire) [1]. We have reported satisfactory short- and long-term outcomes after SOO with a modification involving a ligature around bone fragments to hold them together to avoid nonunion or malunion along with proximal rotational closing-wedge osteotomy of the first metatarsal [7][8][26]. Horita et al. fixed the osteotomy site with a screw instead of a K-wire and described good clinical outcomes with SOO [27].
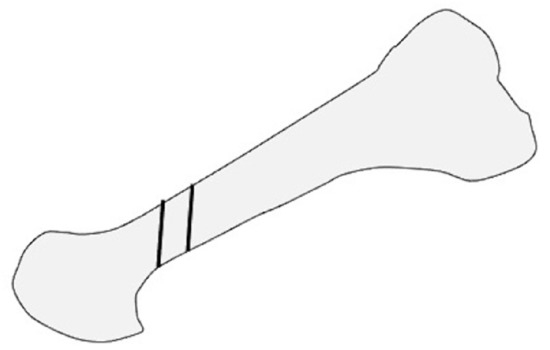
Figure 6. Shortening oblique osteotomy of the lesser metatarsal in lateral view.
2.2.2. Weil Osteotomy
Weil osteotomy is cut from the dorsal surface of the metatarsal head to the proximal plantar surface along the metatarsal shaft, while attempting to be parallel to the ground, which allows a fixed amount of shortening of the metatarsal (Figure 7). After shortening was completed, a screw was used to fix the two fragments [28][29].
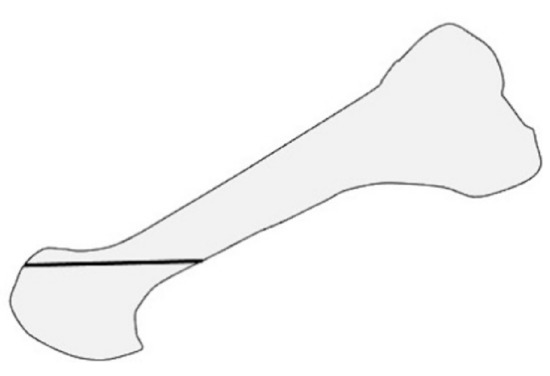
Figure 7. Weil osteotomy of the lesser metatarsal in lateral view.
Barouk et al. modified Weil osteotomy by additional removal of a thin trapezoidal bone to elevate the plantar aspect of the metatarsal head. For preoperative assessment, they set the metatarsal shortening point (MS point), which is the location of the most proximal part of the base of the proximal phalanx of the most impaired ray. The amount of metatarsal shortening was determined as the distance between the MS point and the distal end of the metatarsal head. In their study, average shortening amounted to 13 mm. This study described failed joint preservation of the lesser MTP joint, resulting in secondary surgery occurring in only 2% of all cases. They suggested that the shortening should reach the MS point to achieve successful correction of the deformities [16].
Bhavikatti et al. examined 66 feet that underwent joint-preserving surgery combined with a scarf osteotomy of the first ray and Weil osteotomy of the lesser metatarsal. As described above, the patients showed good clinical and radiographic results [2].
2.2.3. Offset Osteotomy
Offset osteotomy involves shortening of the metatarsal bone and shifting the metatarsal head medially for lesser MTP joint deformities, as reported by Owaki et al. in 2003. After the osteotomy, two notches were made in the cortical bone at the distal end of the proximal stump. The proximal end of the metatarsal head was inserted into the notch to achieve shortening and shifting of the lesser metatarsals [30].
Hirao et al. changed the direction of shift of each metatarsal head to reconstruct the transverse arch (Figure 8). This modified offset osteotomy showed satisfactory clinical and radiographic outcomes in 80 patients with rheumatoid forefoot deformities. Recurrence of dorsal dislocation and subluxation of the lesser MTP joints occurred in some cases. In the recurrence group, 67% showed varus hindfoot preoperatively, and most of the preoperative valgus hindfoot cases involved midfoot ankyloses. They suggested that surgeons had to consider the possibility of recurrence of lesser MTP joint deformities in cases of varus hindfoot and midfoot ankyloses [31].
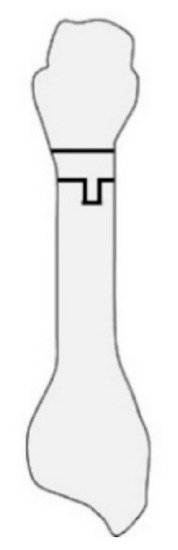
Figure 8. Offset osteotomy of the lesser metatarsal in anteroosterial view.
2.2.4. Proximal Oblique Shortening Osteotomy
Niki et al. developed shortening oblique osteotomies of the bases of the second, third, and fourth metatarsals combined with a modified Lapidus arthrodesis of the first TMT joint and a modified Coughlin osteotomy of the fifth metatarsal. Oblique osteotomy was performed at an angle of 30° to the longitudinal axis of the metatarsal (Figure 9). After the distal fragment was displaced dorsally and proximally to shorten and elevate the metatarsal, the osteotomy site was fixed using a screw. No obvious recurrence of deformity or symptomatic callosity occurred after surgery in 57 cases [5].
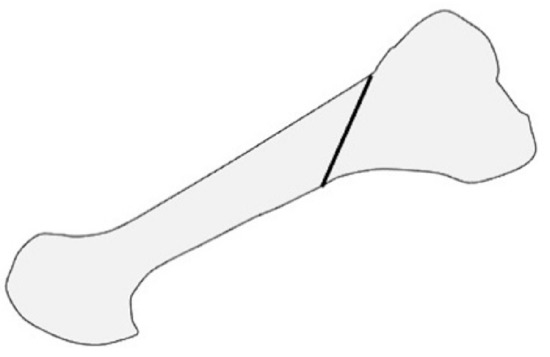
Figure 9. Proximal oblique shortening osteotomy of the lesser metatarsal in lateral view.
2.3. Post-Operative Protocol
The time at which weight-bearing is started varies according to past reports: heel gait immediately after surgery [16][7], heel gait 1 week after surgery [4], full weight-bearing two or three weeks after surgery [3][25][1][11], partial weight-bearing 3 weeks after surgery [5][6], and full weight-bearing 6 weeks after surgery [2][12]. Most authors allowed patients to wear an orthosis or a specific shoe during walking.
K-wires inserted from the toes to fix the osteotomy site of the lesser metatarsals were usually removed 3 weeks after surgery [5][6][25][7][1]. Hirao et al. found that early introduction of range of motion (ROM) exercises following the removal of K-wires 2 weeks after surgery increased the ROM of the lesser toes 6 months after surgery, when compared to the non-exercise group [32].
References
- Hanyu, T.; Yamazaki, H.; Murasawa, A.; Tohyama, C. Arthroplasty for rheumatoid forefoot deformities by a shortening oblique osteotomy. Clin. Orthop. Relat. Res. 1997, 338, 131–138.
- Bhavikatti, M.; Sewell, M.D.; Al-Hadithy, N.; Awan, S.; Bawarish, M.A. Joint preserving surgery for rheumatoid forefoot deformities improves pain and corrects deformity at midterm follow-up. Foot 2012, 22, 81–84.
- Nagashima, M.; Kato, K.; Miyamoto, Y.; Takenouchi, K. A modified Hohmann method for hallux valgus and telescoping osteotomy for lesser toe deformities in patients with rheumatoid arthritis. Clin. Rheumatol. 2007, 26, 748–752.
- Jo, Y.H.; Park, K.C.; Song, Y.S.; Sung, I.H. Comparison of outcomes according to fixation technique following the modified Ludloff osteotomy for hallux valgus in patients with rheumatoid arthritis. BMC Musculoskelet Disord 2017, 18, 371.
- Niki, H.; Hirano, T.; Akiyama, Y.; Mitsui, H.; Fujiya, H. Long-term outcome of joint-preserving surgery by combination metatarsal osteotomies for shortening for forefoot deformity in patients with rheumatoid arthritis. Mod. Rheumatol. 2015, 25, 683–688.
- Niki, H.; Hirano, T.; Okada, H.; Beppu, M. Combination joint-preserving surgery for forefoot deformity in patients with rheumatoid arthritis. J. Bone Jt. Surg. Br. 2010, 92, 380–386.
- Yano, K.; Ikari, K.; Iwamoto, T.; Saito, A.; Naito, Y.; Kawakami, K.; Suzuki, T.; Imamura, H.; Sakuma, Y.; Hiroshima, R.; et al. Proximal rotational closing-wedge osteotomy of the first metatarsal in rheumatoid arthritis: Clinical and radiographic evaluation of a continuous series of 35 cases. Mod. Rheumatol. 2013, 23, 953–958.
- Yano, K.; Ikari, K.; Tobimatsu, H.; Okazaki, K. Patient-Reported and Radiographic Outcomes of Joint-Preserving Surgery for Rheumatoid Forefoot Deformities: A Retrospective Case Series with Mean Follow-up of 6 Years. J. Bone Jt. Surg. Am. 2021.
- Larsen, A.; Dale, K.; Eek, M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol. Diagn. 1977, 18, 481–491.
- Kushioka, J.; Hirao, M.; Tsuboi, H.; Ebina, K.; Noguchi, T.; Nampei, A.; Tsuji, S.; Akita, S.; Hashimoto, J.; Yoshikawa, H. Modified Scarf Osteotomy with Medial Capsule Interposition for Hallux Valgus in Rheumatoid Arthritis: A Study of Cases Including Severe First Metatarsophalangeal Joint Destruction. J. Bone Jt. Surg. Am. 2018, 100, 765–776.
- Hirao, M.; Ebina, K.; Tsuboi, H.; Nampei, A.; Tsuji, S.; Noguchi, T.; Owaki, H.; Yoshikawa, H.; Hashimoto, J. Modified Scarf Osteotomy with Medial Capsular Interposition in Great Toe and Metatarsal Shortening Offset Osteotomy in Lesser Toes for Rheumatoid Deformity. JBJS Essent. Surg. Tech. 2018, 8, e27.
- Popelka, S.; Hromadka, R.; Vavrik, P.; Bartak, V.; Popelka, S., Jr.; Sosna, A. Hypermobility of the first metatarsal bone in patients with rheumatoid arthritis treated by Lapidus procedure. BMC Musculoskelet. Disord. 2012, 13, 148.
- Weil, L.S. Scarf osteotomy for correction of hallux valgus. Historical perspective, surgical technique, and results. Foot Ankle Clin. 2000, 5, 559–580.
- Molloy, A.; Widnall, J. Scarf osteotomy. Foot Ankle Clin. 2014, 19, 165–180.
- Leemrijse, T.; Maestro, M.; Tribak, K.; Gombault, V.; Devos Bevernage, B.; Deleu, P.A. Scarf osteotomy without internal fixation to correct hallux valgus. Orthop. Traumatol. Surg. Res. Otsr 2012, 98, 921–927.
- Barouk, L.S.; Barouk, P. Joint-preserving surgery in rheumatoid forefoot: Preliminary study with more-than-two-year follow-up. Foot Ankle Clin. 2007, 12, 435–454.
- Ebina, K.; Hirao, M.; Tsuboi, H.; Kaneshiro, S.; Nishikawa, M.; Goshima, A.; Noguchi, T.; Nakaya, H.; Etani, Y.; Miyama, A.; et al. Impact of combining medial capsule interposition with modified scarf osteotomy for hallux valgus. Mod. Rheumatol. 2020, 30, 204–210.
- Lapidus, P.W. The author’s bunion operation from 1931 to 1959. Clin. Orthop. 1960, 16, 119–135.
- Shi, K.; Hayashida, K.; Tomita, T.; Tanabe, M.; Ochi, T. Surgical treatment of hallux valgus deformity in rheumatoid arthritis: Clinical and radiographic evaluation of modified Lapidus technique. J. Foot Ankle Surg. 2000, 39, 376–382.
- Coughlin, M.J.; Jones, C.P. Hallux valgus and first ray mobility. A prospective study. J. Bone Jt. Surg. Am. 2007, 89, 1887–1898.
- Thordarson, D.B.; Aval, S.; Krieger, L. Failure of hallux MP preservation surgery for rheumatoid arthritis. Foot Ankle Int. 2002, 23, 486–490.
- Christensen, P.H.; Hansen, T.B. Hallux valgus correction using a modified Hohmann technique. Foot Ankle Int. 1995, 16, 177–180.
- Helal, B.; Greiss, M. Telescoping osteotomy for pressure metatarsalgia. J. Bone Jt. Surg. Br. 1984, 66, 213–217.
- Sharp, J.T.; Bluhm, G.B.; Brook, A.; Brower, A.C.; Corbett, M.; Decker, J.L.; Genant, H.K.; Gofton, J.P.; Goodman, N.; Larsen, A.; et al. Reproducibility of multiple-observer scoring of radiologic abnormalities in the hands and wrists of patients with rheumatoid arthritis. Arthritis Rheum. 1985, 28, 16–24.
- Takakubo, Y.; Takagi, M.; Tamaki, Y.; Sasaki, A.; Nakano, H.; Orui, H.; Ogino, T. Mid-term results of joint-preserving procedures by a modified Mann method for big toe deformities in rheumatoid patients undergoing forefoot surgeries. Mod. Rheumatol. 2010, 20, 147–153.
- Yano, K.; Ikari, K.; Ishibashi, M.; Momohara, S. Preventing delayed union after distal shortening oblique osteotomy of metatarsals in the rheumatoid forefoot. Mod. Rheumatol. 2016, 26, 546–550.
- Horita, M.; Nishida, K.; Hashizume, K.; Nasu, Y.; Saiga, K.; Nakahara, R.; Machida, T.; Ohashi, H.; Ozaki, T. Outcomes of Resection and Joint-Preserving Arthroplasty for Forefoot Deformities for Rheumatoid Arthritis. Foot Ankle Int. 2018, 39, 292–299.
- Vandeputte, G.; Dereymaeker, G.; Steenwerckx, A.; Peeraer, L. The Weil osteotomy of the lesser metatarsals: A clinical and pedobarographic follow-up study. Foot Ankle Int. 2000, 21, 370–374.
- Trnka, H.J.; Muhlbauer, M.; Zettl, R.; Myerson, M.S.; Ritschl, P. Comparison of the results of the Weil and Helal osteotomies for the treatment of metatarsalgia secondary to dislocation of the lesser metatarsophalangeal joints. Foot Ankle Int. 1999, 20, 72–79.
- Owaki, H.; Hashimoto, J.; Hayashida, K.; Hashimoto, H.; Ochi, T.; Yoshikawa, H. Short term result of metatarsal realignment for rheumatoid forefoot deformities by metatarsal shortening offset osteotomy. Orthop. Proc. 2003, 85, 80.
- Hirao, M.; Ebina, K.; Tsuboi, H.; Nampei, A.; Kushioka, J.; Noguchi, T.; Tsuji, S.; Owaki, H.; Hashimoto, J.; Yoshikawa, H. Outcomes of modified metatarsal shortening offset osteotomy for forefoot deformity in patients with rheumatoid arthritis: Short to mid-term follow-up. Mod. Rheumatol. 2017, 27, 981–989.
- Hirao, M.; Tsuboi, H.; Tazaki, N.; Kushimoto, K.; Ebina, K.; Yoshikawa, H.; Hashimoto, J. Effects of range of motion exercise of the metatarsophalangeal joint from 2-weeks after joint-preserving rheumatoid forefoot surgery. Mod. Rheumatol. 2020, 30, 305–312.




